Abstract
Malignant and benign brain tumors with a propensity to recur continue to be a clinical challenge despite decades-long efforts to develop systemic and more advanced local therapies. GammaTile (GT Medical Technologies Inc., Tempe AZ) has emerged as a novel brain brachytherapy device placed during surgery, which starts adjuvant radiotherapy immediately after resection. GammaTile received FDA clearance in 2018 for any recurrent brain tumor and expanded clearance in 2020 to include upfront use in any malignant brain tumor. More than 1,000 patients have been treated with GammaTile to date, and several publications have described technical aspects of the device, workflow, and clinical outcome data. Herein, we review the technical aspects of this brachytherapy treatment, including practical physics principles, discuss the available literature with an emphasis on clinical outcome data in the setting of brain metastases, glioblastoma, and meningioma, and provide an overview of the open and pending clinical trials that are further defining the efficacy and safety of GammaTile.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Brain tumors that tend to recur, such as high-grade glioma, brain metastases, and some meningiomas, inflict a great degree of morbidity and mortality. Adjuvant radiation therapy after resection of these tumors is standard of care, aimed at providing local control (LC). Despite technological advances made in external beam radiation therapy (EBRT), such as stereotactic radiotherapy (SRT), intensity modulated radiation therapy (IMRT), and protons, LC remains a challenge in the postoperative setting for brain metastases [1,2,3], glioblastoma (GBM) [4], and recurrent meningioma [5].
Suboptimal outcomes may continue for several reasons. The time needed for wound healing between resection and EBRT initiation allows opportunity for proliferation of residual tumor cells, which can result in rapid early progression (REP) as seen in GBM [6], and rapid recurrence (RR) of brain metastasis before initiation of adjuvant EBRT [7, 8]. Precisely defining the target volume for a postoperative tumor cavity can be challenging when using EBRT, particularly for brain metastases [9,10,11]. Additionally, providing LC after recurrence of a previously irradiated tumor is especially challenging since brain immediately adjacent to the local recurrence would typically have already received EBRT to near tolerance doses [12,13,14], making it difficult to provide efficacious doses of radiation with repeat EBRT for tumors that have shown themselves to be resistant to EBRT.
Implanting internal radioactive sources within the tumor cavity immediately after resection, a radiation modality referred to as brachytherapy (BT), may address multiple intrinsic challenges of EBRT and thus expand available options for effective postoperative adjuvant therapy [15,16,17]. Dose from low-energy radioactive sources implanted within the surgical cavity is characterized by a steep fall off in tissue surrounding the target volume, which results in dosimetric sparing of scalp or distal normal brain parenchyma compared to EBRT [15, 16, 18]. Among brain BT techniques, GammaTile® (GT Medical Technologies Inc., Tempe AZ) was specifically developed to improve the dosimetric, technical, and workflow aspects of existing techniques [19, 20] and is the only commercially available collagen tile BT.
Below, we review the technical aspects of GammaTile therapy and then discuss published clinical outcome data for brain metastases, GBM, and meningioma. We discuss how GammaTile use may help circumvent two management barriers that can affect outcomes: (1) time delays to EBRT (and the phenomenon REP/RR) and (2) the difficulty of treating recurrent, previously irradiated tumors. We also discuss the four ongoing and one upcoming clinical trials (Table 1) evaluating the safety and efficacy of GammaTile across various clinical scenarios.
Technical factors
GammaTiles are bioresorbable, conformable, 20 × 20 × 4 mm collagen squares containing four radioactive titanium-encapsulated cesium-131 (Cs-131) seeds per tile (Fig. 1). Upon completion of resection, the neurosurgeon lines the tumor cavity with sufficient tiles to cover the surfaces at risk for recurrence. This permanently implanted device functions as both a seed carrier and three-dimensional spacer, offsetting seeds 3 mm from the tumor cavity surface and 10 mm from each other (Fig. 2). The 10 mm fixed inter-seed spacing aims to prevent dosimetric “hot spots” and “cold spots” that could arise from irregular spacing of seeds and can occur with more traditional brain BT methods, such as stranded seeds [19]. The 3 mm offset between seeds and the tile surface prevents the very high doses of radiation that would occur if seeds were placed directly on brain.
The radioactive Cs-131 seeds used in GammaTiles are manufactured to have a fixed source strength of 3.5 U (cGy cm2 h−1) on day of implant. The GammaTile design and source strength results in a physical dose of approximately 60 Gy to a depth of 5 mm in brain (Fig. 3); however, cavity shape, cavity size, and number of tiles can affect specific implant dose distributions. Compared to more traditional brain BT using seeds with a range of source strengths and heterogeneity of prescription doses [21, 22], standardization of source strength at implant reduces dosimetric variability across patients and may simplify studying outcomes.
