Abstract
Purpose
A novel polymer micelle was prepared with a high drug loading, good stability, high tolerance and better anti-tumor effect.
Methods
TM-2 was encapsulated in poly-block-poly (D, L-lactic acid) self-assembled micelles by the thin-film hydration method. From the critical micelle concentrations of the copolymers, particle size, drug loading and encapsulation efficiency of drug-loading micelles, the appropriate polymer material could be assessed. Comparisons between TM-2 solution and TM-2 micelles were done to evaluate the pharmacokinetics and toxicity in rats, compared with Taxol to evaluate the anti-tumor effect in mice.
Results
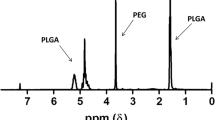
The optimized TM-2 micelles achieved a high drug loading (~20%) with the polymer material of PEG2k-PLA2.5k, with a particle size of 30 nm and no significant change in particle size after lyophilization. The result of pharmacokinetic experiment displayed that the half-life in vivo was obviously prolonged. The maximum tolerated dose of TM-2 micelles was approximately 25 mg/kg in rats, and the relative tumor growth rate of Taxol (15 mg/kg), TM-2 (10 mg/kg), TM-2 (15 mg/kg) and TM-2 (40 mg/kg) in mice were 49.35%, 49.14%, 36.44 and 9.98% respectively.
Conclusions
TM-2 micelles with high drug loading increased drug solubility, improved tolerance, antitumor effects and reduced toxicity.






Similar content being viewed by others
Abbreviations
- A549:
-
Human lung xenografts
- ACN:
-
Acetonitrile
- AUC:
-
Concentration-time curve
- BC:
-
Breast cancer
- Clz :
-
Plasma clearance
- Cmax :
-
Maximum plasma concentration
- CMC:
-
Critical micelle concentration
- CrEL:
-
Cremophor EL
- CYP:
-
Cytochrome P450 proteins
- DL:
-
Drug loading
- DLS:
-
Dynamic light scattering
- DMF:
-
N-N dimethylformamide
- DSC:
-
Differential scanning calorimetry
- EE:
-
Encapsulation efficiency
- FTIR:
-
Fourier Transform infrared spectroscopy
- GPC:
-
Gel permeation chromatography
- KB/VCR:
-
Human cervical adenocarcinoma resistant to vincristine
- MBC:
-
Metastatic breast cancer
- MCF:
-
7/ADR-Human breast cancer resistant to adriamycin
- MDR:
-
Multiple drug resistance
- MTD:
-
The maximum tolerable dose
- NSCLC:
-
Non-small cell lung cancer
- OC:
-
Ovarian cancer
- ODnc:
-
Negative control absorbance
- ODpc:
-
Positive control absorbance
- ODt:
-
Sample absorbance
- PBS:
-
Phosphate-buffered saline
- PDI:
-
Polydispersity index
- PEG:
-
PLA-Poly-block-poly (D, L-lactic acid)
- PSD:
-
Particle size distribution
- PSMA:
-
Prostate-specific membrane antigen
- PTX:
-
Paclitaxel
- RTV:
-
Relative tumor volume
- SD:
-
Male Sprague-Dawley
- T/C:
-
Relative tumor growth rate
- t1/2 :
-
Elimination half-life
- Taxol:
-
Commercial name of paclitaxel solution
- TEM:
-
Transmission electron microscopy
- Tmax :
-
Maximum plasma concentration
- Tween:
-
Polysorbate
- XRD:
-
X-ray diffraction
References
Shi J, Chen X, Gu Y, et al. Preformulation and development of chemically stable lipid emulsions containing a novel taxane derivative, TM-2. Eur J Lipid Sci Technol. 2014;116(4):486–96.
Lin H, Zhao Y, Men L, Yang M, Liu H, Shao Y, et al. Development of a rapid and sensitive UPLC-MS/MS assay for the determination of TM-2 in beagle dog plasma and its application to a pharmacokinetic study. Biomed Chromatogr. 2015;29(1):110–4.
