Abstract
Background
The introduction of Cesium-131 (Cs-131) as a radiation source has led to a resurgence of brachytherapy for central nervous system (CNS) tumors. The aim of this study was to evaluate the safety and efficacy of the largest cohort of Cs-131 patients to-date.
Methods
A retrospective review of all CNS tumors treated with resection and adjuvant Cs-131 brachytherapy at New York-Presbyterian/Weill Cornell from 2010 to 2021 was performed. Overall survival (OS) and local control (LC) were assessed with Kaplan-Meier methodology. Univariable analysis was conducted to identify patient factors associated with local recurrence or radiation necrosis.
Results
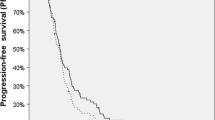
Adjuvant Cs-131 brachytherapy following resection was performed in 119 patients with a median follow-up time of 11.8 (IQR 4.7–23.6) months and a mean of 22.3 +/-30.3 months. 1-year survival rates were 53.3% (95%CI 41.9–64.6%) for brain metastases (BrM), 45.9% (95%CI 24.8–67.0%) for gliomas, and 73.3% (95%CI 50.9–95.7%) for meningiomas. 1-year local control rates were 84.7% for BrM, 34.1% for gliomas, and 83.3% for meningiomas (p < 0.001). For BrM, local control was superior in NSCLC relative to other BrM pathologies (90.8% versus 76.5%, p = 0.039). Radiographic radiation necrosis (RN) was identified in 10 (8.4%) cases and demonstrated an association with smaller median tumor size (2.4 [IQR 1.8-2.7 cm] versus 3.1 [IQR 2.4-3.8 cm], p = 0.034). Wound complications occurred in 14 (11.8%) patients.
Conclusions
Cs-131 brachytherapy demonstrated a favorable safety and efficacy profile characterized by high rates of local control for all treated pathologies. The concept of brachytherapy has seen a resurgence given the excellent results when Cs-131 is used as a source.





Similar content being viewed by others

References
Patchell RA, Tibbs PA, Regine WF et al (1998) Postoperative radiotherapy in the treatment of single metastases to the brain: a randomized trial. JAMA 280(17). https://doi.org/10.1001/jama.280.17.1485
Mahajan A, Ahmed S, McAleer MF et al (2017) Post-operative stereotactic radiosurgery versus observation for completely resected brain metastases: a single-centre, randomised, controlled, phase 3 trial. Lancet Oncol 18(8). https://doi.org/10.1016/S1470-2045(17)30414-X
Stupp R, Mason WP, van den Bent MJ et al (2005) Radiotherapy plus Concomitant and Adjuvant Temozolomide for Glioblastoma. N Engl J Med 352(10). https://doi.org/10.1056/nejmoa043330
Bander ED, Yuan M, Reiner AS et al (2021) Durable 5-year local control for resected brain metastases with early adjuvant SRS: the effect of timing on intended-field control. Neuro-Oncology Pract 8(3). https://doi.org/10.1093/nop/npab005
Roth O’Brien DA, Poppas P, Kaye SM et al (2021) Timing of adjuvant fractionated stereotactic Radiosurgery affects local control of Resected Brain Metastases. Pract Radiat Oncol 11(3). https://doi.org/10.1016/j.prro.2021.01.011
Mahase SS, Navrazhina K, Schwartz TH, Parashar B, Wernicke AG (2019) Intraoperative brachytherapy for resected brain metastases. Brachytherapy 18(3). https://doi.org/10.1016/j.brachy.2019.01.011
Wernicke AG, Taube S, Smith AW, Parashar B (2017) Central Nervous System Brachytherapy. In: Handbook of Image-Guided Brachytherapy.; https://doi.org/10.1007/978-3-319-44827-5_18
Ostertag CB, Kreth FW (1995) Interstitial iodine-125 radiosurgery for cerebral metastases. Br J Neurosurg 9(5). https://doi.org/10.1080/02688699550040873
Prados M, Leibel S, Barnett CM, Gutin P (1989) Interstitial brachytherapy for metastatic brain tumors. Cancer 63(4). https://doi.org/10.1002/1097-0142(19890215)63:4<657::AID-CNCR2820630410>3.0.CO;2-Q
Laperriere NJ, Leung PMK, McKenzie S et al (1998) Randomized study of brachytherapy in the initial management of patients with malignant astrocytoma. Int J Radiat Oncol Biol Phys 41(5). https://doi.org/10.1016/S0360-3016(98)00159-X