GammaTile dosimetry. A Preoperative T1 post contrast MRI showing a single brain metastasis. B Postoperative MRI fused with postoperative CT scan demonstrating GammaTile dosimetry (doses in centigray) [8]
Cs-131 has a half-life of 9.7 days, compared to 59.4 days for iodine-125, which has also been used in brain BT. The relatively short half-life of Cs-131 ensures the planned dose is given in a shorter period at a higher initial dose rate, which may better address highly proliferative malignant brain tumors [23]. The short half-life also helps ensure the planned dose is delivered before collagen tile reabsorption and seed displacement [24,25,26,27].
Preoperative, intraoperative, and postoperative workflow
GammaTile therapy requires a multidisciplinary care team approach [28]. Neurosurgery, neuro-oncology, and radiation oncology teams collaborate on patient selection and accurate case planning. Based on a preoperative MRI, the surface area of the expected postoperative tumor cavity deemed at risk for recurrence is estimated, considering portions of the cavity that may not need tiles (e.g., surgical tract) and potential intraoperative cavity contraction. After tumor resection, the tiles are placed on the tumor bed with the 3 mm offset from the seed facing brain parenchyma to achieve the desired seed-to-brain offset.
The collagen component of the GammaTile is the same material neurosurgeons have used to reconstruct dura for decades, and the ease of usability is demonstrated with an average implantation time of 2–5 min [24]. The fast implant time helps minimize radiation exposure to perioperative staff and limits the time patients spend under anesthesia. In a study of 22 patients treated with GammaTile (including two patients who had multiple GammaTile treatments for separate tumors), measured and modeled radiation exposure for healthcare workers and caregivers was below regulatory limits for medical personnel and the public [29].
Following surgical closure, a postoperative radiation survey measurement is performed to quantify the maximum radiation exposure one meter from the implant site to verify the patient meets regulatory limits for patient release. Using U.S. Nuclear Regulatory Commission recommendations, patients may be released based on 1-meter measurements of ≤ 6 mrem/hr [30]. In a single institution study, the reported mean survey measurement was 1.83 mrem/hr with a range of 0.5–3.5 mrem/hr for 13 patients [31]. In addition to the standard postoperative MRI exam assessing extent of resection, a thin-cut non-contrast brain CT is obtained, typically 12–72 h postimplant. Like other forms of permanent seed BT, the CT is used to document the position and number of implanted sources as well as the isodose lines/radiation field (Fig. 4) [32]. Importantly, the outcome data (LC, toxicity) described below results from surgically targeting the oncologic at-risk tissue with GammaTiles rather than trying to meet pre-specified dosimetry parameters. To date, no specific postimplant dosimetric parameters have been correlated with probability of LC or toxicity in the case of recurrent GBM [33] or brain metastases [8]. Predictive postimplant dosimetric parameters may become apparent as trial data matures (Table 1).
Brain metastases
Brain metastases are the most common malignant brain tumors in adults, and they pose a burden for patients with cancer both at initial diagnosis and re-occurrence. The use of SRT for intact, typically smaller, non-resected brain metastases confers LC on the order of ~ 85% [34]. Durable LC in the postoperative setting for larger brain metastases requiring resection has been more challenging, with LC at 60–79% [1,2,3]. Whole brain radiotherapy is another option, but comes at the cost of neurocognitive toxicity and still results in a local failure rate of ~ 14% when used in the postoperative setting [1].
Intraoperative treatment with GammaTile implantation may mitigate factors that lead to worse LC after resection. Changes in the resection cavity between SRT planning, MRI, and SRT delivery could lead to a marginal miss, especially due to the highly conformal nature of SRT [7, 9]. Also, time delay from surgery to SRT initiation (which can result from a skilled nursing stay, coordination with systemic therapies, and logistics for setting up radiation oncology consultation, CT simulation, and radiation delivery [35]) leads to worse LC, with a local failure rate of 2.3% if SRT starts before 4 weeks, 14.5% between 4 and 8 weeks, and 48.5% if started after 8 weeks postoperation [35]. Some patients are lost to follow up and never receive SRT, with one prospective trial of post-operative SRS demonstrating 22% of patients never received the planned SRT course [36]. Furthermore, a subset of aggressive brain metastases can rapidly recur after complete resection but before postoperative SRT, even if SRT is delivered before 4 weeks [8]. Compared to postoperative SRT, GammaTiles are implanted at resection, guaranteeing adjuvant radiation starts immediately.
Recurrent brain metastases
Local recurrence of a brain metastasis previously treated with radiation is a particularly challenging clinical situation. Some management options for recurrent previously irradiated brain metastases include SRT, surgery alone, and surgery followed by postoperative SRT. The 1-year estimated LC rate after repeat SRT is 61–68% [37, 38]. The frequency of adverse radiation effect in the repeat SRT (non-surgical) setting from a large series at UCSF was 37% [39], and the frequency of symptomatic radiation necrosis (RN) is 20–24% [39, 40].
