Abstract
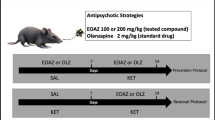
Microglial activation has been associated to the physiopathology of neurodegenerative diseases, such as schizophrenia, and can occur during inflammation and oxidative stress. Pharmacological treatment is associated with severe side effects, and studies for use of plant extracts may offer alternatives with lower toxicity. Harpagophytum procumbens (HP) is a plant known for its anti-inflammatory properties. In the present study, we characterized the ethyl acetate fraction of HP (EAF HP) by ESI-ToF-MS and investigated the effects EAF HP in a lipopolysaccharide (LPS) induced inflammation model on microglial cells (BV-2 lineage). MTT (3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide), DCFH-DA (2′,7′-dichlorofluorescein diacetate) and cell cycle flow cytometer analysis were performed. In vivo was investigated the amphetamine-induced psychosis model through behavioral (locomotor and exploratory activities, stereotypies and working memory) and biochemical (DCFH-DA oxidation and protein thiols) parameters in cortex and striatum of mice. EAF HP reduced activation and proliferation of microglial cells in 48 h (300 µg/mL) and in 72 h after treatments (50–500 µg/mL). Reactive oxygen species levels were lower at the concentration of 100 µg/mL EAF HP. We detected a modulatory effect on the cell cycle, with reduction of cells in S and G2/M phases. In mice, the pre-treatment with EAF HP, for 7 days, protected against positive and cognitive symptoms, as well as stereotypies induced by amphetamine. No oxidative stress was observed in this amphetamine-induced model of psychosis. Such findings suggest that EAF HP can modulate the dopaminergic neurotransmission and be a promising adjuvant in the treatment of locomotor alterations, cognitive deficits, and neuropsychiatric disorders.







Similar content being viewed by others
Data Availability
Enquiries about data availability should be directed to the authors.
References
Nakazawa K (2012) GABAergic interneuron origin of schizophrenia pathophysiology. Neuropharmacology 62(3):1574–1583
Wu JQ, Kosten TR, Zhang XY (2013) Free radicals, antioxidant defense systems, and schizophrenia. Prog Neuropsychopharmacol Biol Psychiatry 46:200–206
Machado AK, Cadoná FC, Assmann CE, Andreazza AC, Duarte MMMF, Branco CS, Zhou X, Souza DV, Da Cruz IBM (2019) Açaí (Euterpe oleracea Mart.) has anti-inflammatory potential through NLRP3-inflammasome modulation. J Funct Foods 56:364–371
Qian S, Golubnitshaja O, Zhan X (2019) Chronic inflammation: key player and biomarker-set to predict and prevent cancer development and progression based on individualized patient profiles. EMPA J 10:365–381
Andreazza AC, Shao L, Wang JF, Young LT (2010) Mitochondrial complex I activity and oxidative damage to mitochondrial proteins in the prefrontal cortex of patients with bipolar disorder. Arch Gen Psychiatry 67:360–368
Feigenson KA, Kusnecov AW, Silverstein SM (2014) Inflammation and the two-hit hypothesis of schizophrenia. Neurosci Biobehav Rev 38:72–93
Monji A, Kato T, Kanba S (2009) Cytokines and schizophrenia: microglia hypothesis of schizophrenia. Psychiatry Clin Neurosci 63:257–265
Asai H, Inoue K, Sakuma E, Shinohara Y, Ueki T (2018) Potential implication of SGK1-dependent activity change in BV-2 microglial cells. Int J Physiol Pathophysiol Pharmacol 10:115–123
Koga M, Serritella AV, Sawa A, Sedlak TW (2016) Implications for reactive oxygen species in schizophrenia pathogenesis. Schizophr Res 176:52–71
Boskovic M, Vovk T, Kores PB, Grabnar I (2011) Oxidative stress in schizophrenia. Curr Neuropharmacol 9:301–312
Prata J, Santos SG, Almeida MI, Coelho R, Barbosa MA (2017) Bridging autism spectrum disorders and schizophrenia through inflammation and biomarkers-pre-clinical and clinical investigations. J Neuroinflamm 14:179
Anauate MC, Torres LM, de Mello SBV (2010) Effect of isolated fractions of Harpagophytum procumbens DC (devil’s claw) on COX1, COX2 activity and nitric oxide production on whole blood assay. Phytother Res 24:1365–1369
Korkina LG (2007) Phenylpropanoids as naturally occurring antioxidants: from plant defense to human health. Cell Mol Biol 53:15–25
Schaffer LF, Peroza LR, Boligon AA, Athayde ML, Alves SH, Fachinetto R, Wagner C (2013) Harpagophytum procumbens prevents oxidative stress and loss of cell viability in vitro. Neurochem Res 38:2256–2267
