ABSTRACT
Purpose
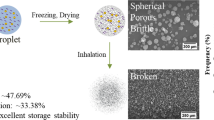
The purpose of this study was to develop inhalable particles that can reach deep into the lungs efficiently independent of inhalation patterns of patients and inhalation devices. We prepared porous particles including L-leucine (Leu), a dispersive agent, by a spray-freeze-drying (SFD) method and examined the influence of inspiratory flow patterns and inhalation devices with various inhalation resistances.
Methods
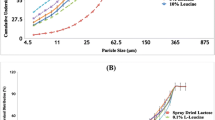
Four types of SFD powder with different Leu contents (0–10%) were prepared. Scanning electron microscopy and laser diffraction were used to measure the morphology and size distribution of the powders. In-vitro inhalation characteristics were determined using a twin-stage liquid impinger equipped with an inspiratory flow pattern simulator. The effects of Leu on the adhesion force and electrostatic property of the particles were evaluated.
Results
The inhalation performance of the powders was improved by the addition of Leu. The powders with Leu showed a high inhalation performance regardless of inspiratory flow patterns and devices. The addition of Leu decreased the adhesion force and increased the surface potential of the powders.
Conclusions
The SFD particles with Leu showed high inhalation performance regardless of the inhalation patterns and devices, which was attributed to the decreased adhesion force between particles and increased dispersibility.










Similar content being viewed by others
Abbreviations
- ANOVA:
-
Analysis of variance
- AUC:
-
Area under the flow rate-time curve
- D50:
-
Geometric mean diameter
- DPI:
-
Dry powder inhaler
- FIR:
-
Flow increase rate
- FlNa:
-
Sodium fluorescein
- Leu:
-
L-leucine
- Man:
-
D-(-)-mannitol
- MMAD:
-
Mass median aerodynamic diameter
- OE:
-
Output efficiency
- PBS:
-
Phosphate buffer solution
- PFR:
-
Peak flow rate
- pMDI:
-
Pressurized metered-dose inhaler
- SEM:
-
Scanning electron microscopy
- SFD:
-
Spray-freeze-drying
- St 2:
-
Stage 2 deposition
- TSLI:
-
Twin-stage liquid impinger
REFERENCES
Dalby R, Suman J. Inhalation therapy: technological milestones in asthma treatment. Adv Drug Deliv Rev. 2003;55(7):779–91.
Adi H, Young PM, Chan HK, Agus H, Traini D. Co-spray-dried mannitol-ciprofloxacin dry powder inhaler formulation for cystic fibrosis and chronic obstructive pulmonary disease. Eur J Pharm Sci. 2010;40(3):239–47.
Ungaro F, d’Emmanuele di Villa Bianca R, Giovino C, Miro A, Sorrentino R, Quaglia F, et al. Insulin-loaded PLGA/cyclodextrin large porous particles with improved aerosolization properties: in vivo deposition and hypoglycaemic activity after delivery to rat lungs. J Control Release. 2009;135(1):25–34.
Timsina MP, Martin GP, Marriott C, Ganderton D, Yianneskis M. Drug delivery to the respiratory tract using dry powder inhalers. Int J Pharm. 1994;101:1–13.
Newman SP, Hollingworth A, Clark R. Effect of different modes of inhalation on drug delivery from a dry powder inhaler. Int J Pharm. 1994;102:127–32.
Borgström L, Bisgaard H, O’Callaghan C, Pedersen S. Dry-powder Inhalers. In: Bisgaard H, O’Callaghan C, Smaldone GC, editors. Drug delivery to the lungs. New York: Marcel Dekker, Inc.; 2002. p. 421–48.
Le VN, Robins E, Flament MP. Agglomerate behaviour of fluticasone propionate within dry powder inhaler formulations. Eur J Pharm Biopharm. 2012;80(3):596–603.
Guenette E, Barrett A, Kraus D, Brody R, Harding L, Magee G. Understanding the effect of lactose particle size on the properties of DPI formulations using experimental design. Int J Pharm. 2009;380(1–2):80–8.
