Abstract
Purpose
This study investigated in vitro transdermal delivery of methotrexate through dermatomed porcine ear and cadaver human skin treated with poly (D,L-lactide-co-glycolide) acid microneedles or fractional ablative laser.
Methods
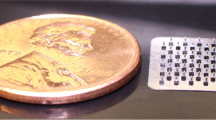
PLGA microneedles were fabricated and characterized using scanning electron microscopy and mechanical assessment techniques. The integrity of treated skin was evaluated by rheometer, transepidermal water loss, and skin electrical resistance measurements. Successful skin microporation was demonstrated by dye binding, histology, pore uniformity, confocal laser microscopy, and DermaScan studies. In vitro permeation experiment was performed on Franz diffusion cells to determine drug delivery into and across the skin.
Results
Both physical treatments resulted in a considerable decrease in skin resistance and an increase in transepidermal water loss value. The laser-created microchannels were significantly larger than those formed by microneedles (p < 0.05). An effective force of 41.04 ± 18.33 N was required to achieve 100% penetration efficiency of the microneedles. For both porcine ear and human skin, laser ablation provided a significantly higher methotrexate permeability into the receptor chamber and skin layers compared to microneedle poration and untreated skin (p < 0.05).
Conclusions
Both fractional ablative laser and polymeric microneedles markedly enhanced in vitro transdermal delivery of methotrexate into and across skin.

ᅟ















Similar content being viewed by others
Abbreviations
- FTIR:
-
Fourier transform infrared spectrophotometer
- MN:
-
Microneedles
- MTX:
-
Methotrexate
- PBS:
-
Phosphate buffered saline
- PDMS:
-
Polydimethylsiloxane
- PLGA:
-
Poly Lactic-co-Glycolic Acid
- PPI:
-
Pore permeability index
- RP-HPLC:
-
Reversed-phase high performance liquid chromatography
- SD:
-
Standard deviation
- SEM:
-
Scanning electron microscopy
- TEWL:
-
Transepidermal water loss
References
Abla MJ, Chaturvedula A, O’Mahony C, Banga AK. Transdermal delivery of methotrexate for pediatrics using silicon microneedles. Ther Deliv. 2013;4:543–51.
Prausnitz MR, Langer R. Transdermal drug delivery. Nat Biotechnol. 2008;26:1261–8.
Banga AK. Microporation applications for enhancing drug delivery. Expert Opin. Drug Deliv. 2009;6:343–54.
Haq MI, Smith E, John DN, Kalavala M, Edwards C, Anstey A, et al. Clinical administration of microneedles: skin puncture, pain and sensation. Biomed Microdevices. 2009;11:35–47.
Kalluri H, Banga AK. Microneedles and transdermal drug delivery. J Drug Delivery Sci Technol. 2009;19:303–10.
Heinrich A, Vizhanyo A, Krammer P, Summer S, Gross S, Bragagna T, et al. Next generation Er:YAG fractional ablative laser. 2011 [cited 2016 Sep 22]. p. 78830M–78830M–6. Available from: doi:https://doi.org/10.1117/12.873522.
Weiss R, Hessenberger M, Kitzmüller S, Bach D, Weinberger EE, Krautgartner WD, et al. Transcutaneous vaccination via laser microporation. J Control Release. 2012;162:391–9.
Sklar LR, Burnett CT, Waibel JS, Moy RL, Ozog DM. Laser assisted drug delivery: a review of an evolving technology. Lasers Surg Med. 2014;46:249–62.
Hantash BM, Bedi VP, Kapadia B, Rahman Z, Jiang K, Tanner H, et al. In vivo histological evaluation of a novel ablative fractional resurfacing device. Lasers Surg Med. 2007;39:96–107.
Taudorf EH, Haak CS, Erlendsson AM, Philipsen PA, Anderson R, Paasch U, et al. Fractional ablative erbium YAG laser: histological characterization of relationships between laser settings and micropore dimensions. Lasers Surg Med. 2014;46:281–9.
Erlendsson AM, Taudorf EH, Eriksson AH, Haak CS, Zibert JR, Paasch U, et al. Ablative fractional laser alters biodistribution of ingenol mebutate in the skin. Arch Dermatol Res. 2015;307:515–22.
Taudorf EH, Lerche CM, Erlendsson AM, Philipsen PA, Hansen SH, Janfelt C, et al. Fractional laser-assisted drug delivery: laser channel depth influences biodistribution and skin deposition of methotrexate. Lasers Surg Med. 2016;48:519–29.
Dadlani C, Orlow SJ. Treatment of children and adolescents with methotrexate, cyclosporine, and etanercept: review of the dermatologic and rheumatologic literature. J Am Acad Dermatol. 2005;52:316–40.
Patiño-García A, Zalacaín M, Marrodán L, San-Julián M, Sierrasesúmaga L. Methotrexate in pediatric osteosarcoma: response and toxicity in relation to genetic polymorphisms and dihydrofolate reductase and reduced folate carrier 1 expression. J Pediatr. 2009;154:688–93.
Vemulapalli V, Yang Y, Friden PM, Banga AK. Synergistic effect of iontophoresis and soluble microneedles for transdermal delivery of methotrexate. J Pharm Pharmacol. 2008;60:27–33.
Kelly A, Ramanan AV. The principles of pharmacological treatment of juvenile idiopathic arthritis. Paediatr Child Health. 2011;21:563–8.
Van Outryve S, Schrijvers D, Van Den Brande J, Wilmes P, Bogers J, Van Marck E, et al. Methotrexate-associated liver toxicity in a patient with breast cancer: case report and literature review. Neth J Med. 2002;60:216–22.
