Abstract
Purpose
Drug elimination alteration has been well reported in acute lymphoblastic leukemia (ALL). Considering that transporters and glomerular filtration influence, to different extents, the drug disposition, and possible side effects, we evaluated the effects of ALL on major renal transporters and glomerular filtration mediated pharmacokinetic changes, as well as expression of renal drug transporters.
Methods
ALL xenograft models were established and intravenously injected with substrates of renal transporters and glomerular filtration separately in NOD/SCID mice. The plasma concentrations of substrates, after single doses, were determined using high-performance liquid chromatography-tandem mass spectrometry (HPLC-MS/MS).
Results
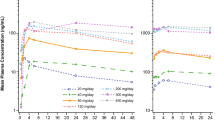
With the development of ALL, protein expression of MDR1, OAT3 and OCT2 were increased by 2.62-fold, 1.70-fold, and 1.45-fold, respectively, whereas expression of MRP2 and MRP4 were significantly decreased by 30.98% and 45.28% in the kidney of ALL groups compared with control groups. Clearance of MDR1-mediated digoxin, OAT3-mediated furosemide, and OCT2-mediated metformin increased by 3.04-fold, 1.47-fold, and 1.26-fold, respectively. However, clearance of MRPs-mediated methotrexate was reduced by 39.5%. These results are consistent with mRNA expression. Clearance of vancomycin and amikacin, as markers of glomerular filtration rate, had a 2.14 and 1.64-fold increase in ALL mice, respectively.
Conclusions
The specific alteration of renal transporters and glomerular filtration in kidneys provide a rational explanation for changes in pharmacokinetics for ALL.



Similar content being viewed by others
Abbreviations
- ABC:
-
ATP-binding cassette
- ALL:
-
Acute lymphoblastic leukemia
- AML:
-
Acute myeloid leukemia
- BCRP:
-
Breast cancer resistance protein
- CL:
-
Clearance
- GFR:
-
Glomerular filtration ratio
- MDR:
-
Multidrug resistance
- MRPs:
-
Multidrug resistance proteins
- OATs:
-
Organic anion transporters
- OCTs:
-
Organic cation transporters
- PK:
-
Pharmacokinetics
- SLC:
-
Solute carrier
- TRM:
-
Treatment-related mortality
References
Teachey DT, O'Connor D. How I treat newly diagnosed T-cell acute lymphoblastic leukemia (T-ALL) and T-cell lymphoblastic lymphoma in children. Blood. 2019.
Li B, Brady SW, Ma X, Shen S, Zhang Y, Li Y, et al. Therapy-induced mutations drive the genomic landscape of relapsed acute lymphoblastic leukemia. Blood. 2019.
Pea F, Viale P, Candoni A, Pavan F, Pagani L, Damiani D, et al. Teicoplanin in patients with acute leukaemia and febrile neutropenia: a special population benefiting from higher dosages. Clin Pharmacokinet. 2004;43(6):405–15.
Dong L, Zhai XY, Yang YL, Wang L, Zhou Y, Shi HY, et al. Population pharmacokinetics and dosing optimization of imipenem in children with hematological malignancies. Antimicrob Agents Chemother. 2019;63(6).
Zhao W, Zhang D, Fakhoury M, Fahd M, Duquesne F, Storme T, et al. Population pharmacokinetics and dosing optimization of vancomycin in children with malignant hematological disease. Antimicrob Agents Chemother. 2014;58(6):3191–9.
Konig J, Muller F, Fromm MF. Transporters and drug-drug interactions: important determinants of drug disposition and effects. Pharmacol Rev. 2013;65(3):944–66.
Ivanyuk A, Livio F, Biollaz J, Buclin T. Renal drug transporters and drug interactions. Clin Pharmacokinet. 2017;56(8):825–92.
Evers R, Piquette-Miller M, Polli JW, Russel FGM, Sprowl JA, Tohyama K, et al. Disease-associated changes in drug transporters may impact the pharmacokinetics and/or toxicity of drugs: a white paper from the international transporter consortium. Clin Pharmacol Ther. 2018;104(5):900–15.
Liu T, Meng Q, Wang C, Liu Q, Guo X, Sun H, et al. Changes in expression of renal Oat1, Oat3 and Mrp2 in cisplatin-induced acute renal failure after treatment of JBP485 in rats. Toxicol Appl Pharmacol. 2012;264(3):423–30.