Surgical resection can be done for recurrent previously irradiated brain metastases, especially when there is mass effect, but surgery without adjuvant radiation leads to a local failure rate of 40–44% [34, 41]. Postoperative SRT after resecting a previously irradiated brain metastasis leads to LC of 70–75% with an RN rate of 13% [41, 42]. Lowering the radiation dose, which can mitigate RN, may compromise LC [43], especially for radioresistant tumors (recurring after radiation).
In the initial multi-histology prospective basket trial at Barrow Neurological Institute evaluating GammaTile, 96 patients with 108 tumor cavities received resection and GammaTile. Within this cohort, 12 patients with recurrent brain metastases were enrolled. The estimated 1-year LC of recurrent previously irradiated brain metastases treated with GammaTile was 80%. The single patient that experienced local failure had a 3.2 cm sarcoma metastasis. Two patients (16.7%) experienced radiation injury that resolved with dexamethasone [20].
GammaTile outcomes in the recurrent setting have been largely reproduced on a prospective registry at Memorial Sloan Kettering Cancer Center [44], where 20 patients received GammaTile to a total of 25 brain metastases that were previously irradiated and had recurred (median recurrence was 3 cm). The 1-year local failure incidence after resection and GammaTile was 8%, and symptomatic necrosis was 16%, which was managed with dexamethasone. This registry trial prompted investigators at Memorial Sloan Kettering Cancer Center to initiate a randomized Phase 2 trial (NCT04690348) comparing resection with GammaTile to resection without GammaTile (Table 1).
Most recently, Miami Cancer Institute reported on their experience using resection and GammaTile for recurrent previously irradiated brain metastases. They compared LC after salvage surgery plus GammaTile to LC after the first course of EBRT. The 6-, 12-, and 18-month LC rates were 66.7%, 33.3%, and 25% after the previous EBRT, and in comparison, these rates were 100%, 100%, and 100% after surgery plus GammaTile (p < 0.001). At a median follow up of 14.5 months, there was one instance (8%) of RN (Grade 2) [45].
Newly diagnosed brain metastases
As a pilot study, The University of Minnesota evaluated GammaTile for newly diagnosed brain metastases. They identified 10 consecutive patients with rapidly growing brain metastases, which they defined as either (1) brain metastases that developed symptomatic postoperative recurrence before radiation could be given (within 4 weeks of surgery) and required another resection or (2) patients who had brain metastases enlarged by > 25% volume before surgery and were considered at risk of RR between surgery and SRT. Once identified, these patients all underwent surgery (resection or re-resection) plus GammaTile. At a median follow-up of 186 days, no patients experienced local recurrence and there were no incidences of RN [8].
The use of GammaTile for newly diagnosed brain metastasis requiring resection is being evaluated by the Phase 3 trial ROADS trial (NCT04365374) (Table 1). In this trial, patients with tumors measuring 2–5 cm in diameter are randomized between surgery plus postoperative SRT versus surgery plus GammaTile. Primary outcome is LC with secondary outcomes including overall survival (OS) and rates of leptomeningeal disease (which can occur in up to 30% of cases after SRT) [46].
Glioblastoma
GBM is the most common malignant primary brain tumor in adults. Most re-occur within 2 cm of the resection cavity [4, 24, 47,48,49]. Despite great efforts over the last ~ 20 years to improve the standard of care for the treatment of newly diagnosed GBM, median OS from diagnosis continues to be poor, around 16–20 months [50].
At recurrence, there is no established standard of care, and available options include surgical resection, re-irradiation, systemic therapies and/or immunotherapies, alone or in combination [12,13,14, 50,51,52]. None of the available treatment strategies have shown significant OS via randomized trials.
Recurrent glioblastoma
As part of the multi-histology prospective basket trial at Barrow, 28 patients with recurrent GBM received maximum safe resection with GammaTile (20 patients at first recurrence, 8 patients at second or third recurrence). Median time to local failure was 12.1 months and median OS from diagnosis was 25 months [17]. There was a 7% rate of symptomatic RN among these patients managed with dexamethasone.
Another prospective cohort of patients at the University of Minnesota was treated with maximum safe resection and GammaTile for IDH wild-type GBM recurrence. 6- and 12-month LC was 86 and 81% respectively, and median OS from diagnosis was 25 months. Although RN was suspected in 4 patients (18%), upon subsequent craniotomy, pathology demonstrated recurrence. The authors also reported a contemporaneous cohort of patients treated with surgery but without GammaTile. Comparing the two cohorts, patients who received GammaTile with resection had a longer progression-free survival (PFS) (p = 0.05) and OS (p = 0.006) [33] compared to the non-GammaTile cohort. To date, the most used indication for GammaTile has been recurrent GBM [53].
The PATHWAYS trial (NCT05900908) will evaluate GammaTile for first recurrence of GBM by randomizing patients with IDH wild-type recurrent GBM to either surgery alone or surgery plus GammaTile (Table 1). Patients on both arms will then receive systemic therapy, either bevacizumab or lomustine, (decided by the treatment team). This trial is scheduled to open in the fall of 2023 with a target accrual of 267 patients and with a primary outcome of OS.