Vagace JM, de la Maya MD, Caceres-Marzal C, de Murillo SG, Gervasini G. Central nervous system chemotoxicity during treatment of pediatric acute lymphoblastic leukemia/lymphoma. Crit Rev Oncol Hematol. 2012;84:274–86.
Fang J-Y, Liu P-F, Huang C-M. Decreasing systemic toxicity via transdermal delivery of anticancer drugs. Curr Drug Metab. 2008;9:592–7.
Alvarez-Figueroa MJ, Blanco-Mendez J. Transdermal delivery of methotrexate: iontophoretic delivery from hydrogels and passive delivery from microemulsions. Int J Pharm. 2001;215:57–65.
Sutton L, Swinehart JM, Cato A, Kaplan AS. A clinical study to determine the efficacy and safety of 1% methotrexate/Azone®(MAZ) gel applied topically once daily in patients with psoriasis vulgaris. Int J Dermatol. 2001;40:464–7.
Ali MFM, Salah M, Rafea M, Saleh N. Liposomal methotrexate hydrogel for treatment of localized psoriasis: preparation, characterization and laser targeting. Med Sci Monit. 2008;14:PI66–74.
Prasad R, Anand S, Koul V. Biophysical assessment of DC iontophoresis and current density on transdermal permeation of methotrexate. Int J Pharm Investig. 2011;1:234.
Lee W-R, Shen S-C, Fang C-L, Zhuo R-Z, Fang J-Y. Topical delivery of methotrexate via skin pretreated with physical enhancement techniques: low-fluence erbium: YAG laser and electroporation. Lasers Surg Med. 2008;40:468–76.
Wong T-W, Zhao Y-L, Sen A, Hui SW. Pilot study of topical delivery of methotrexate by electroporation. Br J Dermatol. 2005;152:524–30.
Stewart WD, Wallace SM, Runikis JO. Absorption and local action of methotrexate in human and mouse skin. Arch Dermatol. 1972;106:357–61.
Taudorf EH, Lerche CM, Vissing A-C, Philipsen PA, Hannibal J, D’Alvise J, et al. Topically applied methotrexate is rapidly delivered into skin by fractional laser ablation. Expert Opin Drug Deliv. 2015;12:1059–69.
Park J-H, Allen MG, Prausnitz MR. Biodegradable polymer microneedles: fabrication, mechanics and transdermal drug delivery. J Control Release. 2005;104:51–66.
Nguyen HX, Banga AK. Enhanced skin delivery of vismodegib by microneedle treatment. Drug Deliv Transl Res. 2015;5:407–23.
Nguyen HX, Banga AK. Fabrication, characterization and application of sugar microneedles for transdermal drug delivery. Ther Deliv. 2017;8:249–64.
Donnelly RF, McCrudden MT, Alkilani AZ, Larrañeta E, McAlister E, Courtenay AJ, et al. Hydrogel-forming microneedles prepared from “super swelling” polymers combined with lyophilised wafers for transdermal drug delivery. PLoS One. 2014;9:e111547.
McCrudden MTC, Alkilani AZ, McCrudden CM, McAlister E, McCarthy HO, Woolfson AD, et al. Design and physicochemical characterisation of novel dissolving polymeric microneedle arrays for transdermal delivery of high dose, low molecular weight drugs. J Control Release. 2014;180:71–80.
Kalluri H, Kolli CS, Banga AK. Characterization of microchannels created by metal microneedles: formation and closure. AAPS J. 2011;13:473–81.
Kolli CS, Banga AK. Characterization of solid maltose microneedles and their use for transdermal delivery. Pharm Res. 2008;25:104–13.
Kalluri H, Banga AK. Formation and closure of microchannels in skin following microporation. Pharm Res. 2011;28:82–94.
Davis SP, Landis BJ, Adams ZH, Allen MG, Prausnitz MR. Insertion of microneedles into skin: measurement and prediction of insertion force and needle fracture force. J Biomech. 2004;37:1155–63.
Hasanovic A, Winkler R, Resch GP, Valenta C. Modification of the conformational skin structure by treatment with liposomal formulations and its correlation to the penetration depth of aciclovir. Eur J Pharm Biopharm Off J Arbeitsgemeinschaft Für Pharm Verfahrenstechnik EV. 2011;79:76–81.
Sviridov AP, Zimnyakov DA, Sinichkin YP, Butvina LN, Omelchenko AJ, Shakh GS, et al. Attenuated total reflection Fourier transform infrared and polarization spectroscopy of in vivo human skin ablated, layer by layer, by erbium:YAG laser. J Biomed Opt. 2004;9:820–7.
Larrañeta E, Moore J, Vicente-Pérez EM, González-Vázquez P, Lutton R, Woolfson AD, et al. A proposed model membrane and test method for microneedle insertion studies. Int J Pharm. 2014;472:65–73.
Enfield J, O’Connell M-L, Lawlor K, Jonathan E, O’Mahony C, Leahy M. In-vivo dynamic characterization of microneedle skin penetration using optical coherence tomography. J Biomed Opt. 2010;15:46001.
Acknowledgments and Disclosures
The authors would like to thank Michelle Vu, College of Pharmacy, Mercer University for her contribution in proof-reading the manuscript. The authors do not have any conflicts of interest to report for this manuscript.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
ESM 1
(DOCX 2764 kb)
Rights and permissions
About this article
Cite this article
Nguyen, H.X., Banga, A.K. Delivery of Methotrexate and Characterization of Skin Treated by Fabricated PLGA Microneedles and Fractional Ablative Laser. Pharm Res 35, 68 (2018). https://doi.org/10.1007/s11095-018-2369-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11095-018-2369-6