Abstract
COVID-19 is a highly infectious disease, and in very recent times, it has shown a massive impact throughout the globe. Several countries faced the COVID-19 infection waves multiple times. These later waves are more aggressive than the first wave and drastically impact social and economic factors. We developed a mechanistic model with imperfect lockdown effect, reinfection, transmission variability between symptomatic & asymptomatic, and media awareness to focus on the early detection of multiple waves and their control measures. Using daily COVID-19 cases data from six states of India, we estimated several important model parameters. Moreover, we estimated the home quarantine, community, and basic reproduction numbers. We developed an algorithm to carry out global sensitivity analysis (Sobol) of the parameters that influence the number of COVID-19 waves (\(W_\mathrm{C}\)) and the average number of COVID-19 cases in a wave (\(A_\mathrm{W}\)). We have identified some critical controlling parameters that mainly influenced \(W_\mathrm{C}\) and \(A_\mathrm{W}\). Our study also revealed the best COVID-19 control strategy/strategies among vaccination, media awareness, and their combination using an optimal cost-effective study. The detailed analysis suggests that the severity of asymptomatic transmission is around 10% to 29% of that of symptomatic transmission in all six locations. About 1% to 4% of the total population under lockdown may contribute to new COVID-19 infection in all six locations. Optimal cost-effective analysis based on interventions, namely only vaccination (VA), only media awareness (ME), and a combination of vaccination & media (VA+ME), are projected for the period March 14, 2020, to August 31, 2021, for all the six locations. We have found that a large percentage of the population (26% to 45%) must be vaccinated from February 13 to August 31, 2021, to avert an optimal number of COVID-19 cases in these six locations.
Similar content being viewed by others
1 Introduction
In December 2019, novel coronavirus disease 2019 (COVID-19) caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) was first observed in Wuhan, China, and spread all over the world in a very short duration [64]. The World Health Organization (WHO) carefully examined various characteristics of COVID-19 and declares this outbreak as a pandemic [65]. As of January 23, 2022, more than 352.2 million confirmed cases and over 5.6 million deaths in more than 220 countries and territories due to COVID-19 are reported across the globe [22]. Moreover, 39.5 million confirmed cases and 4.8 lakh deaths due to COVID-19 are reported in India in the same period [22]. Mainly five subtypes of coronaviruses have been identified, e.g., Alpha, Beta, Gamma, Delta, and Omicron, and SARS-CoV-2 is a form of Beta coronavirus [18, 46, 54].
The initial impact of COVID-19 was catastrophic for almost all countries throughout the globe. As a preventive measure, most of the countries implemented a complete or partial lockdown together with several other preventive measures such as wearing a mask, social distancing, etc., to reduce the contact rate. However, after a certain time, i.e., at the end of the first wave, most of the countries lifted strict lockdown and other measures, which probably leads to other waves of infection. These later waves are more aggressive than the first wave and have a drastic impact on social and economic factors [61]. Currently, COVID-19 multiple waves hit several countries like the USA, India, Brazil, Russia, France, etc. Various studies deal with the causes, prevention, and projection of multiple waves as it has a very calamitous impact on a country. Kaxiras et al. [27] studied the impact of different social distancing factors on multiple waves of COVID-19. A multiple wave model was developed and analyzed the data from several countries in multiple wave scenarios. They also studied the peak intensities of the waves and concluded about the effectiveness of various intervention measures. In their paper, Leung et al. [34] studied a SIR model and discussed the possibility of a second wave based on the relaxation of some preventive measures after the first wave of COVID-19 infection. They have suggested that effective reproduction rate and confirmed case-fatality risk are two critical factors to control the second wave. Hassan and Mahmoud [19] considered a modified SEIR model and studied the impact of COVID-19 multiple waves on US healthcare networks, causes from states reopening during the Fall and Winter seasons. They have observed that the hospitalized cases drastically rise in several regions during the second and third waves. They also showed that protective measures play a vital role and soften these may cause other waves of uncontrollable disease spread in some countries. Cheetham et al. [7] predicted the optimal level of social distancing that could prevent further COVID-19 waves. They warned against the complete lifting of the lockdown after the first wave and projected about a more severe second wave based on the intensive levels of social contact.
Awareness of the people through media is a powerful tool to curb the disease propagation during an infectious disease outbreak [29, 53]. It has already been established that media awareness changes the population behavior, which leads to modifying the disease spread [43, 69]. As COVID-19 is a highly infectious disease, the role of media is a crucial controlling factor during this pandemic period. Media reporting helps the people to gain knowledge about COVID-19 and act accordingly by taking various protecting measures (e.g., wearing masks, keeping social distancing, sanitization, etc.) to save themselves as well as the community [15]. Many studies focused on the impact of media awareness and suggested that it is a very effective non-pharmaceutical intervention in the absence of vaccines. Although there are recently various vaccines available, the continuous flow of media awareness is needed to control the spread of COVID-19 completely. In their paper, Kobey [28] analyzed an SEIR model to study the impact of media awareness programs on the spread of COVID-19 and suggested that the most effective strategies for controlling or eradicating the spread of COVID-19 by isolating a fraction of susceptible from infective. Zhou et al. [69] considered a compartment model with media programs as a separate state variable and suggested that besides improving the medical levels, media coverage may be an effective way to mitigate the disease spreading during the initial stage of an outbreak. Recently, Taki et al. [60] studied a stochastic model to investigate the impact of media awareness on the spread of COVID-19 and studied the disease extinction scenario. They concluded that the media efforts could be helpful to reduce the number of infectives and offer more time to the authorities to react to the global pandemic. In this context, Sooknanan and Mays [57] performed an interesting study based on the contribution of social media in the spread of COVID-19 pandemic.