Telko MJ, Hickey AJ. Dry powder inhaler formulation. Respir Care. 2005;50(9):1209–27.
Young PM, Kwork P, Adi H, Chan HK, Traini D. Lactose composite carriers for respiratory delivery. Pharm Res. 2009;26(4):802–10.
Baily MM, Gorman EM, Munson EJ, Berkland C. Pure insulin nanoparticle agglomerates for pulmonary delivery. Lungmuir. 2008;24(33):13614–20.
Raffin RP, Colombo P, Sonvico F, Rossi A, Jornada DS, Pohlmann AR, et al. Agglomerates containing pantoprazole microparticles: modulating the drug release. AAPS PharmSciTech. 2009;10(2):335–45.
Russo P, Sacchetti C, Pasquali I, Bettini R, Massimo G, Colombo P, et al. Primary microparticles and agglomerates of morphine for nasal insufflation. J Pharm Sci. 2006;95(12):2553–61.
Adi H, Larson I, Chiou H, Young P, Traini D, Stewart P. Agglomerate strength and dispersion of salmeterol xinafoate from powder mixtures for inhalation. Pharm Res. 2006;23(11):2556–65.
Iida K, Hayakawa Y, Okamoto H, Danjo K, Leuenberger H. Preparation of dry powder inhalation by surface treatment of lactose carrier particles. Chem Pharm Bull (Tokyo). 2003;51(1):1–5.
de Boer AH, Chan HK, Price R. A critical view on lactose-based drug formulation and device studies for dry powder inhalation: which are relevant and what interactions to expect? Adv Drug Deliv Rev. 2012;64(3):257–74.
Edwards DA, Hanes J, Caponetti G, Hrkach J, Ben-Jebria A, Eskew ML, et al. Large porous particles for pulmonary drug delivery. Science. 1997;276(5320):1868–71.
Edwards DA, Ben-Jebria A, Langer R. Recent advances in pulmonary drug delivery using large, porous inhaled particles. J Appl Physiol (1985). 1998;85(2):379–85.
Vanbever R, Mintzes JD, Wang J, Nice J, Chen D, Batycky R, et al. Formulation and physical characterization of large porous particles for inhalation. Pharm Res. 1999;16(11):1735–42.
Mohri K, Okuda T, Mori A, Danjo K, Okamoto H. Optimized pulmonary gene transfection in mice by spray-freeze dried powder inhalation. J Control Release. 2010;144(2):221–6.
Chew NY, Shekunov BY, Tong HH, Chow AH, Savage C, Wu J, et al. Effect of amino acids on the dispersion of disodium cromoglycate powders. J Pharm Sci. 2005;94(10):2289–300.
Li HY, Seville PC, Williamson IJ, Birchall JC. The use of amino acids to enhance the aerosolisation of spray-dried powders for pulmonary gene therapy. J Gene Med. 2005;7(3):343–53.
Ungaro F, Giovino C, Coletta C, Sorrentino R, Miro A, Quaglia F. Engineering gas-foamed large porous particles for efficient local delivery of macromolecules to the lung. Eur J Pharm Sci. 2010;41(1):60–70.
Duan J, Vogt FG, Li X, Hayes Jr D, Mansour HM. Design, characterization, and aerosolization of organic solution advanced spray-dried moxifloxacin and ofloxacin dipalmitoylphosphatidylcholine (DPPC) microparticulate/nanoparticulate powders for pulmonary inhalation aerosol delivery. Int J Nanomedicine. 2013;8:3489–505.
Lohrmann M, Kappl M, Butt HJ, Urbanetz NA, Lippold BC. Adhesion forces in interactive mixtures for dry powder inhalers-evaluation of a new measuring method. Eur J Pharm Biopharm. 2007;67(2):579–86.
Malmberg LP, Rytilä P, Happonen P, Haahtela T. Inspiratory flows through dry powder inhaler in chronic obstructive pulmonary disease: age and gender rather than severity matters. Int J Chron Obstruct Pulmon Dis. 2010;5:257–62.
