Abstract
Purpose
Resection beyond the contrast-enhanced zone contributed to reduce tumor burden and prolong survival in glioblastomas. The optimal extent of resection (EOR) and how to achieve it are worthy of continuous investigation for obtaining a satisfactory balance between maximal resection and the preservation of neurological function.
Methods
A total of 340 adult supratentorial lobar glioblastomas (included astrocytoma, WHO 4, IDH mutation and glioblastoma) were retrospectively evaluated. The clinical data, EOR, technique of resection, postoperative complications, overall survival (OS) and progression-free survival (PFS) were assessed by univariate, multivariate and propensity score matched analysis. Histological staining was performed to comprehend the effect of the membranous structures and the cell distribution in tumoral and peritumoral regions.
Results
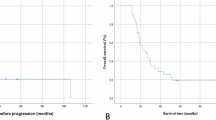
Supramaximal resection (SMR) was confirmed as resection with 100% EORCE and > 50% EORnCE in glioblastomas by Cox proportional hazards model. Histological results showed SMR reduced the cell density of surgical edge compared to total resection. En-bloc technique based on membranous structures, which had blocking effect on tumoral invasion, contributed to achieve SMR. Moreover, applying en-bloc technique and achieving SMR did not additionally deteriorate neurological function and had similarly effects on the improvement of neurological function. Multivariate analysis confirmed that IDH1 status, technique of resection and EOR were independently correlated with PFS, and > 64 years old, IDH1 status, technique of resection, EOR and preoperative NIHSS were independently correlated with OS.
Conclusions
Applying en-bloc technique and achieving SMR, which could reduce tumor burden and did not increase additional complications, both had remarkedly positive effects on clinical outcomes in patients with primary supratentorial lobar glioblastomas.



Similar content being viewed by others
Data availability
The datasets generated during and analyzed during the current study are available from the corresponding author on reasonable request.
References
Hervey-Jumper SL, Berger MS (2016) Maximizing safe resection of low- and high-grade glioma. J Neurooncol 130:269–282. https://doi.org/10.1007/s11060-016-2110-4
Sanai N, Berger MS (2008) Glioma extent of resection and its impact on patient outcome. Neurosurgery 62:753–766. https://doi.org/10.1227/01.neu.0000318159.21731.cf
Ringel F, Pape H, Sabel M et al (2016) Clinical benefit from resection of recurrent glioblastomas: results of a multicenter study including 503 patients with recurrent glioblastomas undergoing surgical resection. Neuro Oncol 18:96–104. https://doi.org/10.1093/neuonc/nov145
Grabowski MM, Recinos PF, Nowacki AS et al (2014) Residual tumor volume versus extent of resection: predictors of survival after surgery for glioblastoma. J Neurosurg 121:1115–1123. https://doi.org/10.3171/2014.7.JNS132449
Suchorska B, Weller M, Tabatabai G et al (2016) Complete resection of contrast-enhancing tumor volume is associated with improved survival in recurrent glioblastoma-results from the DIRECTOR trial. Neuro Oncol 18:549–556. https://doi.org/10.1093/neuonc/nov326
Yordanova YN, Moritz-Gasser S, Duffau H (2011) Awake surgery for WHO grade II gliomas within “noneloquent” areas in the left dominant hemisphere: toward a “supratotal” resection: clinical article. JNS 115:232–239. https://doi.org/10.3171/2011.3.JNS101333
de Leeuw CN, Vogelbaum MA (2019) Supratotal resection in glioma: a systematic review. Neuro Oncol 21:179–188. https://doi.org/10.1093/neuonc/noy166
Rossi M, Ambrogi F, Gay L et al (2020) Is supratotal resection achievable in low-grade gliomas? Feasibility, putative factors, safety, and functional outcome. J Neurosurg 132:1692–1705. https://doi.org/10.3171/2019.2.JNS183408