To eradicate COVID-19 completely, the vaccine is an essential component and its impact together with other interventions must be studied. Apart from non-pharmaceutical interventions, several vaccines have recently been developed and used throughout the globe. However, besides a safe and effective vaccine becomes available, there are several logistical and operational challenges associated with its coverage [13, 41]. Many researchers have recently studied the impact of the vaccine to mainly explore its efficacy, required percentage of the vaccinated population to control the epidemic, vaccine distribution strategy, etc. In their paper, Mukandavire et al. [41] studied a compartmental model to study the vaccine efficacy in South Africa. They concluded that vaccine efficacy of at least 70% and very high coverage is required to control the spread of COVID-19. An extensive study was performed by [24] based on several vaccination strategies and their effect on COVID-19 mortality. An age structure mathematical model was considered by [40] to explore the impact of vaccines with several non-pharmaceutical interventions (NPIs). They concluded that only vaccination could not contain the COVID-19 outbreak, but it may be combined with NPIs to control the disease. In their work, MacIntyre et. al. [39] explored vaccination strategies for COVID-19 and the population herd immunity in the state of New South Wales, Australia. They projected that a vaccine with 90% efficiency can create a herd immunity if at least 66% population are vaccinated. They also added that people should be vaccinated at a very fast rate (e.g., 60,000 doses per day) to gain quick control over the disease. Herd immunity against COVID-19 may not be possible if a vaccine has an efficacy of less than 70%. However, the optimal vaccination strategy is advantageous in this context, but we also need to consider various associated costs in a practical situation. Several articles have been published on the optimal control strategy applied to vaccine administration [36], transmission risk [42], non-pharmaceutical interventions [44], etc., in the context of COVID-19. Since media awareness and vaccination are both effective measures against COVID-19 and have not been explored much, it will be interesting to study the overall optimized cost with both of these interventions.
In the present paper, we developed a new mathematical model on COVID-19 with imperfect lockdown effect, reinfection, transmission variability between symptomatic & asymptomatic, and media awareness. Using daily COVID-19 cases data from six states, namely Andhra Pradesh (AP), Karnataka (KA), Kerala (KL), Maharashtra (MH), Tamil Nadu (TN), and West Bengal (WB), respectively, for the time period March 14, 2020, till May 12, 2021, we estimated several important epidemiological parameters of the new COVID-19 model. To measure the severity of transmission occurring from home-quarantined and community population, we estimated the home-quarantined (symptomatic and asymptomatic) reproduction number, the community (symptomatic and asymptomatic) reproduction number, and the basic reproduction number for the six mentioned locations. We developed an algorithm to carry out a variance based global sensitivity analysis technique based on Sobol’s method to identify key epidemiological model parameter/parameters that influence the number of COVID-19 waves and the average number of COVID-19 cases in a wave in a location. Finally, an optimal cost-effective study is carried out to determine the best COVID-19 control strategy/strategies among vaccination, media awareness, and their combination to reduce the number of COVID-19 cases in the six mentioned locations at a minimum cost.
2 Method
2.1 Model formulation
We developed a mechanistic model on SARS-CoV-2 that focused on studying the mechanism behind multiple COVID-19 waves in six Indian states, namely Andhra Pradesh (AP), Karnataka (KA), Kerala (KL), Maharashtra (MH), Tamil Nadu (TN), and West Bengal (WB). We assume the total human population in a location are subdivided into seven mutually exclusive subclasses Susceptible (S), Home-quarantined (\(S_{L}\)), Exposed (E), Asymptomatic (\(I_{A}\)), Symptomatic (\(I_{S}\)), Notified cases (H), and Recovered (R). As COVID-19 is a highly contagion disease, therefore, it is expected that Awareness campaigns (e.g. TV, Newspapers, Social media, Govt. camps, etc.) will gradually increase as the disease progress over time [14, 23, 45]. Therefore, we also considered a Media & awareness density compartment (M) in addition to the human compartments.
Furthermore, the COVID-19 model developed in this manuscript is an extension of our earlier work [50]. Below we provided the point-wise extension of the previous work [50]:
-
1.
We considered a fraction (\(\theta \)) of the home-quarantined population (\(S_{L}\)) maintain proper social distancing and therefore do not mix with the community. Thus, remaining fraction (\(1-\theta \)) of \(S_{L}\) can mix within the community, therefore, getting infection in contact with community symptomatic (\(I_{S}\)) and asymptomatic (\(I_{A}\)).
-
2.
At the beginning of the epidemic, high density of awareness campaign leads to a larger percentage of the home-quarantined population. However, we assume that this percentage approaches a constant value as the disease progresses. Therefore, we have modified the bilinear awareness response function considered in Kumar et al. [30] by considering a saturating awareness response function \(\frac{\psi S M}{1+M}\), where \(\psi \) is the awareness response intensity of the susceptible individuals.
-
3.
Reinfection with COVID-19 can be possible after exposure to a high virus load [1, 12]. Prolonged virus shedding could be found among COVID-19 recovered patients [35, 38], and therefore, they are advised to home isolation after the recovery. Therefore, we assume that a fraction of the recovered population (R) moved to the home-quarantined compartment (\(S_{L}\)) after the period (\(\frac{1}{\omega _\mathrm{r}}\)) of natural immunity.
-
4.
we assume that a fraction \((\xi )\) of the COVID-19 notified cases (H) are critical patients, and they required treatment. Natural recovery rate (\(\gamma _{2}\)) of the treated person modified by relative rate of recovery \(\lambda \). Currently, there is no effective medicine for the COVID-19. Therefore, we assume that the modification parameter \(\lambda \) is greater than zero. Furthermore, we also assume that non-critical fraction \((1-\xi )\) of the notified cases get natural recovery at a rate \(\gamma _{2}\).
-
5.
Awareness density (M) increases in proportion to a number of notified COVID-19 patients (H) in the population. With a limited budget to carry out an awareness campaign, we assume a saturated type growth rate of awareness density (M). We assume that the awareness campaign degraded at a rate d.
Therefore, following [50] and the assumptions (1) to (5), we have the following system of equation that represent the dynamics of COVID-19:
All the parameters and their biological interpretation are provided in Table 1. Furthermore, a flow diagram of the model (2.1) is provided in Fig. 1.