Men L, Lin H, Zhao Y, Liu H, Yang M, Fan R, et al. Metabolism of TM-2, a potential antitumor drug, in rats by using LC-MS. J Sep Sci. 2014;37(6):625–9.
Hennenfent KL, Govindan R. Novel formulations of taxanes: a review. Old wine in a new bottle? Ann Oncol. 2006;17(5):735–49.
Reddy LH, Bazile D. Drug delivery design for intravenous route with integrated physicochemistry, pharmacokinetics and pharmacodynamics: illustration with the case of taxane therapeutics. Adv Drug Deliv Rev. 2014;71:34–57.
Sofias AM, Dunne M, Storm G, Allen C. The battle of "nano" paclitaxel. Adv Drug Deliv Rev. 2017;122:20–30.
Tae-You Kim D-WK, et al. Phase I and Pharmacopoeia Study of Gene-PM, a Cremophor-Free, Polymeric Micelle-Formulated Paclitaxel, in Patients with Advanced Malignancies. Clin Cancer Res. 2004;10:3708–16.
Ibrahim ND NK, Legha S, Soon-Shiong P, Theriault RL, Rivera E, Esmaeli B, et al. Phase I and pharmacokinetic study of ABI-007, a Cremophor-free, protein-stabilized, Nanoparticle Formulationof Paclitaxel. Clin Cancer Res. 2002;8:1038–44.
Yamada K, Yamamoto N, Yamada Y, Mukohara T, Minami H, Tamura T. Phase I and pharmacokinetic study of ABI-007, albumin-bound paclitaxel, administered every 3 weeks in Japanese patients with solid tumors. Jpn J Clin Oncol. 2010;40(5):404–11.
Petros RA, DeSimone JM. Strategies in the design of nanoparticles for therapeutic applications. Nat Rev Drug Discov. 2010;9(8):615–27.
Jeffrey Hrkach DVH, Ali MM, Andrianova E, Auer J. Preclinical development and clinical translation of aPSMA-targeted docetaxel nanoparticle with a differentiated pharmacologicalprofile. Nanomedicine. 2012;4:128.
Von Hoff DD, Mita MM, Ramanathan RK, Weiss GJ, Mita AC, LoRusso PM, et al. Phase I Study of PSMA-targeted Docetaxel-containing nanoparticle BIND-014 in patients with advanced solid tumors. Clin Cancer Res. 2016;22(13):3157–63.
Shalgunov V, Zaytseva-Zotova D, Zintchenko A, Levada T, Shilov Y, Andreyev D, et al. Safarovsmall a CE. Comprehensive study of the drug delivery properties of poly(l-lactide)-poly(ethylene glycol) nanoparticles in rats and tumor-bearing mice. J Control Release. 2017;261:31–42.
He Z, Wan X, Schulz A, Bludau H, Dobrovolskaia MA, Stern ST, et al. A high capacity polymeric micelle of paclitaxel: implication of high dose drug therapy to safety and in vivo anti-cancer activity. Biomaterials. 2016;101:296–309.
Li Y, He H, Wang Q, Tang X. Preparation, stability and pharmacokinetics evaluation of lipid microspheres loading a promising antitumor candidate, Timataxel. Asian J Pharm Sci. 2016;11(6):771–9.
Marques MRC, Loebenberg R, Almukainzi M. Simulated biological fluids with possible application in dissolution testing. Dissolut Technol. 2011;18(3):15–28.
Zeng R.Lin H.Leng Y.Xu J.Ma J. Studies on hemolysis properties of medical α-calcium sulfate hemihydrate. Journal of Hainan Medical University 2017:16–18.
Mei T, Zhu Y, Ma T, He T, Li L, Wei C, et al. Synthesis, characterization, and biocompatibility of alternating block polyurethanes based on PLA and PEG. J Biomed Mater Res A. 2014;102(9):3243–54.
Duan X, Li Y. Physicochemical characteristics of nanoparticles affect circulation, biodistribution, cellular internalization, and trafficking. Small. 2013;9(9–10):1521–32.
Burt H M, Zhang X,Toleikis P,Embree L,Hunter W. Development of copolymers of poly(d,l-lactide) and methoxypolyethylene glycol as micellar carriers of paclitaxel. Colloid Ssurface B. 1999:161–171.
