Abstract
Purpose
This study aimed to investigate the potential pharmacokinetic interactions between curcumin, imatinib and bosutinib, combining In Vitro and in silico methods.
Methods
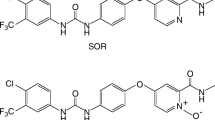
In Vitro metabolism of imatinib and bosutinib were investigated in pooled human liver microsomes and recombinant CYP3A4 enzyme in the presence and absence of curcumin and curcumin glucuronide using an LC-MS/MS assay for N-desmethyl metabolites. A physiologically-based pharmacokinetic (PBPK) model for curcumin formulated as solid lipid nanoparticles (SLN) was constructed using In Vitro glucuronidation kinetics and published clinical pharmacokinetic data. The potential effects of curcumin coadministration on systemic exposures of imatinib and bosutinib were predicted in silico using PBPK simulations.
Results
Curcumin demonstrated potent reversible inhibition of cytochrome P450 (CYP)3A4-mediated N-demethylation of imatinib and bosutinib and CYP2C8-mediated metabolism of imatinib with inhibitory constants (ki,u) of ≤1.5 μmol. L−1. A confirmatory In Vitro study with paclitaxel, the 6α-hydroxylation of which is exclusively mediated by CYP2C8, was consistent with a potent inhibition of this enzyme by curcumin. Curcumin glucuronide also inhibited both CYP enzymes In Vitro, albeit to a lesser extent than that of curcumin. PBPK model simulations predicted that at recommended dosing regimens of SLN curcumin, coadministration would result in an increase in systemic exposures of imatinib and bosutinib of up to only 10%.
Conclusion
A PBPK model for curcumin in a SLN formulation was successfully developed. Although curcumin possesses a strong In Vitro inhibitory activity towards CYP3A4 and CYP2C8 enzymes, its interactions with imatinib and bosutinib were unlikely to be of clinical importance due to curcumin’s poor bioavailability.







Similar content being viewed by others
Abbreviations
- AUC:
-
Area under the plasma concentration-time curve
- CML:
-
Chronic myeloid leukaemia
- CYP:
-
Cytochrome P450
- fuinc :
-
Unbound fraction during incubation
- HIM:
-
Human intestinal microsomes
- HLM:
-
Human liver microsomes
- IVIVE:
-
In Vitro to In Vivo extrapolation
- ki :
-
Inhibitory constant
- M5:
-
N-desmethyl bosutinib
- NDMI:
-
N-desmethyl imatinib
- PBPK:
-
Physiologically-based pharmacokinetic
- POR:
-
P450 reductase
- rCYP3A4:
-
Recombinant human CYP3A4 enzyme
- SLN:
-
Solid lipid nanoparticles
- SULT:
-
Sulphotransferase
- UGT:
-
Uridine 5′-diphospho-glucuronosyltransferase
References
Hochhaus A, Larson RA, Guilhot F, Radich JP, Branford S, Hughes TP, et al. Long-term outcomes of imatinib treatment for chronic myeloid leukemia. N Engl J Med. 2017;376(10):917–27.
Cortes JE, Gambacorti-Passerini C, Deininger MW, Mauro MJ, Chuah C, Kim DW, et al. Bosutinib versus imatinib for newly diagnosed chronic myeloid leukemia: results from the randomized BFORE trial. J Clin Oncol. 2018;36(3):231–7.
Fleischer T, Chang TT, Chiang JH, Chang CM, Hsieh CY, Yen HR. Adjunctive Chinese herbal medicine therapy improves survival of patients with chronic myeloid leukemia: a nationwide population-based cohort study. Cancer Med. 2016;5(4):640–8.
Roe AL, Paine MF, Gurley BJ, Brouwer KR, Jordan S, Griffiths JC. Assessing natural product-drug interactions: an end-to-end safety framework. Regul Toxicol Pharmacol. 2016;76:1–6.