In A, C and E (fist column) we have plotted daily confirmed cases (C) derived from the model (2.1) and it represents the first wave (A), beginning of the second wave (C) and a complete second wave (E), respectively. In B, D and F (second column) we have plotted \(\frac{\mathrm{d}C}{\mathrm{d}t}\) and we counted the number of sign changes (red circle) in the time series of \(\frac{\mathrm{d}C}{\mathrm{d}t}\). (Colour figure online)
2.2 Some dynamical properties of the model (2.1)
We found that every forward solution of the COVID-19 system (2.1) is positively invariant and bounded (see Supplementary Appendix). Using the next-generation matrix method [63], we analytically determine the basic reproduction number (\(R_{0}\)) for the system (2.1) [see Supplementary Appendix]. Furthermore, the model (2.1) has an unique disease-free equilibrium (\(E_{0}\)), and it is locally asymptotically stable (LAS) if \(R_{0} < 1\) (see Supplementary Appendix). Due to complexity of the system (2.1), we were unable to show analytically the existence and LAS of the endemic equilibrium (\(E_*=(S^*,S_L^*,E^*,I_A^*,I_S^*,H^*,R^*,M^*)\)) of the system (2.1). Therefore, we numerically show the existence and LAS of \(E_*\) by varying two key epidemiological parameters, namely the average symptomatic transmission rate (\(\beta \)), and the average notification & hospitalization rate (\(\tau \)) to their corresponding ranges (see Table 1).
2.3 Data
Daily COVID-19 confirmed cases for the six Indian states Andhra Pradesh (AP), Karnataka (KA), Kerala (KL), Maharashtra (MH), Tamil Nadu (TN), and West Bengal (WB) were collected [21] for the time period March 14, 2020, to May 12, 2021. State-wise demographic data were obtained from [37, 58].
2.4 Estimation of parameters
Several Model (2.1) parameters are estimated (see Table 1) for the mentioned seven locations using daily confirmed COVID-19 cases. An elaboration of the estimation procedure is discussed in [49, 50].
2.5 Basic reproduction number
The basic reproduction number (\(R_{0}\)) for the basic COVID-19 model (2.1) has the following expression (see Supplementary Appendix):
To distinguish the transmission occurring from community, home-quarantined, symptomatic, asymptomatic infected population, we define the following reproduction numbers:
-
Asymptomatic community reproduction number (\(R_{A}^{C}\)):
$$\begin{aligned} \begin{array}{cccc} \displaystyle {R_{A}^{C}} &{}=&{} \displaystyle \frac{\sigma \beta \left( \mu + \omega \right) }{\left( \mu + \sigma \right) \left[ \mu + \omega + (1-\theta ) l\right] } \frac{\chi \rho }{\left( \mu + \gamma _1\right) }.\\ \end{array}\nonumber \\ \end{aligned}$$(2.3) -
Symptomatic community reproduction number (\(R_{S}^{C}\)):
$$\begin{aligned} \begin{array}{cccc} \displaystyle {R_{S}^{C}} &{}=&{} \displaystyle \frac{\sigma \beta \left( \mu + \omega \right) }{\left( \mu + \sigma \right) \left[ \mu + \omega + (1-\theta ) l\right] } \frac{\left( 1-\chi \right) }{\left( \mu + \gamma _2 + \tau \right) }.\\ \end{array}\nonumber \\ \end{aligned}$$(2.4) -
Asymptomatic home-quarantined reproduction number (\(R_{A}^{H}\)):
$$\begin{aligned} \begin{array}{cccc} \displaystyle {R_{A}^{H}} &{}=&{} \displaystyle \frac{\sigma \beta \left( 1-\theta \right) l}{\left( \mu + \sigma \right) \left[ \mu + \omega + (1-\theta ) l\right] } \frac{\chi \rho }{\left( \mu + \gamma _1\right) }.\\ \\ \end{array}\nonumber \\ \end{aligned}$$(2.5) -
Symptomatic home-quarantined reproduction number (\(R_{S}^{H}\)):
$$\begin{aligned} \begin{array}{cccc} \displaystyle {R_{S}^{H}} &{}=&{} \displaystyle \frac{\sigma \beta \left( 1-\theta \right) l}{\left( \mu + \sigma \right) \left[ \mu + \omega + (1-\theta ) l\right] } \frac{\left( 1-\chi \right) }{\left( \mu + \gamma _2 + \tau \right) }.\\ \end{array}\nonumber \\ \end{aligned}$$(2.6)
It can be easily verified that \(R_{0} = R_{A}^{C} + R_{S}^{C} + R_{A}^{H} + R_{S}^{H}\).
2.6 Exploring multiple COVID-19 waves
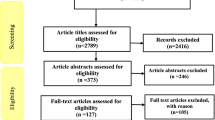
One of the main aims of this study is to identify which model (2.1) parameters are most influencing on the multiple waves in the dynamics of COVID-19 in these six states. To explore more on this, we carried out Sobol global sensitivity analysis [25, 55] of these parameters with the number of COVID-19 waves during a time period (\(W_\mathrm{C}\)) and the average number of cases in a wave (\(A_\mathrm{W}\)). We derived \(W_\mathrm{C}\) for a particular duration of the epidemic by counting the number of sign changes in the rate of change of daily confirmed cases (C). In Fig. 2A, time series of the daily confirmed cases (C) shows the first wave and \(\frac{\mathrm{d}C}{\mathrm{d}t}\) (see Fig. 2B) suggest one sign change. Similarly, the time series of the daily confirmed cases (C) in Fig. 2C suggests completion of the first wave and starting of the second wave. Corresponding in Fig. 2D suggests two sign changes in the time series of \(\frac{\mathrm{d}C}{\mathrm{d}t}\). Finally, Fig. 2E depicts completion of the second wave, and Fig. 2F shows three sign changes in the time series of \(\frac{\mathrm{d}C}{\mathrm{d}t}\). Sign changes of the time series in \(\frac{\mathrm{d}C}{\mathrm{d}t}\) in Fig. 2 lead us to develop the algorithm to compute \(W_\mathrm{C}\) as follows:
-
To neglect some initial fluctuations, we remove first 20 time points of the daily confirmed cases (C) simulation obtained from the COVID-19 model (2.1).