Locatelli M, Ferrante C, Carradori S, Secci D, Leporini L, Chiavaroli A, Leone S, Recinella L, Orlando G, Martinotti S, Brunetti L, Vacca M, Menghini L (2017) Optimization of aqueous extraction and biological activity of Harpagophytum procumbens root on ex vivo rat colon inflammatory model. Phytother Res 31:937–944
Laghari AH, Memon S, Nelofar A, Khan KM, Yasmin A (2011) Determination of free phenolic acids and antioxidant activity of methanolic extracts obtained from fruits and leaves of Chenopodium album. Food Chem 126:1850–1855
Costa F, Dornelles E, Cattani MFM, Algarve TD, De Souza Filho OC, Sagrillo MR, Garcia LFM, Da Cruz IBM (2012) Influence of Val16Ala SOD2 polymorphism on the in-vitro effect of clomiphene citrate in oxidative metabolism. Reprod Biomed Online 24:474–481
William-Faltaos S, Rouillard D, Lechat P, Bastian G (2006) Cell cycle arrest and apoptosis induced by oxaliplatin (L-OHP) on four human cancer cell lines. Anticancer Res 26:2093–2100
Datson N, Speksnijder N, Jong IEM, Steenbergen P, Christensen KV, Potempa K, Pedersen JT, Egebjerg J, Kallunki P, Nielsen EB, Kloet ER, Didriksen M (2011) Hippocampal CA1 region shows differential regulation of gene expression in mice displaying extremes in behavioral sensitization to amphetamine: Relevance for psychosis susceptibility? Psychopharmacology 217:525–538
Figueira FH, Leal CQ, Reis EM, Röpke J, Wagner C, da Rocha JBT, Fachinetto R (2015) Effects of diphenyl diselenide on behavioral and biochemical changes induced by amphetamine in mice. J Neural Transm 122:201209
Ceretta APC, Schaffer LF, de Freitas CM, Reinheimer JB, Dotto MM, Fachinetto R (2016) Gabapentin prevents behavioral changes on the amphetamineinduced animal model of schizophrenia. Schizophr Res 175(1–3):230–231
Soulimani R, Younos C, Mortier F, Derrieu C (1994) The role of stomachal digestion on the pharmacological activity of plant extracts, using as an example extracts of Harpagophytum procumbens. Can J Physiol Pharmacol 72(12):1532–1536
Busanello A, Peroza LR, Wagner C, Sudati JH, Pereira RP, Prestes AS, Rocha JBT, Fachinetto R, Barbosa NBV (2012) Resveratrol reduces vacuous chewing movements induced by acute treatment with fluphenazine. Pharmacol Biochem Behav 101(2):307–310
Machado MS, Rosa RM, Dantas AS, Reolon GK, Appelt HR, Braga AL, Henriques JAP, Roesler R (2006) An organic selenium compound attenuates apomorphine-induced stereotypy in mice. Neurosci Lett 410(3):198–202
Ellman GL (1959) Tissue sulfhydryl groups. Arch Biochem Biophys 82(1):70–77
Pérez-Severiano F, Pérez-Rodríguez M, Pedraza-Chaverrí J, Maldonado PD, Campos ONM, Sánchez-García A, Santamaría A (2004) S-Allylcysteine, a garlicderived antioxidant, ameliorates quinolinic acid-induced neurotoxicity and oxidative damage in rats. Neurochem Int 45(8):1175–1183
Loew D, Möllerfeld J, Schrödter A, Puttkammer S, Kaszkin M (2001) Investigations on the pharmacokinetic properties of Harpagophytum extracts and their effects on eicosanoid biosynthesis in vitro and ex vivo. Clin Pharmacol Ther 69(5):356–364
Colas C, Garcia P, Popot MA, Bonnaire Y, Bouchonnet S (2008) Optimization of solid-phase extraction for the liquid chromatography—mass spectrometry analysis of harpagoside, 8-para-coumaroyl harpagide, and harpagide in equine plasma and urine. J Chromatogr Sci 46(2):174–183
Mncwangi N, Chen W, Vermaak I, Viljoen AM, Gericke N (2012) Devil’s claw—a review of the ethnobotany, phytochemistry and biological activity of Harpagophytum procumbens. J Ethnopharmacol 143(3):755–771
Shinsmon J, Tan SW, Ooi YY, Ramasamy R, Vidyadaran S (2014) Mesenchymal stem cells exert anti-proliferative effect on lipopolysaccharide-stimulated BV2 microglia by reducing tumour necrosis factor-α levels. J Neuroinflamm 11:149
Abdelouahab N, Heard C (2008) Effect of the major glycosides of Harpagophytum procumbens (Devil’s claw) on epidermal cyclooxygenase-2 (COX-2) in vitro. J Nat Prod 71:746–749
Sun X, Xiong Z, Zhang Y, Meng Y, Xu G, Xia Z, Li L, Zhang R, Ke Z, Xia Z, Hu Y (2012) Harpagoside attenuates MPTP/MPP+ induced dopaminergic neurodegeneration and movement disorder via elevating glial cell line derived neurotrophic factor. J Neurochem 120:1072–1083
Grant L, McBean DE, Fyfe L, Warnock AM (2009) The inhibition of free radical generation by preparations of Harpagophytum procumbens in vitro. Phytother Res 23:104–110
Schaffer LF, de Freitas CM, Ceretta APC, Peroza LR, de Moraes RE, Krum BN, Wagner C (2016) Harpagophytum procumbens ethyl acetate fraction reduces fluphenazine-induced vacuous chewing movements and oxidative stress in rat brain. Neurochem Res 41(5):1170–1184
