Abstract
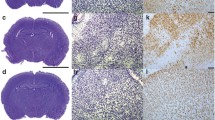
Preterm birth and hypoxia–ischemia (HI) are major causes of neonatal death and neurological disabilities in newborns. The widely used preclinical HI model combines carotid occlusion with hypoxia exposure; however, the relationship between different hypoxia exposure periods with brain tissue loss, astrocyte reactivity and behavioral impairments following HI is lacking. Present study evaluated HI-induced behavioral and morphological consequences in rats exposed to different periods of hypoxia at postnatal day 3. Wistar rats of both sexes were assigned into four groups: control group, HI-120 min, HI-180 min and HI-210 min. Neurodevelopmental reflexes, exploratory abilities and cognitive function were assessed. At adulthood, tissue damage and reactive astrogliosis were measured. Animals exposed to HI-180 and HI-210 min had delayed neurodevelopmental reflexes compared to control group. Histological assessment showed tissue loss that was restricted to the ipsilateral hemisphere in lower periods of hypoxia exposure (120 and 180 min) but affected both hemispheres when 210 min was used. Reactive astrogliosis was increased only after 210 min of hypoxia. Interestingly, cognitive deficits were induced regardless the duration of hypoxia and there were correlations between behavioral parameters and cortex, hippocampus and corpus callosum volumes. These results show the duration of hypoxia has a close relationship with astrocytic response and tissue damage progression. Furthermore, the long-lasting cognitive memory deficit and its association with brain structures beyond the hippocampus suggests that complex anatomical changes should be involved in functional alterations taking place as hypoxia duration is increased, even when the cognitive impairment limit is achieved.





Similar content being viewed by others
References
Blencowe H, Cousens S, Chou D et al (2013) Born too soon: the global epidemiology of 15 million preterm births. Reprod Health 10:1–14. https://doi.org/10.1186/1742-4755-10-S1-S2
Liu L, Johnson HL, Cousens S et al (2012) Global, regional, and national causes of child mortality: an updated systematic analysis for 2010 with time trends since 2000. Lancet 379:2151–2161. https://doi.org/10.1016/S0140-6736(12)60560-1
Volpe JJ (2009) Brain injury in premature infants: a complex amalgam of destructive and developmental disturbances. Lancet Neurol 8:110–124. https://doi.org/10.1016/S1474-4422(08)70294-1
Xiong F, Zhang L (2013) Role of the hypothalamic-pituitary-adrenal axis in developmental programming of health and disease. Front Neuroendocrinol 34:27–46
Clowry GJ, Basuodan R, Chan F (2014) What are the best animal models for testing early intervention in Cerebral Palsy? Front Neurol 5:1–17. https://doi.org/10.3389/fneur.2014.00258
Jantzie LL, Corbett CJ, Berglass J et al (2014) Complex pattern of interaction between in utero hypoxia-ischemia and intra-amniotic inflammation disrupts brain development and motor function. J Neuroinflammation 11:131. https://doi.org/10.1186/1742-2094-11-131
Teune MJ, Bakhuizen S, Bannerman CG et al (2011) A systematic review of severe morbidity in infants born late preterm. Am J Obstet Gynecol 205:374.e1–374.e9. https://doi.org/10.1016/j.ajog.2011.07.015
Zhu LH, Bai X, Zhang N et al (2014) Improvement of human umbilical cord mesenchymal stem cell transplantation on glial cell and behavioral function in a neonatal model of periventricular white matter damage. Brain Res 1563:13–21. https://doi.org/10.1016/j.brainres.2014.03.030
Stadlin A, James A, Fiscus R et al (2003) Development of a postnatal 3-day-old rat model of mild hypoxic-ischemic brain injury. Brain Res 993:101–110. https://doi.org/10.1016/j.brainres.2003.08.058
Sizonenko SV, Sirimanne E, Mayall Y et al (2003) Selective cortical alteration after hypoxic-ischemic injury in the very immature rat brain. Pediatr Res 54:263–269. https://doi.org/10.1203/01.PDR.0000072517.01207.87