Kanabuchi K, Kondo T, Tanigaki T, Tajiri S, Hayama N, Takahari Y, et al. Minimal inspiratory flow from dry powder inhalers according to a biphasic model of pressure vs. flow relationship. Tokai J Exp Clin Med. 2011;36(1):1–4.
Newman SP, Busse WW. Evolution of dry powder inhaler design, formulation, and performance. Respir Med. 2002;96(5):293–304.
Stocks J, Hislop AA. Structure and function on the respiratory system. In: Bisgaard H, O’Callaghan C, Smaldone GC, editors. Drug delivery to the lungs. New York: Marcel Dekker, Inc.; 2002. p. 47–104.
Okamoto H, Nishida S, Todo H, Sakakura Y, Iida K, Danjo K. Pulmonary gene delivery by chitosan-pDNA complex powder prepared with supercritical carbon dioxide. J Pharm Sci. 2003;92(2):371–80.
Hira D, Okuda T, Kito D, Ishizeki K, Okada T, Okamoto H. Inhalation performance of physically mixed dry powders evaluated with a simple simulator for human inspiratory flow patterns. Pharm Res. 2010;27:2131–40.
Hira D, Okuda T, Ichihashi M, Mizutani A, Ishizeki K, Okada T, et al. Influence of peak inspiratory flow rate and pressure drop on inhalation property of dry powder inhalers. Chem Pharm Bull. 2012;60(3):341–7.
Bürki K, Jeon I, Arpagaus C, Betz G. New insights into respirable protein powder preparation using a nano spray dryer. Int J Pharm. 2011;408(1–2):248–56.
Geller DE, Weers J, Heuerding S. Development of an inhaled dry-powder formulation of tobramycin using PulmoSphere™ technology. J Aerosol Med Pulm Drug Deliv. 2011;24(4):175–82.
Nolan LM, Tajber L, McDonald BF, Barham AS, Corrigan OI, Healy AM. Excipient-free nanoporous microparticles of budesonide for pulmonary delivery. Eur J Pharm Sci. 2009;37(5):593–602.
Claus S, Schoenbrodt T, Weiler C, Friess W. Novel dry powder inhalation system based on dispersion of lyophilisates. Eur J Pharm Sci. 2011;43(1–2):32–40.
Bouchard A, Jovanović N, Hofland GW, Jiskoot W, Mendes E, Crommelin DJ, et al. Supercritical fluid drying of carbohydrates: selection of suitable excipients and process conditions. Eur J Pharm Biopharm. 2008;68(3):781–94.
Reverchon E, Della Porta G, Pallado P. Supercritical antisolvent precipitation of salbutamol microparticles. Powder Technol. 2001;114:17–22.
Hoe S, Ivey JW, Boraey MA, Shamsaddini-Shahrbabak A, Javaheri E, Matinkhoo S, et al. Use of a fundamental approach to spray-drying formulation design to facilitate the development of multi-component dry powder aerosols for respiratory drug delivery. Pharm Res. 2014;31(2):449–65.
Yang JJ, Liu CY, Quan LH, Liao YH. Preparation and in vitro aerosol performance of spray-dried Shuang-Huang-Lian corrugated particles in carrier-based dry powder inhalers. AAPS PharmSciTech. 2012;13(3):816–25.
ACKNOWLEDGMENTS AND DISCLOSURES
This study was supported by Adaptable and Seamless Technology Transfer Program through target-driven R&D, Japan Science and Technology Agency (JST). We thank Hitachi Automotive Systems, Co., Ltd., for supplying inspiratory flow meter and inhalation devices.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Otake, H., Okuda, T., Hira, D. et al. Inhalable Spray-Freeze-Dried Powder with L-Leucine that Delivers Particles Independent of Inspiratory Flow Pattern and Inhalation Device. Pharm Res 33, 922–931 (2016). https://doi.org/10.1007/s11095-015-1838-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11095-015-1838-4