Selker RG, Shapiro WR, Burger P et al (2002) The Brain Tumor Cooperative Group NIH Trial 87 – 01: a randomized comparison of surgery, external radiotherapy, and carmustine versus surgery, interstitial radiotherapy boost, external radiation therapy, and carmustine. Neurosurgery 51(2). https://doi.org/10.1097/00006123-200208000-00009
Charfen CO, Sneed PK, Wara WM et al (1992) High activity iodine-125 interstitial implant for gliomas. Int J Radiat Oncol Biol Phys 24(4). https://doi.org/10.1016/0360-3016(92)90702-J
Gutin PH, Prados MD, Phillips TL et al (1991) External irradiation followed by an interstitial high activity iodine-125 implant “boost” in the initial treatment of malignant gliomas: NCOG study 6G-82-2 gliomas: NCOG study 6H-82-2. Int J Radiat Oncol Biol Phys 21(3). https://doi.org/10.1016/0360-3016(91)90676-U
Dagnew E, Kanski J, McDermott MW et al (2007) Management of newly diagnosed single brain metastasis using resection and permanent iodine-125 seeds without initial whole-brain radiotherapy: a two institution experience. Neurosurg Focus 22(3). https://doi.org/10.3171/foc.2007.22.3.4
Raleigh DR, Seymour ZA, Tomlin B et al (2017) Resection and brain brachytherapy with permanent iodine-125 sources for brain metastasis. J Neurosurg 126(6). https://doi.org/10.3171/2016.4.JNS152530
Magill ST, Lau D, Raleigh DR, Sneed PK, Fogh SE, McDermott MW (2017) Surgical resection and interstitial iodine-125 brachytherapy for high-grade meningiomas: a 25-year series. Neurosurgery 80(3). https://doi.org/10.1227/NEU.0000000000001262
Huang K, Sneed PK, Kunwar S et al (2009) Surgical resection and permanent iodine-125 brachytherapy for brain metastases. J Neurooncol 91(1). https://doi.org/10.1007/s11060-008-9686-2
Yondorf MZ, Faraz S, Smith AW et al (2020) Dosimetric differences between cesium-131 and iodine-125 brachytherapy for the treatment of resected brain metastases. J Contemp Brachytherapy 12(4). https://doi.org/10.5114/jcb.2020.98109
Han DY, Ma L, Braunstein S, Raleigh D, Sneed PK, McDermott M Resection Cavity Contraction Effects in the Use of Radioactive Sources (1–25 versus Cs-131) for Intra-Operative Brain Implants. Cureus. Published online 2018. https://doi.org/10.7759/cureus.2079
Julie DA, Lazow SP, Vanderbilt DB et al (2021) A matched-pair analysis of clinical outcomes after intracavitary cesium-131 brachytherapy versus stereotactic radiosurgery for resected brain metastases. J Neurosurg 134(5). https://doi.org/10.3171/2020.3.JNS193419
Pham A, Yondorf MZ, Parashar B et al (2016) Neurocognitive function and quality of life in patients with newly diagnosed brain metastasis after treatment with intra-operative cesium-131 brachytherapy: a prospective trial. J Neurooncol 127(1). https://doi.org/10.1007/s11060-015-2009-5
Wernicke AG, Yondorf MZ, Peng L et al (2014) Phase I/II study of resection and intraoperative cesium-131 radioisotope brachytherapy in patients with newly diagnosed brain metastases. J Neurosurg 121(2). https://doi.org/10.3171/2014.3.JNS131140
Wernicke AG, Smith AW, Taube S et al (2017) Cesium-131 brachytherapy for recurrent brain metastases: durable salvage treatment for previously irradiated metastatic disease. J Neurosurg 126(4). https://doi.org/10.3171/2016.3.JNS152836
Wernicke AG, Taube S, Smith AW, Herskovic A, Parashar B, Schwartz TH (2020) Cs-131 brachytherapy for patients with recurrent glioblastoma combined with bevacizumab avoids radiation necrosis while maintaining local control. Brachytherapy 19(5). https://doi.org/10.1016/j.brachy.2020.06.013
Wernicke AG, Hirschfeld CB, Smith AW et al (2017) Clinical outcomes of large brain metastases treated with neurosurgical resection and intraoperative Cesium-131 brachytherapy: results of a prospective trial. Int J Radiat Oncol Biol Phys 98(5). https://doi.org/10.1016/j.ijrobp.2017.03.044