Tang G, Gudsnuk K, Kuo SH et al (2014) Loss of mTOR-dependent macroautophagy causes autistic-like synaptic pruning deficits. Neuron 83:1131–1143. https://doi.org/10.1016/j.neuron.2014.07.040
Rice JE, Vannucci RC, Brierley JB (1981) The influence of immaturity on hypoxic-ischemic brain damage in the rat. Ann Neurol 9(2):131–141
Patel SD, Pierce L, Ciardiello A et al (2015) Therapeutic hypothermia and hypoxia-ischemia in the term-equivalent neonatal rat: characterization of a translational preclinical model. Pediatr Res 78:264–271. https://doi.org/10.1038/pr.2015.100
Patel SD, Pierce L, Ciardiello AJ, Vannucci SJ (2014) Neonatal encephalopathy: pre-clinical studies in neuroprotection. Biochem Soc Trans 42:564–568. https://doi.org/10.1042/BST20130247
Arteni NS, Salgueiro J, Torres I et al (2003) Neonatal cerebral hypoxia-ischemia causes lateralized memory impairments in the adult rat. Brain Res 973:171–178. https://doi.org/10.1016/S0006-8993(03)02436-3
Pereira LO, Nabinger PM, Strapasson ACP et al (2009) Long-term effects of environmental stimulation following hypoxia-ischemia on the oxidative state and BDNF levels in rat hippocampus and frontal cortex. Brain Res 1247:188–195. https://doi.org/10.1016/j.brainres.2008.10.017
Wang LS, Zhou J, Shao XM, Tang XC (2002) Huperzine A attenuates cognitive deficits and brain injury in neonatal rats after hypoxia-ischemia. Brain Res 949:162–170. https://doi.org/10.1016/S0006-8993(02)02977-3
Semple BD, Blomgren K, Gimlin K et al (2013) Brain development in rodents and humans: identifying benchmarks of maturation and vulnerability to injury across species. Prog Neurobiol 106–107:1–16. https://doi.org/10.1016/j.pneurobio.2013.04.001
Alexander M, Garbus H, Smith AL et al (2014) Behavioral and histological outcomes following neonatal HI injury in a preterm (P3) and term (P7) rodent model. Behav Brain Res 259:85–96. https://doi.org/10.1016/j.bbr.2013.10.038
Sanches EF, Arteni N, Nicola F et al (2015) Sexual dimorphism and brain lateralization impact behavioral and histological outcomes following hypoxia–ischemia in P3 and P7 rats. Neuroscience 290:581–593. https://doi.org/10.1016/j.neuroscience.2014.12.074
McCullough N, Parkes J, Kerr C, McDowell BC (2011) The health of children and young people with cerebral palsy: a longitudinal, population-based study. Int J Nurs Stud 50:747–756. https://doi.org/10.1016/j.ijnurstu.2011.01.011
Volpe JJ (2009) The encephalopathy of prematurity-brain injury and impaired brain development inextricably intertwined. Semin Pediatr Neurol 16:167–178. https://doi.org/10.1016/j.spen.2009.09.005
Durán-Carabali L, Sanches E, Marques M et al (2017) Longer hypoxia–ischemia periods to neonatal rats causes motor impairments and muscular changes. Neuroscience 340:291–298. https://doi.org/10.1016/j.neuroscience.2016.10.068
Towfighi J, Mauger D, Vannucci RC, Vannucci SJ (1997) Influence of age on the cerebral lesions in an immature rat model of cerebral hypoxia-ischemia: a light microscopic study. Brain Res Dev Brain Res 100:149–160
Burda JE, Sofroniew MV (2014) Reactive gliosis and the multicellular response to CNS damage and disease. Neuron 81:229–248. https://doi.org/10.1016/j.neuron.2013.12.034
Odorcyk FK, Nicola F, Duran-Carabali LE et al (2017) Galantamine administration reduces reactive astrogliosis and upregulates the anti-oxidant enzyme catalase in rats submitted to neonatal hypoxia ischemia. Int J Dev Neurosci 62:15–24. https://doi.org/10.1016/j.ijdevneu.2017.07.006
Ling E-A, Leblond CP (1973) Investigation of glial cells in semithin sections. II. Variation with age in the numbers of the various glial cell types in rat cortex and corpus callosum. J Comp Neurol 149:73–81. https://doi.org/10.1002/cne.901490105
Epelman M, Daneman A, Halliday W et al (2012) Abnormal corpus callosum in neonates after hypoxic-ischemic injury. Pediatr Radiol 42:321–330. https://doi.org/10.1007/s00247-011-2238-5
Sanches EF, Durán-Carabali LE, Tosta A et al (2017) Pregnancy swimming causes short- and long-term neuroprotection against hypoxia-ischemia in very immature rats. Pediatr Res 82:544–553. https://doi.org/10.1038/pr.2017.110