Nowicki MT, Aleksunes LM, Sawant SP, Dnyanmote AV, Mehendale HM, Manautou JE. Renal and hepatic transporter expression in type 2 diabetic rats. Drug Metab Lett. 2008;2(1):11–7.
Laouari D, Yang R, Veau C, Blanke I, Friedlander G. Two apical multidrug transporters, P-gp and MRP2, are differently altered in chronic renal failure. Am J Physiol Renal Physiol. 2001;280(4):F636–45.
Lee MW, Kim HJ, Yoo KH, Kim DS, Yang JM, Kim HR, et al. Establishment of a bioluminescent imaging-based in vivo leukemia model by intra-bone marrow injection. Int J Oncol. 2012;41(6):2047–56.
Li X, Wang Y, Zhou Q, Yu Y, Chen L, Zheng J. A sensitive method for digoxin determination using formate-adduct ion based on the effect of ionization enhancement in liquid chromatograph-mass spectrometer. J Chromatogr B Analyt Technol Biomed Life Sci. 2015;978–979:138–44.
Guo P, Wang X, Liu L, Belinsky MG, Kruh GD, Gallo JM. Determination of methotrexate and its major metabolite 7-hydroxymethotrexate in mouse plasma and brain tissue by liquid chromatography-tandem mass spectrometry. J Pharm Biomed Anal. 2007;43(5):1789–95.
Macwan JS, Ionita IA, Akhlaghi F. A simple assay for the simultaneous determination of rosuvastatin acid, rosuvastatin-5S-lactone, and N-desmethyl rosuvastatin in human plasma using liquid chromatography-tandem mass spectrometry (LC-MS/MS). Anal Bioanal Chem. 2012;402(3):1217–27.
Shi J, Hu Y, Smith DE, Zhu HJ. A sensitive liquid chromatography-tandem mass spectrometry method for the quantification of valacyclovir and its metabolite acyclovir in mouse and human plasma. J Chromatogr B Analyt Technol Biomed Life Sci. 2018;1092:447–52.
Marques MA, Soares Ade S, Pinto OW, Barroso PT, Pinto DP, Ferreira-Filho M, et al. Simple and rapid method determination for metformin in human plasma using high performance liquid chromatography tandem mass spectrometry: application to pharmacokinetic studies. J Chromatogr B Analyt Technol Biomed Life Sci. 2007;852(1–2):308–16.
Gajula R, Pilli NR, Ravi VB, Maddela R, Inamadugu JK, Polagani SR, et al. Simultaneous determination of atorvastatin and aspirin in human plasma by LC-MS/MS: its pharmacokinetic application. Sci Pharm. 2012;80(4):923–40.
Cheng C, Liu S, Xiao D, Hollembaek J, Yao L, Lin J, et al. LC-MS/MS method development and validation for the determination of polymyxins and vancomycin in rat plasma. J Chromatogr B Analyt Technol Biomed Life Sci. 2010;878(28):2831–8.
Dijkstra JA, Sturkenboom MG, Hateren K, Koster RA, Greijdanus B, Alffenaar JW. Quantification of amikacin and kanamycin in serum using a simple and validated LC-MS/MS method. Bioanalysis. 2014;6(16):2125–33.
Dostalek M, Akhlaghi F, Puzanovova M. Effect of diabetes mellitus on pharmacokinetic and pharmacodynamic properties of drugs. Clin Pharmacokinet. 2012;51(8):481–99.
Zamek-Gliszczynski MJ, Lee CA, Poirier A, Bentz J, Chu X, Ellens H, et al. ITC recommendations for transporter kinetic parameter estimation and translational modeling of transport-mediated PK and DDIs in humans. Clin Pharmacol Ther. 2013;94(1):64–79.
International Transporter C, Giacomini KM, Huang SM, Tweedie DJ, Benet LZ, Brouwer KL, et al. Membrane transporters in drug development. Nat Rev Drug Discov. 2010;9(3):215–36.
Diekjurgen D, Grainger DW. Drug transporter expression profiling in a three-dimensional kidney proximal tubule in vitro nephrotoxicity model. Pflugers Arch. 2018;470(9):1311–23.
Mehrvar N, Abolghasemi H, Rezvany MR, Akbari ME, Saberynejad J, Mehrvar A, et al. Characterizing Iranian pediatric patients with relapsed acute lymphoblastic leukemia through gene expression profiling of common ATP binding cassette transporters subfamily C. J Pediatr Hematol Oncol. 2020;42(1):41–5.