Salehi B, Stojanovic-Radic Z, Matejic J, Sharifi-Rad M, Anil Kumar NV, Martins N, et al. The therapeutic potential of curcumin: a review of clinical trials. Eur J Med Chem. 2019;163:527–45.
Adiwidjaja J, McLachlan AJ, Boddy AV. Curcumin as a clinically-promising anti-cancer agent: pharmacokinetics and drug interactions. Expert Opin Drug Metab Toxicol. 2017;13(9):953–72.
Johnson EJ, Gonzalez-Perez V, Tian DD, Lin YS, Unadkat JD, Rettie AE, et al. Selection of priority natural products for evaluation as potential precipitants of natural product-drug interactions: a NAPDI center recommended approach. Drug Metab Dispos. 2018;46(7):1046–52.
Kusuhara H, Furuie H, Inano A, Sunagawa A, Yamada S, Wu C, et al. Pharmacokinetic interaction study of sulphasalazine in healthy subjects and the impact of curcumin as an In Vivo inhibitor of BCRP. Br J Pharmacol. 2012;166(6):1793–803.
Lee CA, O'Connor MA, Ritchie TK, Galetin A, Cook JA, Ragueneau-Majlessi I, et al. Breast cancer resistance protein (ABCG2) in clinical pharmacokinetics and drug interactions: practical recommendations for clinical victim and perpetrator drug-drug interaction study design. Drug Metab Dispos. 2015;43(4):490–509.
Volak LP, Hanley MJ, Masse G, Hazarika S, Harmatz JS, Badmaev V, et al. Effect of a herbal extract containing curcumin and piperine on midazolam, flurbiprofen and paracetamol (acetaminophen) pharmacokinetics in healthy volunteers. Br J Clin Pharmacol. 2013;75(2):450–62.
Hussaarts K, Hurkmans DP, Oomen-de Hoop E, van Harten LJ, Berghuis S, van Alphen RJ, et al. Impact of curcumin (with or without piperine) on the pharmacokinetics of tamoxifen. Cancers (Basel). 2019; 11(3), 403:1–12.
Kennedy J, Wang CC, Wu CH. Patient disclosure about herb and supplement use among adults in the US. Evid Based Complement Alternat Med. 2008;5(4):451–6.
Hsueh CH, Hsu V, Pan Y, Zhao P. Predictive performance of physiologically-based pharmacokinetic models in predicting drug-drug interactions involving enzyme modulation. Clin Pharmacokinet. 2018;57(10):1337–46.
Grimstein M, Yang Y, Zhang X, Grillo J, Huang SM, Zineh I, et al. Physiologically based pharmacokinetic modeling in regulatory science: an update from the U.S. Food and Drug Administration's Office of Clinical Pharmacology. J Pharm Sci. 2019;108(1):21–5.
Brantley SJ, Gufford BT, Dua R, Fediuk DJ, Graf TN, Scarlett YV, et al. Physiologically based pharmacokinetic modeling framework for quantitative prediction of an herb-drug interaction. CPT Pharmacometrics Syst Pharmacol. 2014;3:e107.
Adiwidjaja J, Boddy AV, McLachlan AJ. Physiologically based pharmacokinetic modelling of hyperforin to predict drug interactions with St John's wort. Clin Pharmacokinet. 2019;58(7):911–26.
Parmentier Y, Pothier C, Delmas A, Caradec F, Trancart MM, Guillet F, et al. Direct and quantitative evaluation of the human CYP3A4 contribution (fm) to drug clearance using the In Vitro silensomes model. Xenobiotica. 2017;47(7):562–75.
Filppula AM, Neuvonen M, Laitila J, Neuvonen PJ, Backman JT. Autoinhibition of CYP3A4 leads to important role of CYP2C8 in imatinib metabolism: variability in CYP2C8 activity may alter plasma concentrations and response. Drug Metab Dispos. 2013;41(1):50–9.
Arellano C, Gandia P, Lafont T, Jongejan R, Chatelut E. Determination of unbound fraction of imatinib and N-desmethyl imatinib, validation of an UPLC-MS/MS assay and ultrafiltration method. J Chromatogr B Analyt Technol Biomed Life Sci. 2012;907:94–100.