Moses P, Courchesne E, Stiles J et al (2000) Regional size reduction in the human corpus callosum following pre- and perinatal brain injury. Cereb Cortex 10:1200–1210. https://doi.org/10.1093/cercor/10.12.1200
Lubics A, Reglodi D, Tamás A et al (2005) Neurological reflexes and early motor behavior in rats subjected to neonatal hypoxic-ischemic injury. Behav Brain Res 157:157–165. https://doi.org/10.1016/j.bbr.2004.06.019
Cárdenas L, García-García F, Santiago-Roque I et al (2015) Enriched environment restricted to gestation accelerates the development of sensory and motor circuits in the rat pup. Int J Dev Neurosci 41:68–73. https://doi.org/10.1016/j.ijdevneu.2014.11.008
Fox WM (1965) Reflex-ontogeny and behavioural development of the mouse. Anim Behav 13:234–241. https://doi.org/10.1016/0003-3472(65)90041-2
Sanches EF, Arteni NS, Spindler C et al (2012) Effects of pre- and postnatal protein malnutrition in hypoxic-ischemic rats. Brain Res 1438:85–92. https://doi.org/10.1016/j.brainres.2011.12.024
Favero AM, Weis SN, Zeni G et al (2006) Diphenyl diselenide changes behavior in female pups. Neurotoxicol Teratol 28:607–616. https://doi.org/10.1016/j.ntt.2006.08.003
Arteni NS, Pereira LO, Rodrigues AL et al (2010) Lateralized and sex-dependent behavioral and morphological effects of unilateral neonatal cerebral hypoxia-ischemia in the rat. Behav Brain Res 210:92–98. https://doi.org/10.1016/j.bbr.2010.02.015
Paxinos G, Watson C (1998) The rat brain—in stereotaxic coordinates, Fourth
Furukawa S, Sameshima H, Yang L, Ikenoue T (2011) Acetylcholine receptor agonist reduces brain damage induced by hypoxia-ischemia in newborn rats. Reprod Sci 18:172–179. https://doi.org/10.1177/1933719110385129
Ota A, Ikeda T, Ikenoue T, Toshimori K (1997) Sequence of neuronal responses assessed by immunohistochemistry in the newborn rat brain after hypoxia-ischemia. Am J Obstet Gynecol 177:519–526. https://doi.org/10.1016/S0002-9378(97)70139-X
Mestriner RG, Saur L, Bagatini PB et al (2015) Astrocyte morphology after ischemic and hemorrhagic experimental stroke has no influence on the different recovery patterns. Behav Brain Res 278:257–261. https://doi.org/10.1016/j.bbr.2014.10.005
Tai W, Burke KA, Dominguez JF et al (2009) Growth deficits in a postnatal day 3 rat model of hypoxic-ischemic brain injury. Behav Brain Res 202:40–49. https://doi.org/10.1016/j.bbr.2009.03.043
Mayoral SR, Omar G, Penn AA (2009) Sex differences in a hypoxia model of preterm brain damage. Pediatr Res 66:248–253. https://doi.org/10.1203/PDR.0b013e3181b1bc34
Ment LR, Schwartz M, Makuch RW, Stewart WB (1998) Association of chronic sublethal hypoxia with ventriculomegaly in the developing rat brain. Dev Brain Res. https://doi.org/10.1016/S0165-3806(98)00139-4
Horvath G, Reglődi Dora, Farkas J et al (2015) Perinatal positive and negative influences on the early neurobehavioral reflex and motor development. In: Antonelli Marta C (ed) Perinatal programming of neurodevelopment. Springer, New York, pp 149–167
Ashwal S, Ghosh N, Turenius CI et al (2014) The reparative effects of neural stem cells in neonatal hypoxic-schemic injury are not influenced by host gender. Pediatr Res 75:603–611. https://doi.org/10.1038/pr.2014.7.The
Huang Z, Song L, Wang C et al (2012) Hypoxia-ischemia upregulates TRAIL and TRAIL receptors in the immature rat brain. Dev Neurosci 33:519–530. https://doi.org/10.1159/000334475
Rice JE, Vannucci RC, Brierley JB (1981) The influence of immaturity on hypoxic-ischemic brain damage in the rat. Ann Neurol 9:131–141. https://doi.org/10.1002/ana.410090206
Schuch CP, Diaz R, Deckmann I et al (2016) Early environmental enrichment affects neurobehavioral development and prevents brain damage in rats submitted to neonatal hypoxia-ischemia. Neurosci Lett 617:101–107. https://doi.org/10.1016/j.neulet.2016.02.015
Söderström I, Strand M, Ingridsson AC et al (2009) 17Β-Estradiol and enriched environment accelerate cognitive recovery after focal brain ischemia. Eur J Neurosci 29:1215–1224. https://doi.org/10.1111/j.1460-9568.2009.06662.x