-
If \(sign change = 1\), then the first wave of the COVID-19 will be observed within the time period and therefore \(W_\mathrm{C} =1\).
-
If \(2 \le sign change \le 3\), then the second wave of the COVID-19 will be observed within the time period and therefore \(W_\mathrm{C} =2\)
-
If \(4 \le sign change \le 5\), then the third wave of the COVID-19 will be observed within the time period and therefore \(W_\mathrm{C} =3\)
-
If \(6 \le sign change \le 7\), then the fourth wave of the COVID-19 will be observed within the time period and therefore \(W_\mathrm{C} =4\)
-
This process will be continued for further waves of COVID-19.
Finally, the average number of cases in a wave (\(A_\mathrm{W}\)) is computed using the following formula:
2.7 Global sensitivity analysis
We determine the first-order (\(S_{i}\)) and total order (\(S_{T_{i}}\)) Sobol sensitivity index [25, 55] of the parameters Average transmission rate of symptomatic COVID-19 infected (\(\beta \)), Transmission variability factor between symptomatic and asymptomatic infection (\(\rho \)), Awareness response intensity (\(\psi \)), Fraction of home-quarantined population who maintain social distancing (\(\theta \)), Period of natural immunity in COVID-19 (\(\frac{1}{\omega _\mathrm{r}}\)), Fraction of asymptomatic infected in the population (\(\chi \)), and Average notification rate (\(\tau \)) with responses the number of COVID-19 waves during a time period (\(W_\mathrm{C}\)) and the average number of cases in a wave (\(A_\mathrm{W}\)), respectively. We prefer to use global sensitivity based on Sobol indices as the responses \(W_\mathrm{C}\) and \(A_\mathrm{W}\) have a nonlinear non-monotone relationship with the mentioned parameters.
2.8 Model with vaccination
To determine an optimal COVID-19 vaccination and media awareness strategy, we incorporate the effect of vaccination in our model. We assumed that at time t, a fraction p(t) of the susceptible and home-quarantined population are vaccinated (2 doses of Covishield) with vaccine efficacy \(\zeta \). Those vaccinated individuals in susceptible and home-quarantined compartments move to the recovered compartment. As vaccination may not be able to life-long immunity against COVID-19 [48], therefore, we assume vaccine-based immunity wanes at a rate \(\omega _\mathrm{r}\). We considered the time-dependent rate of awareness response \(\psi (t)\) to optimize the awareness response. Based on these assumptions, the extension of the model (2.1) is given as follows:
2.9 Optimal cost-effectiveness strategy
One of the focuses of this study is to reduce COVID-19 cases at a minimum implementation cost of vaccination and awareness campaigns. In India, the first phase of vaccination started on January 16, 2021 [10]. However, in our COVID-19 model (2.8), we have considered the effect of full vaccination (a person received two doses of COVID-19 vaccine). The second dose of vaccination is started in India on February 13, 2021 [51]. Therefore, we carried out optimal vaccination effects from February 13, 2021, to August 31, 2021. However, the effect of awareness was studied from March 14, 2020, up to August 31, 2021. The difference in an awareness campaign with vaccination coverage is that the media campaign started as soon as the COVID-19 cases were observed in the country. To attain this goal, we constructed the following objective function:
where \(A_1\), \(A_{2}\), and \(A_{3}\) are provided in Table 2. The first integrand in (2.9) represents the cost of COVID-19-related deaths [49]. The second integrand represents cost incurred in the process of information transmission [30]. The third integrand represents cost of vaccination [26].
Model (2.1) to the daily COVID-19 cases from six states in India for the time period March 14, 2020, to May 12, 2021. Observed cases are in blue circle, and black line is the model solution. Here, subscripts AP, KA, KL, MH, TN, and WB are Andhra Pradesh, Karnataka, Kerala, Maharashtra, Tamil Nadu, and West Bengal, respectively
We aim to minimize J with respect to vaccination rate p(t) and awareness response rate \( \psi (t)\) using Pontryagin’s maximum principle [30, 49]. The minimization technique of the objective function J is discussed in Supplementary Appendix. We determine the daily average awareness response rate \(\hat{\psi }\) (from March 14, 2020, up to August 31, 2021), the daily average vaccination rate \(\hat{p}\) (from February 13, 2021, up to August 31, 2021), and the total vaccination coverage \(\hat{p}_{T}\) (from February 13, 2021, up to August 31, 2021) in six locations (AP, KA, KL, MH, TN, and WB) using the following formulae:
3 Results
Model (2.1) fitting to the daily COVID-19 cases from the six locations, namely Andhra Pradesh (AP), Karnataka (KA), Kerala (KL), Maharashtra (MH), Tamil Nadu (TN), and West Bengal (WB) for the time period March 14, 2020, to May 12, 2021, is provided in Fig. 3. It is clear from Fig. 3 that the basic COVID-19 model (2.1) can capture the trend of the second waves in those six locations quite well. The estimated value of the symptomatic transmission rate (\(\beta \)) and variability factor between symptomatic and asymptomatic disease transmission (\(\rho \)) suggest that the severity of asymptomatic transmission is around 10% to 30% of the symptomatic transmission in all the six locations (see Table 3). Estimate of the fraction of home quarantined population who maintain social distancing, \(\theta \) (see Table 3), suggests that in all six locations, about 1% to 4% of the total population under lockdown may contribute to new COVID-19 infection. Furthermore, the estimate of the percentage of asymptomatic infected (\(\chi \)) was found to be higher than the percentage of symptomatic infected (see Table 3) in three locations, namely AP, MH, and WB, respectively. This suggests that the majority of COVID-19 cases in these three locations were undetected. Opposite trends were observed in KA, KL and TN, respectively. The recovery modification factor (\(\lambda \)) in all the six locations was less than unity (see Table 3). Therefore, our result indicates that hospitalized patients have a slower recovery rate compared to the natural recovery rate of the community symptomatic infected persons (\(\gamma _{2}\)) in five locations AP, KL, MH, TN, and WB, respectively (see Table 3).