Gota VS, Maru GB, Soni TG, Gandhi TR, Kochar N, Agarwal MG. Safety and pharmacokinetics of a solid lipid curcumin particle formulation in osteosarcoma patients and healthy volunteers. J Agric Food Chem. 2010;58(4):2095–9.
Haupt LJ, Kazmi F, Ogilvie BW, Buckley DB, Smith BD, Leatherman S, et al. The reliability of estimating ki values for direct, reversible inhibition of cytochrome P450 enzymes from corresponding IC50 values: a retrospective analysis of 343 experiments. Drug Metab Dispos. 2015;43(11):1744–50.
Turner DB. Rostami-Hodjegan A. Rowland-Yeo K. Prediction of non-specific hepatic microsomal binding from readily available physicochemical properties: Tucker GT; 2006. https://www.certara.com/wp-content/uploads/Resources/Posters/DavidISSX2006.pdf
Venkatakrishnan K, von Moltke LL, Obach RS, Greenblatt DJ. Drug metabolism and drug interactions: application and clinical value of In Vitro models. Curr Drug Metab. 2003;4(5):423–59.
Lestari ML, Indrayanto G. Curcumin. Profiles Drug Subst Excip Relat Methodol. 2014;39:113–204.
Guri A, Gulseren I, Corredig M. Utilization of solid lipid nanoparticles for enhanced delivery of curcumin in cocultures of HT29-MTX and Caco-2 cells. Food Funct. 2013;4(9):1410–9.
Vareed SK, Kakarala M, Ruffin MT, Crowell JA, Normolle DP, Djuric Z, et al. Pharmacokinetics of curcumin conjugate metabolites in healthy human subjects. Cancer Epidemiol Biomark Prev. 2008;17(6):1411–7.
Anuchapreeda S, Leechanachai P, Smith MM, Ambudkar SV, Limtrakul PN. Modulation of P-glycoprotein expression and function by curcumin in multidrug-resistant human KB cells. Biochem Pharmacol. 2002;64(4):573–82.
Wattanachai N, Polasek TM, Heath TM, Uchaipichat V, Tassaneeyakul W, Tassaneeyakul W, et al. In Vitro-In Vivo extrapolation of CYP2C8-catalyzed paclitaxel 6alpha-hydroxylation: effects of albumin on In Vitro kinetic parameters and assessment of interindividual variability in predicted clearance. Eur J Clin Pharmacol. 2011;67(8):815–24.
Hossain MA, Tran T, Chen T, Mikus G, Greenblatt DJ. Inhibition of human cytochromes P450 In Vitro by ritonavir and cobicistat. J Pharm Pharmacol. 2017;69(12):1786–93.
Kerdpin O, Elliot DJ, Boye SL, Birkett DJ, Yoovathaworn K, Miners JO. Differential contribution of active site residues in substrate recognition sites 1 and 5 to cytochrome P450 2C8 substrate selectivity and regioselectivity. Biochemistry. 2004;43(24):7834–42.
Miners JO, Bowalgaha K, Elliot DJ, Baranczewski P, Knights KM. Characterization of niflumic acid as a selective inhibitor of human liver microsomal UDP-glucuronosyltransferase 1A9: application to the reaction phenotyping of acetaminophen glucuronidation. Drug Metab Dispos. 2011;39(4):644–52.
Jamei M, Marciniak S, Edwards D, Wragg K, Feng K, Barnett A, et al. The Simcyp population based simulator: architecture, implementation, and quality assurance. In Silico Pharmacol. 2013;1:9.
Pulla Reddy AC, Sudharshan E, Appu Rao AG, Lokesh BR. Interaction of curcumin with human serum albumin--a spectroscopic study. Lipids. 1999;34(10):1025–9.
Rodgers T, Rowland M. Mechanistic approaches to volume of distribution predictions: understanding the processes. Pharm Res. 2007;24(5):918–33.