Ungerer G, Cui J, Ndam T, Bekemeier M, Song H, Li R, Siedhoff HR, Yang B, Appenteng MK, Greenlief CM, Miller DK, Sun GY, Folk WR, Gu Z (2020) Harpagophytum procumbens extract ameliorates allodynia and modulates oxidative and antioxidant stress pathways in a rat model of spinal cord injury. NeuroMol Med 22:278–292
Avato P, Argentieri MP (2019) Quality assessment of commercial spagyric tinctures of Harpagophytum procumbens and their antioxidant properties. Molecules 24:1–15
Park KS (2016) A systematic review on anti-inflammatory activity of harpagoside. J Biochem Mol Biol Res 2:166–169
Fujioka H, Akema T (2010) Lipopolysaccharide acutely inhibits proliferation of neural precursor cells in the dentate gyrus in adult rats. Brain Res 1352:35–42
Biazi BI, D’Epiro GFR, Zanetti TA, Oliveira MT, Ribeiro LR, Mantovani MS (2017) Risk assessment via metabolism and cell growth inhibition in a HepG2/C3A cell line upon treatment with Arpadol and its active component Harpagoside. Phytother Res 31:387–394
Boyda HN, Tse L, Procyshyn RM, Honer WG, Barr AM (2010) Preclinical models of antipsychotic drug-induced metabolic side effects. Trends Pharmacol Sci 31:484–497
Wolgin DL (2012) Amphetamine stereotypy, the basal ganglia, and the “selection problem.” Behav Brain Res 231(2):297–308
Chen C, Zhang H, Xu H, Xue R, Zheng Y, Wu T, Lian Y (2018) Harpagoside rescues the memory impairments in chronic cerebral hypoperfusion rats by inhibiting PTEN activity. J Alzheimers Dis 63(2):445–455
Bramness JG, Gundersen ØH, Guterstam J, Rognli EB, Konstenius M, Løberg EM, Franck J (2012) Amphetamine-induced psychosis-a separate diagnostic entity or primary psychosis triggered in the vulnerable? BMC Psychiatry 12(1):221
Mahomed IM, Ojewole JA (2006) Anticonvulsant activity of Harpagophytum procumbens DC [Pedaliaceae] secondary root aqueous extract in mice. Brain Res Bull 69(1):57–62
El-Sisi AES, Sokkar SS, El-Sayad MES, Ramadan ES, Osman EY (2016) Celecoxib and omega-3 fatty acids alone and in combination with risperidone affect the behavior and brain biochemistry in amphetamine-induced model of schizophrenia. Biomed Pharmacother 82:425–431
Rampino A, Marakhovskaia A, Soares-Silva T, Torretta S, Veneziani F, Beaulieu JM (2019) Antipsychotic drug responsiveness and dopamine receptor signaling; old players and new prospects. Front Psychiatry 9(702):1–13
Karam CS, Javitch JA (2018) Phosphorylation of the amino terminus of the dopamine transporter: regulatory mechanisms and implications for amphetamine action. Adv Pharmacol 82:205–234
Akil M, Pierri JN, Whitehead RE, Edgar CL, Mohila C, Sampson AR, Lewis DA (1999) Lamina-specific alterations in the dopamine innervation of the prefrontal cortex in schizophrenic subjects. Am J Psychiatry 156(10):1580–1589
Abi-Dargham A, van de Giessen E, Slifstein M, Kegeles LS, Laruelle M (2009) Baseline and amphetamine-stimulated dopamine activity are related in drug-naive schizophrenic subjects. Biol Psychiatry 65(12):1091–1093
Berman SB, Hastings TG (1999) Dopamine oxidation alters mitochondrial respiration and induces permeability transition in brain mitochondria: implications for Parkinson’s disease. J Neurochem 73(3):1127–1137
Meyer U, Schwarz MJ, Müller N (2011) Inflammatory processes in schizophrenia: a promising neuroimmunological target for the treatment of negative/cognitive symptoms and beyond. Pharmacol Ther 132(1):96–110
Thomas DM, Kuhn DM (2005) Cyclooxygenase-2 is an obligatory factor in methamphetamine-induced neurotoxicity. J Pharmacol Exp Ther 313(2):870–876
Kaszkin M, Beck KF, Koch E, Erdelmeier C, Kusch S, Pfeilschifter J, Loew D (2004) Downregulation of iNOS expression in rat mesangial cells by special extracts of Harpagophytum procumbens derives from harpagoside-dependent and independent effects. Phytomedicine 11(7–8):585–595
Funding
Funding was provided by Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (Grant No. 001).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing Interests
The authors have not disclosed any competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lima, V.B., Viana, A.R., Santos, D. et al. Ethyl Acetate Fraction of Harpagophytum procumbens Prevents Oxidative Stress In Vitro and Amphetamine-Induced Alterations in Mice Behavior. Neurochem Res 48, 1716–1727 (2023). https://doi.org/10.1007/s11064-022-03846-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11064-022-03846-z