For patients with recurrent GBM, quality of life is a top priority, and by providing radiation at time of resection, BT can spare patients the time needed for daily treatments of EBRT. Quality of life is also an outcome measure on the registry and PATHWAYS trials (Table 1).
Newly diagnosed glioblastoma
Standard of care for newly diagnosed GBM is maximum safe resection followed by chemoradiation (for patients with good performance status, treatment is 60 Gy in 30 fractions plus temozolomide) along with tumor treating fields [50]. Recently, a multi-institutional meta-analysis studied the frequency of GBM REP (the recurrence of any amount or growth of tumor) between maximum safe resection and start of EBRT. The incidence of REP was 46%, and importantly, REP was associated with worse PFS and OS [6]. Additionally, some recent reports suggest that delays between surgery and radiation may impact GBM outcomes [54, 55]. These findings suggest that starting radiation immediately at time of maximum safe resection could reduce the incidence of REP, preclude time delay to EBRT, and potentially improve outcomes.
The GESTALT trial (NCT05342883) (Table 1) is testing the safety and feasibility of combining GammaTile with EBRT and concurrent temozolomide as a way of “bridging” the patient from the time of surgery to the start of EBRT using BT to forestall progression. This study utilizes a novel voxel by voxel optimization algorithm such that the high risk and lower risk CTVs will get the biologically equivalent doses of 60 Gy in 30 fractions and 46 Gy 23 fractions [56].
Meningioma
Meningiomas are the most common benign brain tumors in adults, but recurrence can lead to significant neurologic morbidity and be challenging to manage [19]. Recurrent meningiomas after previous radiation are especially challenging given the large and irregular radiation fields often required for treatment. Since patients can live many years after a recurrence, late toxicity from re-irradiation is an important consideration when deciding salvage treatment strategy. RN risk is often mitigated by administering repeat radiation at a reduced, possibly less effective, dose [19, 57].
On the multi-histology Barrow trial, 20 patients with recurrent previously irradiated meningiomas (20% Grade 1, 70% Grade 2, 10% Grade 3) were treated with resection and GammaTile. PFS at 18 months after salvage surgery plus GammaTile was 89%, compared to 50% PFS at 18 months following the previously attempted therapy). The rate of symptomatic RN was 10% [19].
Harms
The RN rates associated with BT in the re-irradiation setting are listed above by histology, but it is also important to consider other potential adverse effects. These have been tracked on the multicenter STaRT multi-histology registry (NCT04427384) initiated in June 2020, which has enrolled over 250 patients among 33 centers (Table 1). Thus far, GammaTile perioperative morbidity (such as wound breakdown, cerebral edema, readmission, infection) is comparable to craniotomy without GammaTile [44, 58, 59]. There have been over 1,000 GammaTile implants to date [53]. Adverse events (AEs) for patients treated with GammaTile are tracked on the STaRT registry and by manufacturer GT Medical Technologies via post-market surveillance. Using this database, infection rates among all GammaTile cases is ~ 3% (data on file, internal memo. GT Medical Technologies), which is at the baseline infection rate reported for craniotomy without GammaTile [60].
Discussion & conclusion
With any new technology in oncology, the development of mature data takes significant time. Multiple clinical trials are evaluating the efficacy and safety of GammaTile. Pending the completion of these trials, and 5 years after FDA clearance, we have reviewed the accumulated published data across multiple tumor types.
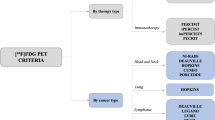
GammaTile is one method of utilizing Cs-131 brachytherapy sources for brain tumors. The other contemporary method that has been reported upon is implantation of vicryl sutures containing Cs-131 seed sources, without the 3-dimensional collagen tile carrier/spacer function. This is often referred to as “stranded seeds.” Table 2 lists the institutional experiences with Cs-131 that include local control and toxicity data that utilized either GammaTile or stranded seeds.
These data suggest LC outcomes with surgery and Cs-131 use for brain metastases, GBM, and meningioma seem promising, particularly in the context of other strategies currently employed for these complicated clinical scenarios and tumor types. In addition, the rate of surgical or radiation AEs after GammaTile use is similar to that of surgery alone or other forms of radiation. Taken together, GammaTile appears to be a useful adjuvant for resected brain tumors.