Darwich AS, Neuhoff S, Jamei M, Rostami-Hodjegan A. Interplay of metabolism and transport in determining oral drug absorption and gut wall metabolism: a simulation assessment using the "advanced dissolution, absorption, metabolism (ADAM)" model. Curr Drug Metab. 2010;11(9):716–29.
Jamei M, Turner D, Yang J, Neuhoff S, Polak S, Rostami-Hodjegan A, et al. Population-based mechanistic prediction of oral drug absorption. AAPS J. 2009;11(2):225–37.
Couto N, Al-Majdoub ZM, Gibson S, Davies PJ, Achour B, Harwood MD, et al. Quantitative proteomics of clinically relevant drug-metabolizing enzymes and drug transporters and their intercorrelations in the human small intestine. Drug Metab Dispos. 2020;48(4):245–54.
Drozdzik M, Groer C, Penski J, Lapczuk J, Ostrowski M, Lai Y, et al. Protein abundance of clinically relevant multidrug transporters along the entire length of the human intestine. Mol Pharm. 2014;11(10):3547–55.
Holder GM, Plummer JL, Ryan AJ. The metabolism and excretion of curcumin (1,7-bis-(4-hydroxy-3-methoxyphenyl)-1,6-heptadiene-3,5-dione) in the rat. Xenobiotica. 1978;8(12):761–8.
Ireson C, Orr S, Jones DJ, Verschoyle R, Lim CK, Luo JL, et al. Characterization of metabolites of the chemopreventive agent curcumin in human and rat hepatocytes and in the rat In Vivo, and evaluation of their ability to inhibit phorbol ester-induced prostaglandin E2 production. Cancer Res. 2001;61(3):1058–64.
Pan MH, Huang TM, Lin JK. Biotransformation of curcumin through reduction and glucuronidation in mice. Drug Metab Dispos. 1999;27(4):486–94.
Ireson CR, Jones DJ, Orr S, Coughtrie MW, Boocock DJ, Williams ML, et al. Metabolism of the cancer chemopreventive agent curcumin in human and rat intestine. Cancer Epidemiol Biomark Prev. 2002;11(1):105–11.
Hoehle SI, Pfeiffer E, Metzler M. Glucuronidation of curcuminoids by human microsomal and recombinant UDP-glucuronosyltransferases. Mol Nutr Food Res. 2007;51(8):932–8.
Bolger GT, Licollari A, Tan A, Greil R, Vcelar B, Greil-Ressler S, et al. Pharmacokinetics of liposomal curcumin (Lipocurc) infusion: effect of co-medication in cancer patients and comparison with healthy individuals. Cancer Chemother Pharmacol. 2019;83(2):265–75.
Storka A, Vcelar B, Klickovic U, Gouya G, Weisshaar S, Aschauer S, et al. Safety, tolerability and pharmacokinetics of liposomal curcumin in healthy humans. Int J Clin Pharmacol Ther. 2015;53(1):54–65.
Houston JB. Drug metabolite kinetics. Pharmacol Ther. 1981;15(3):521–52.
Zanger UM, Schwab M. Cytochrome P450 enzymes in drug metabolism: regulation of gene expression, enzyme activities, and impact of genetic variation. Pharmacol Ther. 2013;138(1):103–41.
Barter ZE, Chowdry JE, Harlow JR, Snawder JE, Lipscomb JC, Rostami-Hodjegan A. Covariation of human microsomal protein per gram of liver with age: absence of influence of operator and sample storage may justify interlaboratory data pooling. Drug Metab Dispos. 2008;36(12):2405–9.
Johnson TN, Tucker GT, Tanner MS, Rostami-Hodjegan A. Changes in liver volume from birth to adulthood: a meta-analysis. Liver Transpl. 2005;11(12):1481–93.
Hatley OJ, Jones CR, Galetin A, Rostami-Hodjegan A. Quantifying gut wall metabolism: methodology matters. Biopharm Drug Dispos. 2017;38(2):155–60.