Sanches E, Arteni N, Scherer E et al (2013) Are the consequences of neonatal hypoxia-ischemia dependent on animals’ sex and brain lateralization? Brain Res 1507:105–114. https://doi.org/10.1016/j.brainres.2013.02.040
Nunn JA, LePeillet E, Netto CA et al (1994) Global ischaemia: hippocampal pathology and spatial deficits in the water maze. Behav Brain Res 62:41–54. https://doi.org/10.1016/0166-4328(94)90036-1
Bothe HW, Bosma HJ, Hofer H et al (1986) Selective vulnerability of hippocampus and disturbances of memory storage after mild unilateral ischemia of gerbil brain. Stroke 17:1160–1163. https://doi.org/10.1161/01.STR.17.6.1160
Zanelli AS, Rajasekaran KK, Grosenbaugh KD, Kapur J (2015) Increased excitability and excitatory synaptic transmission during in vitro ischemia in the neonatal mouse hippocampus. Neuroscience 3:279–289. https://doi.org/10.1016/j.neuroscience.2015.09.046
McLean C, Ferriero D (2004) Mechanisms of hypoxic-ischemic injury in the term infant. Semin Perinatol 28:425–432. https://doi.org/10.1053/j.semperi.2004.10.005
Zhu C, Wang X, Xu F et al (2005) The influence of age on apoptotic and other mechanisms of cell death after cerebral hypoxia-ischemia. Cell Death Differ 12:162–176. https://doi.org/10.1038/sj.cdd.4401545
Ferriero DM (2001) Oxidant mechanisms in neonatal hypoxia-ischemia. Dev Neurosci 23:198–202. https://doi.org/10.1159/000046143
Volpe JJ (2001) Neurobiology of periventricular leukomalacia in the premature infant. Pediatr Res 50:553–562. https://doi.org/10.1203/00006450-200111000-00003
Rocha-Ferreira E, Hristova M, Rocha-Ferreira E, Hristova M (2016) Plasticity in the neonatal brain following hypoxic-ischaemic injury. Neural Plast 2016:1–16. https://doi.org/10.1155/2016/4901014
Johnston MV (2009) Plasticity in the developing brain: implications for rehabilitation. Dev Disabil Res Rev 15:94–101. https://doi.org/10.1002/ddrr.64
Freeman MR (2010) Specification and morphogenesis of astrocytes. Science 330:774–778. https://doi.org/10.1126/science.1190928
Gobius I, Morcom L, Suárez R et al (2016) Astroglial-mediated remodeling of the interhemispheric midline is required for the formation of the corpus callosum Ilan. Cell Rep 17:735–747. https://doi.org/10.1016/j.celrep.2016.09.033.Astroglial-mediated
Mallard C, Davidson JO, Tan S et al (2013) Astrocytes and microglia in acute cerebral injury underlying cerebral palsy associated with preterm birth. Pediatr Res 75:1–7. https://doi.org/10.1038/pr.2013.188
Sofroniew MV (2009) Molecular dissection of reactive astrogliosis and glial scar formation. Trends Neurosci 32:638–647. https://doi.org/10.1016/j.tins.2009.08.002
Mestriner RG, Pagnussat S, Boisserand LSB et al (2011) Skilled reaching training promotes astroglial changes and facilitated sensorimotor recovery after collagenase-induced intracerebral hemorrhage. Exp Neurol 227:53–61. https://doi.org/10.1016/j.expneurol.2010.09.009
Po C, Kalthoff D, Kim YB et al (2012) White matter reorganization and functional response after focal cerebral ischemia in the rat. PLoS ONE. https://doi.org/10.1371/journal.pone.0045629
Segovia KN, Mcclure M, Moravec M et al (2008) Arrested oligodendrocyte lineage maturation in chronic perinatal white matter injury. Ann Neurol 63:520–530. https://doi.org/10.1002/ana.21359.ARRESTED
Theodosis D, Poulain D, Oliet S (2008) Activity-dependent structural and functional plasticity of astrocyte-neuron interactions. Physiol Rev. https://doi.org/10.1152/physrev.00036.2007
Acknowledgements
The authors thank the staff of Reproduction and Laboratory Animal Research Center from Biochemistry Department UFRGS.
Funding
Present work was supported by Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq) and Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Durán-Carabali, L.E., Sanches, E.F., Odorcyk, F.K. et al. Tissue Injury and Astrocytic Reaction, But Not Cognitive Deficits, Are Dependent on Hypoxia Duration in Very Immature Rats Undergoing Neonatal Hypoxia–Ischemia. Neurochem Res 44, 2631–2642 (2019). https://doi.org/10.1007/s11064-019-02884-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11064-019-02884-4