References
Brown PD, Ballman KV, Cerhan JH et al (2017) Postoperative SRS compared with whole brain radiotherapy for resected metastatic brain disease (NCCTG N107C/CEC·3): a multicentre, randomized, controlled, phase 3 trial. Lancet Oncol 18(8):1049–1060. https://doi.org/10.1016/S1470-2045(17)30441-2
Mahajan A, Ahmed S, McAleer MF et al (2017) Postoperative stereotactic radiosurgery versus observation for completely resected brain metastases: a single-centre, randomized, controlled, phase 3 trial. Lancet Oncol 18(8):1040–1048. https://doi.org/10.1016/S1470-2045(17)30414-X
Breen W, Dooley KE, Twohy E et al (2022) Patterns of failure after stereotactic radiosurgery vs. whole brain radiotherapy for resected brain metastases: central imaging review of the N107C/CEC.3 (Alliance) phase III clinical trial. Int J Radiat Oncol Biol Phys 114(5):1063–1064. https://doi.org/10.1016/j.ijrobp.2022.09.012
Minniti G, Tini P, Giraffa M et al (2023) Feasibility of clinical target volume reduction for glioblastoma treated with standard chemoradiation based on patterns of failure analysis. Radiother Oncol 181:109435. https://doi.org/10.1016/j.radonc.2022.11.024
Vagnoni L, Aburas S, Giraffa M, Russo I, Chiarella V, Paolini S, Tini P, Minniti G (2022) Radiation therapy for atypical and anaplastic meningiomas: an overview of current results and controversial issues. Neurosurg Rev 45(5):3019–3033. https://doi.org/10.1007/s10143-022-01806-3
Waqar M, Roncaroli F, Lehrer EJ et al (2022) Rapid early progression (REP) of glioblastoma is an independent negative prognostic factor: results from a systematic review and meta-analysis. Neuro-oncol Adv. https://doi.org/10.1093/noajnl/vdac075
Jarvis LA, Simmons NE, Bellerive M, Erkmen K, Eskey CJ, Gladstone DJ, Hug EB, Roberts DW, Harford AC (2012) Tumor bed dynamics after surgical resection of brain metastases: implications for postoperative radiosurgery. Int J Radiat Oncol Biol Phys 84(4):943–948. https://doi.org/10.1016/j.ijrobp.2012.01.067
Dharnipragada R, Ferreira C, Shah R, Reynolds M, Dusenbery KE, Chen CC (2023) GammaTile® (GT) as a brachytherapy platform for rapidly growing brain metastasis. Neuro-oncol Adv. https://doi.org/10.1093/noajnl/vdad062
Choi CYH, Chang SD, Gibbs IC et al (2012) Stereotactic radiosurgery of the postoperative resection cavity for brain metastases: prospective evaluation of target margin on tumor control. Int J Radiat Oncol Biol Phys 84(2):336–342. https://doi.org/10.1016/j.ijrobp.2011.12.009
Minniti G, Niyazi M, Andratschke N et al (2021) Current status and recent advances in resection cavity irradiation of brain metastases. Radiat Oncol 16(1):73. https://doi.org/10.1186/s13014-021-01802-9
Shi S, Sandhu N, Jin M et al (2020) Stereotactic radiosurgery for resected brain metastases—does the surgical corridor need to be targeted? Pract Radiat Oncol 10(5):e363–e371. https://doi.org/10.1016/j.prro.2020.04.009
Cabrera AR, Kirkpatrick JP, Fiveash JB et al (2016) Radiation therapy for glioblastoma: executive summary of an American society for radiation oncology evidence-based clinical practice guideline. Pract Radiat Oncol 6(4):217–225. https://doi.org/10.1016/j.prro.2016.03.007
Shi W, Scannell Bryan M, Gilbert MR et al (2018) Investigating the effect of reirradiation or systemic therapy in patients with glioblastoma after tumor progression: a secondary analysis of NRG oncology/radiation therapy oncology group trial 0525. Int J Radiat Oncol Biol Phys 100(1):38–44. https://doi.org/10.1016/j.ijrobp.2017.08.038
Tsien C, Pugh S, Dicker AP et al (2019) Randomized phase II trial of re-irradiation and concurrent bevacizumab versus bevacizumab alone as treatment for recurrent glioblastoma (NRG oncology/RTOG 1205): initial outcomes and RT plan quality report. Int J Radiat Oncol Biol Phys 105(1):S78. https://doi.org/10.1016/j.ijrobp.2019.06.539
Purdy JA (2008) Dose to normal tissues outside the radiation therapy patient’s treated volume: a review of different radiation therapy techniques. Health Phys 95(5):666–676. https://doi.org/10.1097/01.hp.0000326342.47348.06
Bartek J, Alattar AA, Dhawan S, Ma J, Koga T, Nakaji P, Dusenbery KE, Chen CC (2019) Receipt of brachytherapy is an independent predictor of survival in glioblastoma in the surveillance, epidemiology, and end results database. J Neuro-oncol 145(1):75–83. https://doi.org/10.1007/s11060-019-03268-y
