ABSTRACT
Purpose
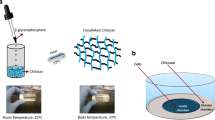
Chitosan-shelled/decafluoropentane-cored oxygen-loaded nanodroplets (OLN) are a new class of nanodevices to effectively deliver anti-cancer drugs to tumoral cells. This study investigated their antitumoral effects ‘per se’, using a mathematical model validated on experimental data.
Methods
OLN were prepared and characterized either in vitro or in vivo. TUBO cells, established from a lobular carcinoma of a BALB-neuT mouse, were investigated following 48 h of incubation in the absence/presence of different concentrations of OLN. OLN internalization, cell viability, necrosis, apoptosis, cell cycle and reactive oxygen species (ROS) production were checked as described in the Method section.
In vivo tumor growth was evaluated after subcutaneous transplant in BALB/c mice of TUBO cells either without treatment or after 24 h incubation with 10% v/v OLN.
Results
OLN showed sizes of about 350 nm and a positive surface charge (45 mV). Dose-dependent TUBO cell death through ROS-triggered apoptosis following OLN internalization was detected. A mathematical model predicting the effects of OLN uptake was validated on both in vitro and in vivo results.
Conclusions
Due to their intrinsic toxicity OLN might be considered an adjuvant tool suitable to deliver their therapeutic cargo intracellularly and may be proposed as promising combined delivery system.







Similar content being viewed by others
Abbreviations
- DAPI:
-
Diamidino-2-phenylindole dihydrochloride
- DMEM:
-
Dulbecco’s modified eagle medium
- FITC:
-
Fluorescein isothiocyanate
- LDH:
-
Lactate dehydrogenase
- MTT:
-
3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide
- OLN:
-
Oxygen-loaded Nanodroplets
- ROS:
-
Oxygen Reactive Species
References
Talevi A, Gantner ME, Ruiz ME. Applications of nanosystems to anticancer drug therapy (Part I. Nanogels, nanospheres, nanocapsules). Recent Pat Anticancer Drug Discov. 2014;9(1):83–98.
Ferrari M. Nanovector therapeutics. Curr Opin Chem Biol. 2005;9(4):343–6.
Gao H, Shi W, Freund LB. Mechanics of receptor-mediated endocytosis. Proc Natl Acad Sci U S A. 2005;102(27):9469–74.
Mora-Huertas CE, Fessi H, Elaissari A. Polymer-based nanocapsules for drug delivery. Int J Pharm. 2010;385(1–2):113–42.
Barrera G, Daga M, Ferrara B, Dianzani C, Pizzimenti S, Argenziano M, et al. Drug delivery nanoparticles in treating Chemoresistant tumor cells. Curr Med Chem. 2017;24(42):4800–15.
Lin Q, Bao C, Yang Y, Liang Q, Zhang D, Cheng S, et al. Highly discriminating photorelease of anticancer drugs based on hypoxia activatable phototrigger conjugated chitosan nanoparticles. Adv Mater. 2013;25(14):1981–6.
Magnetto C, Prato M, Khadjavi A, Giribaldi G, Fenoglio I, Jose J, et al. Ultrasound-activated decafluoropentane-cored and chitosan-shelled nanodroplets for oxygen delivery to hypoxic cutaneous tissues. RSC Adv. 2014;4(72):38433–41.
Prato M, Magnetto C, Jose J, Khadjavi A, Cavallo F, Quaglino E, et al. 2H,3H-decafluoropentane-based nanodroplets: new perspectives for oxygen delivery to hypoxic cutaneous tissues. PLoS One. 2015;10(3):e0119769.
Cavalli R, Bisazza A, Giustetto P, Civra A, Lembo D, Trotta G, et al. Preparation and characterization of dextran nanobubbles for oxygen delivery. Int J Pharm. 2009;381(2):160–5.