Estimate of different reproduction numbers, \(R_{A}^{C}\) (asymptomatic community reproduction number), \(R_{S}^{C}\) (symptomatic community reproduction number), \(R_{A}^{H}\) (asymptomatic home quarantined reproduction number), \(R_{S}^{H}\) (symptomatic home quarantined reproduction number), and \(R_{0}\) (the basic reproduction number), suggested that COVID-19 transmission dominated by the community infection (see Table 4). This result is consistent with the fact that only 1% to 4% percentage of home quarantined population may contribute to new COVID-19 infection (see estimate of \(\theta \) in Table 3). In WB community, infection is dominated by asymptomatic infection (\(R_{A}^{C} > R_{S}^{C}\)), whereas in other five locations (AP, KA, KL, MH, and TN) community, symptomatic infection is dominating (see Table 4). Opposite trend observed in WB is due to higher percentage of asymptomatic infection in the population (see value of \(\chi \) in Table 3) and higher value of the transmission variability between symptomatic and asymptomatic (see value of \(\rho \) in Table 3).
The first-order and total order Sobol sensitivity index of some of the model (2.1) parameters with number COVID-19 waves (\(W_\mathrm{C}\)) during the time period March 14, 2020, to May 12, 2021
The first-order and total order Sobol sensitivity index of some of the model (2.1) parameters with average number COVID-19 cases in a wave (\(A_\mathrm{W}\)) for the time period March 14, 2020, to May 12, 2021
Three key parameters that mainly influence (value of the total order Sobol sensitivity index) the number of COVID-19 waves (\(W_\mathrm{C}\)) in all six locations (AP, KA, KL, MH, TN, and WB) are the average transmission rate of symptomatic COVID-19 infected (\(\beta \)), the average notifications & hospitalization rate (\(\tau \)) and the variability in transmission between symptomatic and asymptomatic (\(\rho \)) [see Fig. 4]. Similar to \(W_\mathrm{C}\), the average number cases in a COVID-19 waves (\(A_\mathrm{W}\)) mainly influenced by \(\beta \) (see Fig. 5). Furthermore, other parameters like \(\theta \) (fraction of home-quarantined population who maintain proper social distancing), \(\omega _\mathrm{r}\) (rate of loss of natural immunity of COVID-19), \(\chi \) (average fraction of the COVID-19 exposed population that become asymptotic infected) and \(\tau \) also have similar impact on \(A_\mathrm{W}\) (see Fig. 5). Therefore, policymakers should focus on controlling these six parameters (\(\beta \), \(\tau \), \(\rho \), \(\theta \), \(\omega _\mathrm{r}\), and \(\chi \)) to restrict further COVID-19 waves and reduce number of cases in a wave in these six locations, namely MH, TN, KA, KL, AP, and WB.
Optimal effect of the interventions vaccination, awareness and their combination are compared in terms of cases reduction (see Table 5) and also total implementation cost (see Table 8). In Table 5, base cases are projected for the period March 14, 2020, to August 31, 2021, for six locations MH, KL, TN, AP, WB, and KA using the basic COVID-19 model (2.1) (with fixed awareness rate \(\psi \)). Optimal cases based on interventions, namely only vaccination (VA), only media awareness (ME), and combination of vaccination & media (VA+ME), are projected for the time period March 14, 2020, to August 31, 2021, for the mentioned six locations (see Table 5). Optimal vaccination effects (VA and VA+ME) are studied from February 13, 2021, onwards in these mentioned six locations. This is because India’s second dose of vaccination (Covishield) started on February 13, 2021. Our result suggests that only vaccination (without any awareness) is not at all effective in reducing COVID-19 cases in all six states (see Table 5). The optimal effect of media awareness (ME) (see Table 5, and Table 8) is found to be most cost-effective (in terms of implementation cost and cases reduction) in AP (about 22% reduction from the base cases), TN (about 29% reduction compared to base cases) and KA (about 54% reduction compared to base cases). In KL, and MH, awareness is also found to have a significant impact (about 20% to 30% reduction from the base cases) in cases reduction (see Table 5). Applying only media awareness (ME) is not found to be effective in WB in terms of cases reduction. Optimal awareness & vaccination combination (VA+ME) found to be most cost-effective (in terms of implementation cost and cases reduction) in MH (about 97% reduction from the base cases), KL (about 87% reduction from the base cases), and WB (about 74% reduction from the base cases) [see Table 5). In Tables 6 and 7, we have provided average optimal rates at which awareness campaigns and vaccination may be carried out in the six locations MH, KL, TN, AP, WB, KA, respectively. Our results suggest that a large percentage of the population (26% to 45%) must be vaccinated from February 13, 2021, to August 31, 2021, in order to avert an optimal number of COVID-19 cases in these six locations (see Table 7).