Molinaro AM, Hervey-Jumper S, Morshed RA et al (2020) Association of maximal extent of resection of contrast-enhanced and non-contrast-enhanced tumor with survival within molecular subgroups of patients with newly diagnosed glioblastoma. JAMA Oncol 6:495–503. https://doi.org/10.1001/jamaoncol.2019.6143
Roh TH, Kang S-G, Moon JH et al (2020) Survival benefit of lobectomy over gross-total resection without lobectomy in cases of glioblastoma in the noneloquent area: a retrospective study. J Neurosurg 132:895–901. https://doi.org/10.3171/2018.12.JNS182558
Shah AH, Mahavadi A, Di L et al (2020) Survival benefit of lobectomy for glioblastoma: moving towards radical supramaximal resection. J Neurooncol 148:501–508. https://doi.org/10.1007/s11060-020-03541-5
Yu L, Zhang G, Qi S (2021) Aggressive treatment in glioblastoma: what determines the survival of patients? J Neurol Surg A Cent Eur Neurosurg 82:112–117. https://doi.org/10.1055/s-0040-1713172
Li YM, Suki D, Hess K, Sawaya R (2016) The influence of maximum safe resection of glioblastoma on survival in 1229 patients: can we do better than gross-total resection? JNS 124:977–988. https://doi.org/10.3171/2015.5.JNS142087
Nogueras JJ, Jagelman DG (1993) Principles of surgical resection. Influence of surgical technique on treatment outcome. Surg Clin N Am 73:103–116. https://doi.org/10.1016/s0039-6109(16)45931-1
Kyoshima K, Akaishi K, Tokushige K et al (2004) Surgical experience with resection en bloc of intramedullary astrocytomas and ependymomas in the cervical and cervicothoracic region. J Clin Neurosci 11:623–628. https://doi.org/10.1016/j.jocn.2003.08.011
Sweeney KJ, Reynolds M, Farrell M, Bolger C (2017) Gross total resection rates of grade II/III intramedullary ependymomas using the surgical strategy of en-bloc resection without intra-operative neurophysiological monitoring. Br J Neurosurg 31:364–368. https://doi.org/10.1080/02688697.2016.1270419
Al-Holou WN, Hodges TR, Everson RG et al (2020) Perilesional resection of glioblastoma is independently associated with improved outcomes. Neurosurgery 86:112–121. https://doi.org/10.1093/neuros/nyz008
Gerritsen JKW, Zwarthoed RH, Kilgallon JL et al (2022) Effect of awake craniotomy in glioblastoma in eloquent areas (GLIOMAP): a propensity score-matched analysis of an international, multicentre, cohort study. Lancet Oncol. https://doi.org/10.1016/S1470-2045(22)00213-3
Lin Z, Yang R, Li K et al (2020) Establishment of age group classification for risk stratification in glioma patients. BMC Neurol 20:310. https://doi.org/10.1186/s12883-020-01888-w
Lemée J-M, Clavreul A, Menei P (2015) Intratumoral heterogeneity in glioblastoma: don’t forget the peritumoral brain zone. Neuro Oncol 17:1322–1332. https://doi.org/10.1093/neuonc/nov119
Jbabdi S, Mandonnet E, Duffau H et al (2005) Simulation of anisotropic growth of low-grade gliomas using diffusion tensor imaging. Magn Reson Med 54:616–624. https://doi.org/10.1002/mrm.20625
Lacroix M, Abi-Said D, Fourney DR et al (2001) A multivariate analysis of 416 patients with glioblastoma multiforme: prognosis, extent of resection, and survival. J Neurosurg 95:190–198. https://doi.org/10.3171/jns.2001.95.2.0190
Keles GE, Chang EF, Lamborn KR et al (2006) Volumetric extent of resection and residual contrast enhancement on initial surgery as predictors of outcome in adult patients with hemispheric anaplastic astrocytoma. JNS 105:34–40. https://doi.org/10.3171/jns.2006.105.1.34
Sanai N, Polley M-Y, McDermott MW et al (2011) An extent of resection threshold for newly diagnosed glioblastomas: clinical article. JNS 115:3–8. https://doi.org/10.3171/2011.2.JNS10998
Marko NF, Weil RJ, Schroeder JL et al (2014) Extent of resection of glioblastoma revisited: personalized survival modeling facilitates more accurate survival prediction and supports a maximum-safe-resection approach to surgery. J Clin Oncol 32:774–782. https://doi.org/10.1200/JCO.2013.51.8886