Adiwidjaja J, Boddy AV, McLachlan AJ. Implementation of a physiologically based pharmacokinetic modelling approach to guide optimal dosing regimens for imatinib and potential drug interactions in paediatrics. Front Pharmacol. 1672;2020(10):1–18.
Ono C, Hsyu PH, Abbas R, Loi CM, Yamazaki S. Application of physiologically based pharmacokinetic modeling to the understanding of bosutinib pharmacokinetics: prediction of drug-drug and drug-disease interactions. Drug Metab Dispos. 2017;45(4):390–8.
Gufford BT, Chen G, Lazarus P, Graf TN, Oberlies NH, Paine MF. Identification of diet-derived constituents as potent inhibitors of intestinal glucuronidation. Drug Metab Dispos. 2014;42(10):1675–83.
Greil R, Greil-Ressler S, Weiss L, Schonlieb C, Magnes T, Radl B, et al. A phase 1 dose-escalation study on the safety, tolerability and activity of liposomal curcumin (Lipocurc™) in patients with locally advanced or metastatic cancer. Cancer Chemother Pharmacol. 2018;82(4):695–706.
Nelson KM, Dahlin JL, Bisson J, Graham J, Pauli GF, Walters MA. The essential medicinal chemistry of curcumin. J Med Chem. 2017;60(5):1620–37.
Cheng D, Li W, Wang L, Lin T, Poiani G, Wassef A, et al. Pharmacokinetics, pharmacodynamics, and PKPD modeling of curcumin in regulating antioxidant and epigenetic gene expression in healthy human volunteers. Mol Pharm. 2019;16(5):1881–9.
Vieira ML, Kirby B, Ragueneau-Majlessi I, Galetin A, Chien JY, Einolf HJ, et al. Evaluation of various static In Vitro-In Vivo extrapolation models for risk assessment of the CYP3A inhibition potential of an investigational drug. Clin Pharmacol Ther. 2014;95(2):189–98.
Guest EJ, Rowland-Yeo K, Rostami-Hodjegan A, Tucker GT, Houston JB, Galetin A. Assessment of algorithms for predicting drug-drug interactions via inhibition mechanisms: comparison of dynamic and static models. Br J Clin Pharmacol. 2011;71(1):72–87.
Fahmi OA, Hurst S, Plowchalk D, Cook J, Guo F, Youdim K, et al. Comparison of different algorithms for predicting clinical drug-drug interactions, based on the use of CYP3A4 In Vitro data: predictions of compounds as precipitants of interaction. Drug Metab Dispos. 2009;37(8):1658–66.
Rowland-Yeo K, Jamei M, Rostami-Hodjegan A. Predicting drug-drug interactions: application of physiologically based pharmacokinetic models under a systems biology approach. Expert Rev Clin Pharmacol. 2013;6(2):143–57.
Einolf HJ, Chen L, Fahmi OA, Gibson CR, Obach RS, Shebley M, et al. Evaluation of various static and dynamic modeling methods to predict clinical CYP3A induction using In Vitro CYP3A4 mRNA induction data. Clin Pharmacol Ther. 2014;95(2):179–88.
Mach CM, Chen JH, Mosley SA, Kurzrock R, Smith JA. Evaluation of liposomal curcumin cytochrome P450 metabolism. Anticancer Res. 2010;30(3):811–4.
Liu Y, Ramirez J, Ratain MJ. Inhibition of paracetamol glucuronidation by tyrosine kinase inhibitors. Br J Clin Pharmacol. 2011;71(6):917–20.
Kim DW, Tan EY, Jin Y, Park S, Hayes M, Demirhan E, et al. Effects of imatinib mesylate on the pharmacokinetics of paracetamol (acetaminophen) in Korean patients with chronic myelogenous leukaemia. Br J Clin Pharmacol. 2011;71(2):199–206.
Zeng X, Cai D, Zeng Q, Chen Z, Zhong G, Zhuo J, et al. Selective reduction in the expression of UGTs and SULTs, a novel mechanism by which piperine enhances the bioavailability of curcumin in rat. Biopharm Drug Dispos. 2017;38(1):3–19.