4 Discussion
In this paper, we considered a new COVID-19 mathematical model (2.1) with imperfect lockdown effect, reinfection of recovered COVID-19 cases, and media awareness. We have analyzed the invariance and boundedness of the solution. The local asymptotic stability of the disease-free equilibrium (DFE) has been studied analytically with the help of the next-generation matrix technique. Due to the high nonlinearity of the model, we have analyzed the model numerically to find all possible equilibrium points and studied their local stability analysis. Several parameters are estimated by the fitting solution of the model (2.1) to daily notified cases for the time period March 14, 2020, till May 12, 2021, from six states, namely Andhra Pradesh (AP), Karnataka (KA), Kerala (KL), Maharashtra (MH), Tamil Nadu (TN), and West Bengal (WB), respectively. We estimated (see Table 4) the community (symptomatic and asymptomatic) reproduction number (\(R_{S}^{C}\) and \(R_{A}^{C}\)), the home quarantined (symptomatic and asymptomatic) reproduction number (\(R_{S}^{H}\) and \(R_{A}^{H}\)), the basic reproduction number (\(R_{0}\)) for the six mentioned states, respectively. To determine a relationship between model (2.1) parameters with the number of COVID-19 waves (\(W_\mathrm{C}\)) and the average number of notified cases in a wave (\(A_\mathrm{W}\)), we develop an algorithm to count the number of waves and the average notified cases for the six location from the solution of the model (2.1). Using this algorithm, we perform a variance-based global sensitivity analysis based on Sobol’s method of seven key epidemiological parameters of the model (2.1) with two responses, namely \(W_\mathrm{C}\) and \(A_\mathrm{W}\), respectively. Moreover, the model (2.1) is then extended to carry out an optimal cost-effective study of some important COVID-19 control strategies (awareness, vaccination, and their combination) in terms of cases reduction and their implementation cost. Our results suggest that a negligible percentage (about 1% to 4%) of COVID-19 transmission occurs from the home-quarantined population. Thus, in these six states, COVID-19 transmission is dominated by community infection. Our analysis suggest that the asymptomatic transmission is less severe (approximately 10% to 30% of the average symptomatic transmission rate) than the symptomatic transmission (see Table 3) in all six locations. This result also reflected in the estimation of community (\(R_{A}^{C}\), and \(R_{S}^{C}\)) and home-quarantined (\(R_{A}^{H}\), and \(R_{S}^{H}\)) reproduction numbers. Results on global sensitivity analysis of model parameters suggest that \(\beta \), \(\tau \), and \(\rho \) are mainly influence the number of COVID-19 waves in the six locations. Optimal use of vaccination and media awareness will reduce the effect of \(\beta \) and \(\rho \). Furthermore, rapid COVID-19 testing will reduce the effect of \(\tau \). Therefore, policymakers may focus on controlling these parameters to control future COVID-19 waves and the average number of cases in a wave. The optimal cost-effective study suggests that awareness as a single intervention and awareness with a combination of vaccination are the two best control strategies in terms of case reduction and implementation cost. In the case of control combination (media awareness and vaccination), a large percentage of the population must be vaccinated in order to reduce the significant number of COVID-19 cases in the mentioned six locations.
Finally, we discuss some drawbacks of the present study and may be extended in from diverse perspectives. In the COVID-19 system (2.1), we assumed that home-quarantined (due to awareness and lockdown) individuals are all susceptible. However, it is possible that a home-quarantined individuals can be COVID-19 exposed or symptomatic or asymptomatic. Consequently, In our study, we neglect the possibility of cross-infection between different home-quarantined population. Furthermore, in this current manuscript, we have shown analytically local asymptotic stability of the DFE (\(E_{0}\)) [see Supplementary Appendix], and also numerically shown the existence and stability of the endemic equilibrium point of the model (2.1) in terms of the basic reproduction number (\(R_{0}\)). However, we have yet to determine the full analytical stability of the endemic equilibrium point of the COVID-19 model (2.1). We shall explore these challenging problems in our future studies.
Data availability
The authors declare that all data generated or analyzed during this study are included in this article.
References
Ahmadian, S., Fathizadeh, H., Shabestari Khiabani, S., Asgharzadeh, M., Kafil, H.S.: Covid-19 reinfection in a healthcare worker after exposure with high dose of virus: a case report. Clin. Case Rep. 9(6), e04257 (2021)
Anderson, R.M., May, R.M.: Population biology of infectious diseases: part I. Nature 280(5721), 361–367 (1979)
Anderson, R.M., Anderson, B., May, R.M.: Infectious Diseases of Humans: Dynamics and Control. Oxford University Press, Oxford (1992)
AstraZeneca’s COVID-19 vaccine shows effectiveness against Indian variants of SARS-CoV-2 virus. https://www.astrazeneca.com/media-centre/articles/2021/astrazenecas-covid-19-vaccine-shows-effectiveness-against-indian-variants-of-sars-cov-2-virus.html(2021). Retrieved 14 July 2021
Bi, Q., Lessler, J., Eckerle, I., Lauer, S.A., Kaiser, L., Vuilleumier, N., Cummings, D.A., Flahault, A., Petrovic, D., Guessous, I., et al.: Insights into household transmission of SARS-CoV-2 from a population-based serological survey. Nat. Commun. 12(1), 1–8 (2021)
Byrne, A.W., McEvoy, D., Collins, A.B., Hunt, K., Casey, M., Barber, A., Butler, F., Griffin, J., Lane, E.A., McAloon, C., et al.: Inferred duration of infectious period of SARS-CoV-2: rapid scoping review and analysis of available evidence for asymptomatic and symptomatic COVID-19 cases. BMJ Open 10(8), e039856 (2020)