Silbergeld DL, Chicoine MR (1997) Isolation and characterization of human malignant glioma cells from histologically normal brain. J Neurosurg 86:525–531. https://doi.org/10.3171/jns.1997.86.3.0525
Pallud J, Varlet P, Devaux B et al (2010) Diffuse low-grade oligodendrogliomas extend beyond MRI-defined abnormalities. Neurology 74:1724–1731. https://doi.org/10.1212/WNL.0b013e3181e04264
Rossi M, Gay L, Ambrogi F et al (2021) Association of supratotal resection with progression-free survival, malignant transformation, and overall survival in lower-grade gliomas. Neuro Oncol 23:812–826. https://doi.org/10.1093/neuonc/noaa225
Roelz R, Reinacher P, Jabbarli R et al (2015) Surgical ventricular entry is a key risk factor for leptomeningeal metastasis of high grade gliomas. Sci Rep 5:17758. https://doi.org/10.1038/srep17758
Sonoda Y, Shibahara I, Matsuda K-I et al (2017) Opening the ventricle during surgery diminishes survival among patients with newly diagnosed glioblastoma treated with carmustine wafers: a multi-center retrospective study. J Neurooncol 134:83–88. https://doi.org/10.1007/s11060-017-2488-7
Mistry AM, Kelly PD, Gallant J-N et al (2019) Comparative analysis of subventricular zone glioblastoma contact and ventricular entry during resection in predicting dissemination, hydrocephalus, and survival. Neurosurgery 85:E924–E932. https://doi.org/10.1093/neuros/nyz144
Karschnia P, Barbiero FJ, Schwaiblmair MH et al (2020) Leptomeningeal dissemination of low-grade neuroepithelial CNS tumors in adults: a 15-year experience. Neuro-Oncol Pract 7:118–126. https://doi.org/10.1093/nop/npz020
Behling F, Kaltenstadler M, Noell S et al (2017) The prognostic impact of ventricular opening in glioblastoma surgery: a retrospective single center analysis. World Neurosurg 106:615–624. https://doi.org/10.1016/j.wneu.2017.07.034
Que T, Zheng H, Tan J et al (2021) Ventricle wall resection contributes to supramaximal resection and prognosis in SVZ-involved frontal gliomas: a single center retrospective study. Clin Neurol Neurosurg 211:107015. https://doi.org/10.1016/j.clineuro.2021.107015
Weller M, van den Bent M, Preusser M et al (2021) EANO guidelines on the diagnosis and treatment of diffuse gliomas of adulthood. Nat Rev Clin Oncol 18:170–186. https://doi.org/10.1038/s41571-020-00447-z
Liu R, Page M, Solheim K et al (2009) Quality of life in adults with brain tumors: current knowledge and future directions. Neuro Oncol 11:330–339. https://doi.org/10.1215/15228517-2008-093
Sagberg LM, Solheim O, Jakola AS (2016) Quality of survival the 1st year with glioblastoma: a longitudinal study of patient-reported quality of life. JNS 124:989–997. https://doi.org/10.3171/2015.4.JNS15194
Acknowledgements
None.
Funding
National Natural Science Foundation of China (Grant Number: 81702473, 82102100), Natural Science Foundation of Guangdong Province (Grant Number: 2114050002642), President Fund of Nanfang Hospital (Grant Number: 2018Z015), and Clinical Research Program of Nanfang Hospital (Grant/Award Number: 2020CR017). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by TQ, JT, PZ, ZL, HZ, GY, XX, HX and JL. The first draft of the manuscript was written by TQ and GH, and was revised by SQ and XZ. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors have no relevant financial or non-financial interests to disclose.
Ethical approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committees of Nanfang Hospital (No. 2013-105).
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent to publish
The authors affirm that human research participants provided informed consent for publication of the images in Figs. 1A, B, 2F and Supplementary Figs. 1A.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Que, T., Huang, G., Tan, Je. et al. Supramaximal resection based on en-bloc technique reduces tumor burden and prolongs survival in primary supratentorial lobar glioblastoma. J Neurooncol 164, 557–568 (2023). https://doi.org/10.1007/s11060-023-04399-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-023-04399-z