Gao Y, Chen G, Luan X, Zou M, Piao H, Cheng G. Improved oral absorption of poorly soluble curcumin via the concomitant use of borneol. AAPS PharmSciTech. 2019;20(4):150.
Moeller T, Six C, Dennell S, Rose T, Watt C. Demographic differences by age, BMI, gender and disease states of phase I and phase II enzyme activities in cryopreserved human hepatocytes. The Toxicologist: Supplement to Toxicological Sciences. 2013; 132(1):Abstract no. 305.
Badee J, Fowler S, de Wildt SN, Collier AC, Schmidt S, Parrott N. The ontogeny of UDP-glucuronosyltransferase enzymes, recommendations for future profiling studies and application through physiologically based pharmacokinetic modelling. Clin Pharmacokinet. 2019;58(2):189–211.
Hu S, Maiti P, Ma Q, Zuo X, Jones MR, Cole GM, et al. Clinical development of curcumin in neurodegenerative disease. Expert Rev Neurother. 2015;15(6):629–37.
Cox KH, Pipingas A, Scholey AB. Investigation of the effects of solid lipid curcumin on cognition and mood in a healthy older population. J Psychopharmacol. 2015;29(5):642–51.
Gupte PA, Giramkar SA, Harke SM, Kulkarni SK, Deshmukh AP, Hingorani LL, et al. Evaluation of the efficacy and safety of capsule Longvida® optimized curcumin (solid lipid curcumin particles) in knee osteoarthritis: a pilot clinical study. J Inflamm Res. 2019;12:145–52.
Dadhaniya P, Patel C, Muchhara J, Bhadja N, Mathuria N, Vachhani K, et al. Safety assessment of a solid lipid curcumin particle preparation: acute and subchronic toxicity studies. Food Chem Toxicol. 2011;49(8):1834–42.
Nair AB, Jacob S. A simple practice guide for dose conversion between animals and human. J Basic Clin Pharm. 2016;7(2):27–31.
He X, Mo L, Li ZY, Tan ZR, Chen Y, Ouyang DS. Effects of curcumin on the pharmacokinetics of talinolol in human with ABCB1 polymorphism. Xenobiotica. 2012;42(12):1248–54.
Trevaskis NL, Kaminskas LM, Porter CJ. From sewer to saviour - targeting the lymphatic system to promote drug exposure and activity. Nat Rev Drug Discov. 2015;14(11):781–803.
Feng T, Wei Y, Lee RJ, Zhao L. Liposomal curcumin and its application in cancer. Int J Nanomedicine. 2017;12:6027–44.
Ait-Oudhia S, Mager DE, Straubinger RM. Application of pharmacokinetic and pharmacodynamic analysis to the development of liposomal formulations for oncology. Pharmaceutics. 2014;6(1):137–74.
Acknowledgments and Disclosures
The In Vitro study was supported by a research grant from Indonesia Endowment Fund for Education (LPDP), Ministry of Finance of the Republic of Indonesia. J.A. is receiving a postgraduate scholarship from Indonesia Endowment Fund for Education (LPDP). Certara UK Limited (Simcyp Division) is gratefully acknowledged for providing the access to the Simcyp Simulator. There are no competing interests to declare.
Author information
Authors and Affiliations
Contributions
J.A., A.V.B. and A.J.M. designed the research and contributed to the interpretation. J.A. performed the simulations and In Vitro experiments, analysed the data and drafted the manuscript. A.V.B. and A.J.M. critically revised the manuscript.
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Adiwidjaja, J., Boddy, A.V. & McLachlan, A.J. Physiologically-Based Pharmacokinetic Predictions of the Effect of Curcumin on Metabolism of Imatinib and Bosutinib: In Vitro and In Vivo Disconnect. Pharm Res 37, 128 (2020). https://doi.org/10.1007/s11095-020-02834-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11095-020-02834-8