Cheetham, N., Waites, W., Ebyarimpa, I., Leber, W., et al.: Determining the level of social distancing necessary to avoid future COVID-19 epidemic waves: a modelling study for North East London. Sci. Rep. 11, 5806 (2021)
Coroiu, A., Moran, C., Campbell, T., Geller, A.C.: Barriers and facilitators of adherence to social distancing recommendations during COVID-19 among a large international sample of adults. PLoS ONE 15(10), e0239795 (2020)
Coronavirus disease 2019 (COVID-19) Situation Report—46. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200306-sitrep-46-covid-19.pdf (2021). Retrieved 14 July 2021
Coronavirus|First phase of vaccination to start on January 16. https://www.thehindu.com/news/national/india-to-start-covid-19-vaccination-drive-on-jan-16/article33536670.ece (2021). Published on: 9 Jan 2021
da Silva, J.A.T., Tsigaris, P.: Estimating worldwide costs of premature mortalities caused by COVID-19. J. Health Res. 35, 353–358 (2020)
Dan, J.M., Mateus, J., Kato, Y., Hastie, K.M., Yu, E.D., Faliti, C.E., Grifoni, A., Ramirez, S.I., Haupt, S., Frazier, A., et al.: Immunological memory to SARS-CoV-2 assessed for up to 8 months after infection. Science 371(6529), eabf4063 (2021)
Equils, O., Kellogg, C., Baden, L., Berger, W., Connolly, S.: Logistical and structural challenges are the major obstacles for family medicine physicians’ ability to administer adult vaccines. Hum. Vaccines Immunother. 15(3), 637–642 (2019)
Facebook to roll out new campaign in India to fight COVID misinformation. https://www.business-standard.com/article/current-affairs/facebook-to-roll-out-new-campaign-in-india-to-fight-covid-misinformation-1210513009511.html (2021). Published on 13 May 2021
Feng, L., Jing, S., Hu, S., et al.: Modelling the effects of media coverage and quarantine on the COVID-19 infections in the UK. Math. Biosci. Eng. 17(4), 3618–3636 (2020)
Fleming, W.H., Rishel, R.W.: Deterministic and Stochastic Optimal Control, vol. 1. Springer Science & Business Media, Berlin (2012)
Govt spending on publicity an investment for the country’s future. https://www.exchange4media.com/advertising-news/govt-spending-on-publicity-an-investment-for-the-countrys-future-103895.html (2020). Published on 9 April 2020
Gwaltney, J.J.: Virology and immunology of the common cold. Rhinology 23(4), 265–271 (1985)
Hassan, E., Mahmoud, H.: Impact of multiple waves of COVID-19 on healthcare networks in the united states. PLoS ONE 16(3), e0247463 (2021)
Hethcote, H.W.: The mathematics of infectious diseases. SIAM Rev. 42(4), 599–653 (2000)
India COVID-19 Tracker. https://www.covid19india.org/ (2021). Retrieved 14 July 2021
India COVID-19 Tracker. https://www.worldometers.info/coronavirus/ (2021). Accessed on 17 June 2021
Javadekar launches awareness campaign on COVID-19 vaccination, Aatmanirbhar Bharat. https://www.hindustantimes.com/india-news/javadekar-launches-awareness-campaign-on-covid-19-vaccination-101612697229360.html (2021). Published on: 7 Feb 2021
Jentsch, P., Anand, M., Bauch, C.: Prioritising COVID-19 vaccination in changing social and epidemiological landscapes: a mathematical modelling study. Lancet Infect. Dis. (2021). https://doi.org/10.1016/S1473-3099(21)00057-8
Jianyong, W., Dhingra, R., Gambhir, M., Remais, J.V.: Sensitivity analysis of infectious disease models: methods, advances and their application. J. R. Soc. Interface 10(86), 20121018 (2013)
Kassa, S.M., Ouhinou, A.: The impact of self-protective measures in the optimal interventions for controlling infectious diseases of human population. J. Math. Biol. 70(1), 213–236 (2015)
Kaxiras, E., Neofotistos, G.: Multiple epidemic wave model of the COVID-19 pandemic: Modeling study. J. Med. Internet Res. 22(7), e20912 (2020)
Kobe, F.T.: Modelling and analysis of effect of awareness programs by media on the spread of COVID-19 pandemic disease. Math. Comput. Sci. 5(5), 93–102 (2020)
Kristiansen, I., Kristiansen, P.A., Gyrd-Hansen, D.: Influenza pandemic: perception of risk and individual precautions in a general population, cross sectional study. BMC Public Health 7, 48 (2007). https://doi.org/10.1186/1471-2458-7-48
Kumar, A., Srivastava, P.K., Takeuchi, Y.: Modeling the role of information and limited optimal treatment on disease prevalence. J. Theor. Biol. 414, 103–119 (2017)
Lauer, S.A., Grantz, K.H., Bi, Q., Jones, F.K., Zheng, Q., Meredith, H.R., Azman, A.S., Reich, N.G., Lessler, J.: The incubation period of coronavirus disease 2019 (COVID-19) from publicly reported confirmed cases: estimation and application. Ann. Intern. Med. 172(9), 577–582 (2020)
Laxminarayan, R., Wahl, B., Dudala, S.R., Gopal, K., Neelima, S., Jawahar Reddy, K.S., Radhakrishnan, J., Lewnard, J.A., et al.: Epidemiology and transmission dynamics of COVID-19 in two Indian states. Science 370(6517), 691–697 (2020)
Lenhart, S., Workman, J.T.: Optimal Control Applied to Biological Models. Chapman and Hall/CRC, London (2007)
Leung, K., Wu, J., Leung, G.: First-wave COVID-19 transmissibility and severity in china outside Hubei after control measures, and second-wave scenario planning: a modelling impact assessment. Lancet 395, 1382–93 (2020)
Li, N., Wang, X., Lv, T.: Prolonged SARS-CoV-2 RNA shedding: not a rare phenomenon. J. Med. Virol. 92(11), 2286–2287 (2020)
Libotte, G., Lobato, F., Platt, G., Neto, A.: Determination of an optimal control strategy for vaccine administration in COVID-19 pandemic treatment. Comput. Methods Programs Biomed. 196, 105664 (2021)
Life expectancy at birth. https://niti.gov.in/content/life-expectancy (2019). Retrieved 5 April 2020
Liu, W.-D., Chang, S.-Y., Wang, J.-T., Tsai, M.-J., Hung, C.-C., Hsu, C.-L., Chang, S.-C.: Prolonged virus shedding even after seroconversion in a patient with COVID-19. J. Infect. 81(2), 318 (2020)
MacIntyre, C., Costantino, V., Trent, M.: Modelling of COVID-19 vaccination strategies and herd immunity, in scenarios of limited and full vaccine supply in NSW, Australia. Vaccine (2021). https://doi.org/10.1016/j.vaccine.2021.04.042