Smith K, Nakaji P, Thomas T et al (2022) Safety and patterns of survivorship in recurrent GBM following resection and surgically targeted radiation therapy: results from a prospective trial. Neuro-oncology 24(Supplement6):S4–S15. https://doi.org/10.1093/neuonc/noac133
Blonigen BJ, Steinmetz RD, Levin L, Lamba MA, Warnick RE, Breneman JC (2010) Irradiated volume as a predictor of brain radionecrosis after linear accelerator stereotactic radiosurgery. Int J Radiat Oncol Biol Phys 77(4):996–1001. https://doi.org/10.1016/j.ijrobp.2009.06.006
Brachman DG, Youssef E, Dardis CJ et al (2018) Resection and permanent intracranial brachytherapy using modular, biocompatible cesium-131 implants: results in 20 recurrent, previously irradiated meningiomas. J Neurosurg 131(6):1819–1828. https://doi.org/10.3171/2018.7.jns18656
Nakaji P, Smith K, Youssef E, Thomas T, Pinnaduwage D, Rogers L, Wallstrom G, Brachman D (2020) Resection and surgically targeted radiation therapy for the treatment of larger recurrent or newly diagnosed brain metastasis: results from a prospective trial. Cureus 12(11):e11570. https://doi.org/10.7759/cureus.11570
Raleigh DR, Seymour ZA, Tomlin B et al (2016) Resection and brain brachytherapy with permanent iodine-125 sources for brain metastasis. J Neurosurg 126(6):1749–1755. https://doi.org/10.3171/2016.4.jns152530
Wernicke AG, Smith AW, Taube S et al (2017) Cesium-131 brachytherapy for recurrent brain metastases: durable salvage treatment for previously irradiated metastatic disease. J Neurosurg 126(4):1212–1219. https://doi.org/10.3171/2016.3.JNS152836
Cl Armpilia, Dale RG, Coles IP, Jones B, Antipas V (2003) The determination of radiobiologically optimized half-lives for radionuclides used in permanent brachytherapy implants. Int J Radiat Oncol Biol Phys 55(2):378–385. https://doi.org/10.1016/s0360-3016(02)04208-6
Gessler DJ, Ferreira C, Dusenbery K, Chen CC (2020) GammaTile®: surgically targeted radiation therapy for glioblastomas. Future Oncol 16(30):2445–2455. https://doi.org/10.2217/fon-2020-0558
Han DY, Ma L, Braunstein S, Raleigh D, Sneed PK, McDermott M (2018) Resection cavity contraction effects in the use of radioactive sources (1–25 versus Cs-131) for intra-operative brain implants. Cureus 10(1):e2079. https://doi.org/10.7759/cureus.2079
Pinnaduwage DS, Srivastava SP, Yan X, Jani S, Brachman DG, Sorensen SP (2022) Dosimetric impacts of source migration, radioisotope type, and decay with permanent implantable collagen tile brachytherapy for brain tumors. Technol Cancer Res Treat 21:15330338221106852. https://doi.org/10.1177/15330338221106852
Odia Y, Gutierrez AN, Kotecha R (2022) Surgically targeted radiation therapy (StaRT) trials for brain neoplasms: a comprehensive review. Neuro-oncology 24(Supplement6):S16–S24. https://doi.org/10.1093/neuonc/noac130
Katlowitz KA, Beckham TH, Kudchadker RJ et al (2023) A novel multimodal approach to refractory brain metastases: a case report. Adv Radiat Oncol 101349:101349. https://doi.org/10.1016/j.adro.2023.101349
Prasad K, Dauer LT, Chu B et al (2022) Patient-specific radiological protection precautions following Cs collagen embedded Cs-131 implantation in the brain. J Appl Clin Méd Phys 23(10):e13776. https://doi.org/10.1002/acm2.13776
Shaffer V (2020) Regulatory guide 8.39 revision 1: Release of patients administered radioactive material. U.S. Nuclear Regulatory Commission. https://www.nrc.gov/docs/ML1923/ML19232A081.pdf. Accessed 13 Sept 2023
Alshreef A, Sterling D, Alaei P, Ferreira C (2020) Radiation safety aspects for GammaTile implant brachytherapy. Abstract presented at: American Association of Physicists in Medicine Annual Meeting; 12–16 July 2020; virtual
Davis BJ, Horwitz EM, Lee WR, Crook JM, Stock RG, Merrick GS, Butler WM, Grimm PD, Stone NN, Potters L, Zietman AL, Zelefsky MJ (2012) American brachytherapy society consensus guidelines for transrectal ultrasound-guided permanent prostate brachytherapy. Brachytherapy 11(1):6–19. https://doi.org/10.1016/j.brachy.2011.07.005
Gessler DJ, Neil EC, Shah R et al (2021) GammaTile® brachytherapy in the treatment of recurrent glioblastomas. Neuro-oncol Adv. https://doi.org/10.1093/noajnl/vdab185
Buszek SM, Tran B, Long JP et al (2023) Postoperative management of recurrence after SRS and surgical resection for brain metastases and predicting benefit from adjuvant radiation. Pract Radiat Oncol. https://doi.org/10.1016/j.prro.2023.05.010