Li X, Yang Z, Yang K, Zhou Y, Chen X, Zhang Y, et al. Self-assembled polymeric Micellar nanoparticles as Nanocarriers for poorly soluble anticancer drug Ethaselen. Nanoscale Res Lett. 2009;4(12):1502–11.
Riley T, Heald CR, Stolnik S, Garnett MC, Illum L, Davis SS. Core-shell structure of PLA-PEG nanoparticles used for drug delivery. J Am Chem Soc. 2003;19(20):8428–35.
Stolnik S, Heald CR, Neal J, Garnett MC, Davis SS, Illum L, et al. Polylactide-poly(ethylene glycol) Micellar-like particles as potential drug carriers: production, colloidal properties and biological performance. J Drug Target. 2010;9(5):361–78.
Ernsting MJ, Murakami M, Roy A, Li SD. Factors controlling the pharmacokinetics, biodistribution and intratumoral penetration of nanoparticles. J Control Release. 2013;172(3):782–94.
Decuzzi P, Godin B, Tanaka T, Lee SY, Chiappini C, Liu X, et al. Size and shape effects in the biodistribution of intravascularly injected particles. J Control Release. 2010;141(3):320–7.
Sung Chul Kim DWK, Shim YH, Bang JS, Hun Seung O, Kim SW, Seo MH. In vivo evaluation of polymeric micellar paclitaxel formulation_ toxicity and efficacy. J Control Release. 2001;72(1–3):191–202.
Dong Y, Feng SS. In vitro and in vivo evaluation of methoxy polyethylene glycol-polylactide (MPEG-PLA) nanoparticles for small-molecule drug chemotherapy. Biomaterials. 2007;28(28):4154–60.
Bazile D, Homme C P, Bassoulet M T, Marlard M, Spenlehauer G, Veillard M. Stealth Me_PEG-PLA nanoparticles avoid uptake by the mononuclear phagocytes system. J Pharm Sci. 1995;84(4):493–8.
Sheng Y, Yuan Y, Liu C, Tao X, Shan X, Xu F. In vitro macrophage uptake and in vivo biodistribution of PLA-PEG nanoparticles loaded with hemoglobin as blood substitutes: effect of PEG content. J Mater Sci Mater Med. 2009;20(9):1881–91.
Zasadil LM, Andersen KA, Yeum D, Rocque GB, Wilke LG, Tevaarwerk AJ, et al. Cytotoxicity of paclitaxel in breast cancer is due to chromosome missegregation on multipolar spindles. Sci Transl Med. 2014;6(229):229ra243.
Davis ME, Chen ZG, Shin DM. Nanoparticle therapeutics: an emerging treatment modality for cancer. Nat Rev Drug Discov. 2008;7(9):771–82.
Cabral H, Matsumoto Y, Mizuno K, Chen Q, Murakami M, Kimura M, et al. Accumulation of sub-100 nm polymeric micelles in poorly permeable tumours depends on size. Nat Nanotechnol. 2011;6(12):815–23.
Ma P, Mumper RJ. Paclitaxel Nano-delivery systems: a comprehensive review. J Nanomed Nanotechnol. 2013;4(2):1000164.
Xiao L, Xiong X, Sun X, Zhu Y, Yang H, Chen H, et al. Role of cellular uptake in the reversal of multidrug resistance by PEG-b-PLA polymeric micelles. Biomaterials. 2011;32(22):5148–57.
Lakkireddy HR, Bazile D. Building the design, translation and development principles of polymeric nanomedicines using the case of clinically advanced poly(lactide(glycolide))-poly(ethylene glycol) nanotechnology as a model: an industrial viewpoint. Adv Drug Deliv Rev. 2016;107:289–332.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wang, Q., Liu, Y., Pu, C. et al. Drug-Polymer Interaction, Pharmacokinetics and Antitumor Effect of PEG-PLA/Taxane Derivative TM-2 Micelles for Intravenous Drug Delivery. Pharm Res 35, 208 (2018). https://doi.org/10.1007/s11095-018-2477-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11095-018-2477-3