Moore, S., Hill, E., Tildesley, M., Dyson, L., Keeling, M.: Vaccination and non-pharmaceutical interventions for COVID-19: a mathematical modelling study. Lancet Infect. Dis. 21, 793–802 (2021)
Mukandavire, Z., Nyabadza, F., Malunguza, N., et al.: Quantifying early COVID-19 outbreak transmission in South Africa and exploring vaccine efficacy scenarios. Hum. Vaccines Immunother. 15(7), e0236003 (2020)
Obsu, L., Balcha, S.: Optimal control strategies for the transmission risk of COVID-19. J. Biol. Dyn. 14(1), 590–607 (2020)
Pellis, L., Scarabel, F., Stage, H.B., et al.: Challenges in control of COVID-19: short doubling time and long delay to effect of interventions. Philos. Trans. R. Soc. B 376, 20200264 (2021)
Perkins, T., Espana, G.: Optimal control of the COVID-19 pandemic with non-pharmaceutical interventions. Bull. Math. Biol. 82, 118 (2020). https://doi.org/10.1007/s11538-020-00795-y
PM Modi to launch COVID-19 awareness campaign today. https://www.hindustantimes.com/india-news/pm-modi-to-launch-covid-awareness-campaign/story-she8m3L9YJFpDTf0PQ9VeJ.html (2020). Published on: 8 Oct 2020
Podder, P., Khamparia, A., Mondal, M.R.H.: Forecasting the spread of COVID-19 and ICU requirements. Int. J. Online Biomed. Eng. 17(5), 81–99 (2021)
Pontryagin, L.S.: Mathematical Theory of Optimal Processes. CRC Press, London (1987)
Rubin, R.: COVID-19 vaccines vs variants—determining how much immunity is enough. JAMA 325(13), 1241–1243 (2021)
Sardar, T., Mukhopadhyay, S., Bhowmick, A.R., Chattopadhyay, J.: An optimal cost effectiveness study on Zimbabwe cholera seasonal data from 2008–2011. PLoS ONE 8(12), e81231 (2013)
Sardar, T., Nadim, S.S., Rana, S., Chattopadhyay, J.: Assessment of lockdown effect in some states and overall India: a predictive mathematical study on COVID-19 outbreak. Chaos Solitons Fractals 139, 110078 (2020)
Second COVID-19 vaccine shot to be administered from Feb 13. https://www.hindustantimes.com/india-news/second-covid-19-vaccine-shot-to-be-administered-from-feb-13-101612435498641.html (2021). Published on: 4 Feb 2021
SII sets price tags for Covishield vaccine. https://www.livemint.com/news/india/covishield-to-cost-400-per-dose-for-states-600-for-private-hospitals-11618991072705.html (2021). Published on: 22 April 2021
Silva, U., Warachit, J., Waicharoen, S., Chittaganpitch, M.: A preliminary analysis of the epidemiology of influenza A (H1N1) virus infection in Thailand from early outbreak data. Euresurveilance 14, 1–3 (2009)
Singh, R., Sarsaiya, S., Singh, T.A., Singh, T., et al.: Corona virus (COVID-19) symptoms prevention and treatment: a short review. J. Drug Deliv. Ther. 11(2–s), 118–120 (2021)
Sobol, I.M.: Global sensitivity indices for nonlinear mathematical models and their Monte Carlo estimates. Math. Comput. Simul. 55(1–3), 271–280 (2001)
Soni, P.: Effects of COVID-19 lockdown phases in India: an atmospheric perspective. Environ. Dev. Sustain. 23, 12044–12055 (2021). https://doi.org/10.1007/s10668-020-01156-4
Sooknanan, J., Mays, N.: Harnessing social media in the modelling of pandemics—challenges and opportunities. Bull. Math. Biol. 83, 57 (2021). https://doi.org/10.1007/s11538-021-00895-3
Statewise population data. http://statisticstimes.com/demographics/population-of-indian-states.php (2019). Retrieved 5 April 2020
Subramanian, R., He, Q., Pascual, M.: Quantifying asymptomatic infection and transmission of COVID-19 in New York city using observed cases, serology, and testing capacity. Proc. Natl. Acad. Sci. 118(9), e2019716118 (2021)
Taki, R., Fatini, M., Khalifi, M., et al.: Understanding death risks of COVID-19 under media awareness strategy: a stochastic approach. J. Anal. (2021). https://doi.org/10.1007/s41478-021-00331-8
Taubenberger, J.K., Morens, D.M.: 1918 Influenza: the mother of all pandemics. Emerg. Infect. Dis. 12, 15–22 (2006)
Transmission of SARS-CoV-2: implications for infection prevention precautions. https://www.who.int/news-room/commentaries/detail/transmission-of-sars-cov-2-implications-for-infection-prevention-precautions#:~:text=The%20incubation%20period%20of%20COVID,to%20a%20confirmed%20case (2020). Published on: 9 July 2020
Van den Driessche, P., Watmough, J.: Reproduction numbers and sub-threshold endemic equilibria for compartmental models of disease transmission. Math. Biosci. 180(1–2), 29–48 (2002)
Wang, C., Horby, P.W., Hayden, F.G., Gao, G.F.: A novel coronavirus outbreak of global health concern. The Lancet 395, 470–473 (2020)
WHO Director-General’s opening remarks at the media briefing on COVID-19—11 March 2020. https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 (2020). Published on: 11 March 2020
Yanes-Lane, M., Winters, N., Fregonese, F., Bastos, M., Perlman-Arrow, S., Campbell, J.R., Menzies, D.: Proportion of asymptomatic infection among COVID-19 positive persons and their transmission potential: a systematic review and meta-analysis. PLoS ONE 15(11), e0241536 (2020)
Yang, X., Chen, L., Chen, J.: Permanence and positive periodic solution for the single-species nonautonomous delay diffusive models. Comput. Math. Appl. 32(4), 109–116 (1996)
Zhang, Y., Fan, K., Gao, S., Liu, Y., Chen, S.: Ergodic stationary distribution of a stochastic sirs epidemic model incorporating media coverage and saturated incidence rate. Physica A 514, 671–685 (2019)
Zhou, W., Wang, A., Xia, F., et al.: Effects of media reporting on mitigating spread of COVID-19 in the early phase of the outbreak. Math. Biosci. Eng. 17(3), 2693–2707 (2020)
Funding
The authors have not disclosed any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interests
The authors declare that they have no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sardar, T., Nadim, S.S. & Rana, S. Detection of multiple waves for COVID-19 and its optimal control through media awareness and vaccination: study based on some Indian states. Nonlinear Dyn 111, 1903–1920 (2023). https://doi.org/10.1007/s11071-022-07887-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11071-022-07887-5