Cavalli R, Bisazza A, Rolfo A, Balbis S, Madonnaripa D, Caniggia I, et al. Ultrasound-mediated oxygen delivery from chitosan nanobubbles. Int J Pharm. 2009;378(1–2):215–7.
Banche G, Prato M, Magnetto C, Allizond V, Giribaldi G, Argenziano M, et al. Antimicrobial chitosan nanodroplets: new insights for ultrasound-mediated adjuvant treatment of skin infection. Future Microbiol. 2015;10(6):929–39.
Khadjavi A, Magnetto C, Panariti A, Argenziano M, Gulino GR, Rivolta I, et al. Chitosan-shelled oxygen-loaded nanodroplets abrogate hypoxia dysregulation of human keratinocyte gelatinases and inhibitors: new insights for chronic wound healing. Toxicol Appl Pharmacol. 2015;286(3):198–206.
Rovero S, Amici A, Carlo ED, Bei R, Nanni P, Quaglino E, et al. DNA vaccination against rat her-2/Neu p185 more effectively inhibits carcinogenesis than transplantable carcinomas in transgenic BALB/c mice. J Immunol. 2000;165(9):5133–42.
Minero VG, Khadjavi A, Costelli P, Baccino FM, Bonelli G. JNK activation is required for TNFalpha-induced apoptosis in human hepatocarcinoma cells. Int Immunopharmacol. 2013;17(1):92–8.
Salvati A, Åberg C, dos Santos T, Varela J, Pinto P, Lynch I, et al. Experimental and theoretical comparison of intracellular import of polymeric nanoparticles and small molecules: toward models of uptake kinetics. Nanomedicine. 2011;7(6):818–26.
Maher MA, Naha PC, Mukherjee SP, Byrne HJ. Numerical simulations of in vitro nanoparticle toxicity - the case of poly(amido amine) dendrimers. Toxicol in Vitro. 2014;28(8):1449–60.
Souto GD, Farhane Z, Casey A, Efeoglu E, McIntyre J, Byrne HJ. Evaluation of cytotoxicity profile and intracellular localisation of doxorubicin-loaded chitosan nanoparticles. Anal Bioanal Chem. 2016;408(20):5443–55.
Kanapathipillai M, Brock A, Ingber DE. Nanoparticle targeting of anti-cancer drugs that alter intracellular signaling or influence the tumor microenvironment. Adv Drug Deliv Rev. 2014;79-80:107–18.
Duchene D, Cavalli R, Gref R. Cyclodextrin-based polymeric nanoparticles as efficient carriers for anticancer drugs. Curr Pharm Biotechnol. 2016;17(3):248–55.
Li Q, Dunn ET, Grandmaison EW, Goosen MFA. Applications and properties of chitosan. J Bioact Compat Polym. 1992;7(4):370–97.
Kumar MNVR, Muzzarelli RAA, Muzzarelli C, Sashiwa H, Domb AJ. Chitosan chemistry and pharmaceutical perspectives. Chem Rev. 2004;104(12):6017–84.
Qi LF, Xu ZR, Li Y, Jiang X, Han XY. In Vitro effects of chitosan nanoparticles on proliferation of human gastric carcinoma cell line MGC803 cells. World J Gastroenterol. 2005;11(33):5136–41.
Qi LF, Xu ZR. In vivo antitumor activity of chitosan nanoparticles. Bioorg Med Chem Lett. 2006;16(16):4243–5.
Jiang M, Ouyang H, Ruan P, Zhao H, Pi Z, Huang S, et al. Chitosan derivatives inhibit cell proliferation and induce apoptosis in breast cancer cells. Anticancer Res. 2011;31(4):1321–8.
Salah R, Michaud P, Mati F, Harrat Z, Lounici H, Abdi N, et al. Anticancer activity of chemically prepared shrimp low molecular weight chitin evaluation with the human monocyte leukaemia cell line, THP-1. Int J Biol Macromol. 2013;52:333–9.
Xu YL, et al. Chitosan nanoparticles inhibit the growth of human hepatocellular carcinoma xenografts through an antiangiogenic mechanism. Anticancer Res. 2009;29(12):5103–9.