Roth O’Brien DA, Kaye SM, Poppas PJ et al (2021) Time to administration of stereotactic radiosurgery to the cavity after surgery for brain metastases: a real-world analysis. J Neurosurg 135(6):1695–1705. https://doi.org/10.3171/2020.10.JNS201934
Brennan C, Yang TJ, Hilden P et al (2014) A phase 2 trial of stereotactic radiosurgery boost after surgical resection for brain metastases. Int J Radiat Oncol Biol Phys 88(1):130–136. https://doi.org/10.1016/j.ijrobp.2013.09.051
Iorio-Morin C, Mercure-Cyr R, Figueiredo G, Touchette CJ, Masson-Côté L, Mathieu D (2019) Repeat stereotactic radiosurgery for the management of locally recurrent brain metastases. J Neuro-oncol 145(3):551–559. https://doi.org/10.1007/s11060-019-03323-8
Koffer P, Chan J, Rava P et al (2017) Repeat stereotactic radiosurgery for locally recurrent brain metastases. World Neurosurg 104:589–593. https://doi.org/10.1016/j.wneu.2017.04.103
Sneed PK, Mendez JS, Vemer-van den Hoek JG et al (2015) Adverse radiation effect after stereotactic radiosurgery for brain metastases: incidence, time course, and risk factors. J Neurosurg 123(2):373–386. https://doi.org/10.3171/2014.10.jns141610
McKay WH, McTyre ER, Okoukoni C et al (2017) Repeat stereotactic radiosurgery as salvage therapy for locally recurrent brain metastases previously treated with radiosurgery. J Neurosurg 127(1):148–156. https://doi.org/10.3171/2016.5.JNS153051
Wilcox JA, Brown S, Reiner AS et al (2021) Salvage resection of recurrent previously irradiated brain metastases: tumor control and radiation necrosis dependency on adjuvant re-irradiation. J Neuro-oncol 155(3):277–286. https://doi.org/10.1007/s11060-021-03872-x
Holt DE, Gill BS, Clump DA et al (2015) Tumor bed radiosurgery following resection and prior stereotactic radiosurgery for locally persistent brain metastasis. Front Oncol 5:84. https://doi.org/10.3389/fonc.2015.00084
Kumar AMS, Miller J, Hoffer SA et al (2018) Postoperative hypofractionated stereotactic brain radiation (HSRT) for resected brain metastases: improved local control with higher BED10. J Neuro-oncol 139(2):449–454. https://doi.org/10.1007/s11060-018-2885-6
Imber BS, Young RJ, Beal K et al (2022) Salvage resection plus cesium-131 brachytherapy durably controls post-SRS recurrent brain metastases. J Neuro-oncol 159(3):609–618. https://doi.org/10.1007/s11060-022-04101-9
Kutuk T, Tolakanahalli R, Chaswal V et al (2023) Surgically targeted radiation therapy (STaRT) for recurrent brain metastases: initial clinical experience. Brachytherapy. https://doi.org/10.1016/j.brachy.2023.08.002
Prabhu RS, Turner BE, Asher AL et al (2021) Leptomeningeal disease and neurologic death after surgical resection and radiosurgery for brain metastases: a multi-institutional analysis. Adv Radiat Oncol 6(2):100644. https://doi.org/10.1016/j.adro.2021.100644
Ogura K, Mizowaki T, Arakawa Y et al (2013) Initial and cumulative recurrence patterns of glioblastoma after temozolomide-based chemoradiotherapy and salvage treatment: a retrospective cohort study in a single institution. Radiat Oncol 8(1):97. https://doi.org/10.1186/1748-717x-8-97
Gaspar LE, Fisher BJ, Macdonald DR et al (1992) Supratentorial malignant glioma: patterns of recurrence and implications for external beam local treatment. Int J Radiat Oncol Biol Phys 24(1):55–57. https://doi.org/10.1016/0360-3016(92)91021-e
Petrecca K, Guiot MC, Panet-Raymond V, Souhami L (2012) Failure pattern following complete resection plus radiotherapy and temozolomide is at the resection margin in patients with glioblastoma. J Neuro-oncol 111(1):19–23. https://doi.org/10.1007/s11060-012-0983-4
Mandl ES, Dirven CMF, Buis DR, Postma TJ, Vandertop WP (2008) Repeated surgery for glioblastoma multiforme: only in combination with other salvage therapy. Surg Neurol 69(5):506–509. https://doi.org/10.1016/j.surneu.2007.03.043
Stupp R, Taillibert S, Kanner A et al (2017) Effect of tumor-treating fields plus maintenance temozolomide vs maintenance temozolomide alone on survival in patients with glioblastoma: a randomized clinical trial. JAMA 318(23):2306–2316. https://doi.org/10.1001/jama.2017.18718
Stupp R, Wong ET, Kanner AA et al (2012) NovoTTF-100A versus physician’s choice chemotherapy in recurrent glioblastoma: a randomised phase III trial of a novel treatment modality. Eur J Cancer 48(14):2192–2202. https://doi.org/10.1016/j.ejca.2012.04.011
Garcia et al. (2023) Usage trends of collagen tile brachytherapy (GammaTile) for the first 900 orders. Abstract 3874. Congress of Neurological Surgeons. 12th Sept 2023