Heemskerk S, Peters JG, Louisse J, Sagar S, Russel FG, Masereeuw R. Regulation of P-glycoprotein in renal proximal tubule epithelial cells by LPS and TNF-alpha. J Biomed Biotechnol. 2010;2010:525180.
Hu M, Liu Y, Deng C, Han R, Jia Y, Liu S, et al. Enhanced invasiveness in multidrug resistant leukemic cells is associated with overexpression of P-glycoprotein and cellular inhibitor of apoptosis protein. Leuk Lymphoma. 2011;52(7):1302–11.
Kunin M, Holtzman EJ, Melnikov S, Dinour D. Urinary organic anion transporter protein profiles in AKI. Nephrol Dial Transplant. 2012;27(4):1387–95.
Yoshizawa K, Ikawa K, Ikeda K, Ohge H, Morikawa N. Population pharmacokinetic-pharmacodynamic target attainment analysis of imipenem plasma and urine data in neonates and children. Pediatr Infect Dis J. 2013;32(11):1208–16.
Sime FB, Roberts MS, Warner MS, Hahn U, Robertson TA, Yeend S, et al. Altered pharmacokinetics of piperacillin in febrile neutropenic patients with hematological malignancy. Antimicrob Agents Chemother. 2014;58(6):3533–7.
Gai Z, Visentin M, Hiller C, Krajnc E, Li T, Zhen J, et al. Organic Cation transporter 2 overexpression may confer an increased risk of gentamicin-induced nephrotoxicity. Antimicrob Agents Chemother. 2016;60(9):5573–80.
Bertino JS Jr, Booker LA, Franck P, Rybicki B. Gentamicin pharmacokinetics in patients with malignancies. Antimicrob Agents Chemother. 1991;35(7):1501–3.
Zhao W, Biran V, Jacqz-Aigrain E. Amikacin maturation model as a marker of renal maturation to predict glomerular filtration rate and vancomycin clearance in neonates. Clin Pharmacokinet. 2013;52(12):1127–34.
Romano S. Fdez de Gatta MM, Calvo MV, caballero D, Dominguez-Gil a, Lanao JM. Population pharmacokinetics of amikacin in patients with haematological malignancies. J Antimicrob Chemother. 1999;44(2):235–42.
Zeitany RG, El Saghir NS, Santhosh-Kumar CR, Sigmon MA. Increased aminoglycoside dosage requirements in hematologic malignancy. Antimicrob Agents Chemother. 1990;34(5):702–8.
Davis RL, Lehmann D, Stidley CA, Neidhart J. Amikacin pharmacokinetics in patients receiving high-dose cancer chemotherapy. Antimicrob Agents Chemother. 1991;35(5):944–7.
Hjorth L, Wiebe T, Karpman D. Hyperfiltration evaluated by glomerular filtration rate at diagnosis in children with cancer. Pediatr Blood Cancer. 2011;56(5):762–6.
Chu X, Galetin A, Zamek-Gliszczynski MJ, Zhang L, Tweedie DJ, International Transporter C. Dabigatran Etexilate and digoxin: comparison as clinical probe substrates for evaluation of P-gp inhibition. Clin Pharmacol Ther. 2018;104(5):788–92.
El-Sheikh AA, Greupink R, Wortelboer HM, van den Heuvel JJ, Schreurs M, Koenderink JB, et al. Interaction of immunosuppressive drugs with human organic anion transporter (OAT) 1 and OAT3, and multidrug resistance-associated protein (MRP) 2 and MRP4. Transl Res. 2013;162(6):398–409.
Momper JD, Tsunoda SM, Ma JD. Evaluation of proposed in vivo probe substrates and inhibitors for Phenotyping transporter activity in humans. J Clin Pharmacol. 2016;56(Suppl 7):S82–98.
ACKNOWLEDGMENTS AND DISCLOSURES
This work was supported by National Science and Technology Major Projects for “Major New Drugs Innovation and Development” (2017ZX09304029-002), National Science Foundation of China (81703603), Young Taishan Scholars Program of Shandong Province, Qilu Young Scholars Program of Shandong University.
Author information
Authors and Affiliations
Corresponding authors
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Zhou, Y., Du, B., Kan, M. et al. Drug Elimination Alteration in Acute Lymphoblastic Leukemia Mediated by Renal Transporters and Glomerular Filtration. Pharm Res 37, 158 (2020). https://doi.org/10.1007/s11095-020-02896-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11095-020-02896-8