Hasegawa M, Yagi K, Iwakawa S, Hirai M. Chitosan induces apoptosis via caspase-3 activation in bladder tumor cells. Jpn J Cancer Res. 2001;92(4):459–66.
Takimoto H, Hasegawa M, Yagi K, Nakamura T, Sakaeda T, Hirai M. Proapoptotic effect of a dietary supplement: water soluble chitosan activates caspase-8 and modulating death receptor expression. Drug Metab Pharmacokinet. 2004;19(1):76–82.
Amidi M, Mastrobattista E, Jiskoot W, Hennink WE. Chitosan-based delivery systems for protein therapeutics and antigens. Adv Drug Deliv Rev. 2010;62(1):59–82.
Kean T, Thanou M. Biodegradation, biodistribution and toxicity of chitosan. Adv Drug Deliv Rev. 2010;62(1):3–11.
Cavalli R, Leone F, Minelli R, Fantozzi R, Dianzani C. New chitosan nanospheres for the delivery of 5-fluorouracil: preparation, characterization and in vitro studies. Curr Drug Deliv. 2014;11(2):270–8.
Wilhelm C, Billotey C, Roger J, Pons JN, Bacri JC, Gazeau F. Intracellular uptake of anionic superparamagnetic nanoparticles as a function of their surface coating. Biomaterials. 2003;24(6):1001–11.
Lee JK, Lim HS, Kim JH. Cytotoxic activity of aminoderivatized cationic chitosan derivatives. Bioorg Med Chem Lett. 2002;12(20):2949–51.
Edinger AL, Thompson CB. Death by design: apoptosis, necrosis and autophagy. Curr Opin Cell Biol. 2004;16(6):663–9.
Görlach A, Dimova EY, Petry A, Martínez-Ruiz A, Hernansanz-Agustín P, Rolo AP, et al. Reactive oxygen species, nutrition, hypoxia and diseases: problems solved? Redox Biol. 2015;6:372–85.
Dunn JD, et al. Reactive oxygen species and mitochondria: a nexus of cellular homeostasis. Redox Biol. 2015;6:472–85.
Hsin YH, Chen CF, Huang S, Shih TS, Lai PS, Chueh PJ. The apoptotic effect of nanosilver is mediated by a ROS- and JNK-dependent mechanism involving the mitochondrial pathway in NIH3T3 cells. Toxicol Lett. 2008;179(3):130–9.
AshaRani PV, Low Kah Mun G, Hande MP, Valiyaveettil S. Cytotoxicity and genotoxicity of silver nanoparticles in human cells. ACS Nano. 2009;3(2):279–90.
Hussain SM, Hess KL, Gearhart JM, Geiss KT, Schlager JJ. In vitro toxicity of nanoparticles in BRL 3A rat liver cells. Toxicol in Vitro. 2005;19(7):975–83.
Limbach LK, Wick P, Manser P, Grass RN, Bruinink A, Stark WJ. Exposure of engineered nanoparticles to human lung epithelial cells: influence of chemical composition and catalytic activity on oxidative stress. Environ Sci Technol. 2007;41(11):4158–63.
Park EJ, Choi J, Park YK, Park K. Oxidative stress induced by cerium oxide nanoparticles in cultured BEAS-2B cells. Toxicology. 2008;245(1–2):90–100.
Kehrer JP, Klotz L. Free radicals and related reactive species as mediators of tissue injury and disease: implications for health. Crit Rev Toxicol. 2015;45(9):765–98.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Khadjavi, A., Stura, I., Prato, M. et al. ‘In Vitro’, ‘In Vivo’ and ‘In Silico’ Investigation of the Anticancer Effectiveness of Oxygen-Loaded Chitosan-Shelled Nanodroplets as Potential Drug Vector. Pharm Res 35, 75 (2018). https://doi.org/10.1007/s11095-018-2371-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11095-018-2371-z