Buszek SM, Al Feghali KA, Elhalawani H, Chevli N, Allen PK, Chung C (2020) Optimal timing of radiotherapy following gross total or subtotal resection of glioblastoma: a real-world assessment using the national cancer database. Sci Rep 10(1):4926. https://doi.org/10.1038/s41598-020-61701-z
Katsigiannis S, Krischek B, Barleanu S et al (2019) Impact of time to initiation of radiotherapy on survival after resection of newly diagnosed glioblastoma. Radiat Oncol 14(1):73. https://doi.org/10.1186/s13014-019-1272-6
Kruser TJ, Bosch WR, Badiyan SN et al (2019) NRG brain tumor specialists consensus guidelines for glioblastoma contouring. J Neuro-oncol 143(1):157–166. https://doi.org/10.1007/s11060-019-03152-9
Parashar B, Wernicke AG, Pavese A, Singh P, Trichter S, Sabbas A et al (2011) Cesium-131 permanent seed brachytherapy: dosimetric evaluation and radiation exposure to surgeons, radiation oncologists, and staff. Brachytherapy 10(6):508–513. https://doi.org/10.1016/j.brachy.2011.04.002
American Association of Neuropathologists, Inc (2023) Abstracts of the 99th annual meeting June 8–11, 2023 Monterey, California. J Neuropathol Exp Neurol 82(6):489–592. https://doi.org/10.1093/jnen/nlad029
Lee S, STaRT Registry Investigators et al. (2023) Patterns of clinical application and 30-day adverse events for patients with intracranial brain neoplasms undergoing resection and implantation of GammaTile—report from a multicenter study. Abstract presented at: Neurosurgical Society of the Virginias Conference; 25–27 Jan 2023
Jiménez-Martínez E, Cuervo G, Hornero A et al (2019) Risk factors for surgical site infection after craniotomy: a prospective cohort study. Antimicrob Resist Infect Control 8:69. https://doi.org/10.1186/s13756-019-0525-3
Bander ED, Kelly A, Ma X, Christos PJ, Wernicke AG, Stieg PE, Trichter S, Knisely JPS, Ramakrishna R, Schwartz TH (2023) Safety and efficacy of cesium-131 brachytherapy for brain tumors. J Neurooncol 163(2):355–365. https://doi.org/10.1007/s11060-023-04352-0
Chen WC, Lafreniere M, Phuong C, Liu SJ, Baal JD, Lometti M, Morin O, Ziemer B, Vasudevan HN, Lucas CG, Hervey-Jumper SL, Theodosopoulos PV, Magill ST, Fogh S, Nakamura JL, Boreta L, Sneed PK, McDermott MW, Raleigh DR, Braunstein SE (2022) Resection with intraoperative cesium-131 brachytherapy as salvage therapy for recurrent brain tumors. J Neurosurg 21:1–7. https://doi.org/10.3171/2021.10.JNS211886
Julie DA, Lazow SP, Vanderbilt DB, Taube S, Yondorf MZ, Sabbas A, Pannullo S, Schwartz TH, Wernicke AG (2020) A matched-pair analysis of clinical outcomes after intracavitary cesium-131 brachytherapy versus stereotactic radiosurgery for resected brain metastases. J Neurosurg 15(5):1447–1454. https://doi.org/10.3171/2020.3.JNS193419
Wernicke AG, Taube S, Smith AW, Herskovic A, Parashar B, Schwartz TH (2020) Cs-131 brachytherapy for patients with recurrent glioblastoma combined with bevacizumab avoids radiation necrosis while maintaining local control. Brachytherapy 19(5):705–712. https://doi.org/10.1016/j.brachy.2020.06.013
Xia Y, Mashouf LA, Baker BR, Maxwell R, Bettegowda C, Redmond KJ, Kleinberg LR, Lim M (2018) Outcomes of metastatic brain lesions treated with radioactive Cs-131 seeds after surgery: experience from one institution. Cureus 30(7):e3075. https://doi.org/10.7759/cureus.3075
Funding
The authors have no outside funding to disclose.
Author information
Authors and Affiliations
Contributions
MG, AT, and DB wrote the main manuscript text (MG’s focus was on clinical backgrounds for brain metastases, glioblastoma, and meningioma as well as outlining published clinical outcome data for GammaTile. AT‘s focus was on the physics principles, DB‘s focus was on technical aspects of the technology). MG and DB prepared all figures and tables. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
M.G., A.T., and D.B. are employees and stock holders of GT Medical Technologies, Inc. The authors were invited to submit a review by the Editor in Chief, and our aim was to provide an evidence based review based on the published literature.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Garcia, M.A., Turner, A. & Brachman, D.G. The role of GammaTile in the treatment of brain tumors: a technical and clinical overview. J Neurooncol 166, 203–212 (2024). https://doi.org/10.1007/s11060-023-04523-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-023-04523-z