Wernicke AG, Lazow SP, Taube S et al (2016) Surgical technique and clinically relevant resection cavity dynamics following implantation of cesium-131 brachytherapy in patients with brain metastases. Oper Neurosurg 12(4). https://doi.org/10.1227/NEU.0000000000000986
Chen WC, Lafreniere M, Phuong C et al Resection with intraoperative cesium-131 brachytherapy as salvage therapy for recurrent brain tumors. J Neurosurg. Published online 2022. https://doi.org/10.3171/2021.10.jns211886
Imber, BS YRBKRAG-LAKSYJA-NDCGBCTVMN (2022). Salvage resection plus cesium-131 brachytherapy durably controls post-SRS recurrent brain metastases. J Neurooncol. ;159(3)
Gessler DJ, Ferreira C, Dusenbery K, Chen CC, GammaTile® (2020) Surgically targeted radiation therapy for glioblastomas. Futur Oncol 16(30). https://doi.org/10.2217/fon-2020-0558
Mooney MA, Bi WL, Cantalino JM et al (2020) Brachytherapy with surgical resection as salvage treatment for recurrent high-grade meningiomas: a matched cohort study. J Neurooncol 146(1). https://doi.org/10.1007/s11060-019-03342-5
Palmisciano P, Haider AS, Balasubramanian K, D’Amico RS, Wernicke AG (2022) The role of cesium-131 brachytherapy in brain tumors: a scoping review of the literature and ongoing clinical trials. J Neurooncol 159(1). https://doi.org/10.1007/s11060-022-04050-3
Brennan C, Yang TJ, Hilden P et al (2014) A phase 2 trial of stereotactic radiosurgery boost after surgical resection for brain metastases. Int J Radiat Oncol Biol Phys 88(1). https://doi.org/10.1016/j.ijrobp.2013.09.051
Mengue L, Bertaut A, Ngo Mbus L et al (2020) Brain metastases treated with hypofractionated stereotactic radiotherapy: 8 years experience after Cyberknife installation. Radiat Oncol 15(1). https://doi.org/10.1186/s13014-020-01517-3
Mathieu D, Kondziolka D, Flickinger JC et al (2008) Tumor bed radiosurgery after resection of cerebral metastases. Neurosurgery 62(4). https://doi.org/10.1227/01.neu.0000316899.55501.8b
Yusuf MB, Amsbaugh MJ, Burton E et al (2018) Increasing time to postoperative stereotactic radiation therapy for patients with resected brain metastases: investigating clinical outcomes and identifying predictors associated with time to initiation. J Neurooncol 136(3). https://doi.org/10.1007/s11060-017-2679-2
Vogelbaum MA, Angelov L, Lee SY, Li L, Barnett GH, Suh JH (2006) Local control of brain metastases by stereotactic radiosurgery in relation to dose to the tumor margin. J Neurosurg 104(6). https://doi.org/10.3171/jns.2006.104.6.907
Petr MJ, McPherson CM, Breneman JC, Warnick RE (2009) Management of newly diagnosed single brain metastasis with surgical resection and permanent I-125 seeds without upfront whole brain radiotherapy. J Neurooncol 92(3 SPEC ISS). https://doi.org/10.1007/s11060-009-9868-6
Wilcox JA, Brown S, Reiner AS et al (2021) Salvage resection of recurrent previously irradiated brain metastases: tumor control and radiation necrosis dependency on adjuvant re-irradiation. J Neurooncol 155(3). https://doi.org/10.1007/s11060-021-03872-x
Sanghvi SM, Lischalk JW, Cai L et al (2017) Clinical outcomes of gastrointestinal brain metastases treated with radiotherapy. Radiat Oncol 12(1). https://doi.org/10.1186/s13014-017-0774-3
Go PH, Klaassen Z, Meadows MC, Chamberlain RS (2011) Gastrointestinal cancer and brain metastasis. Cancer 117(16). https://doi.org/10.1002/cncr.25940
Farnell GF, Buckner JC, Cascino TL, O’Connell MJ, Schomberg PJ, Suman V (1996) Brain metastases from colorectal carcinoma: the long term survivors. Cancer 78(4). https://doi.org/10.1002/(SICI)1097-0142(19960815)78:4<711::AID-CNCR3>3.0.CO;2-H
Goldman DA, Hovinga K, Reiner AS, Esquenazi Y, Tabar V, Panageas KS (2018) The relationship between repeat resection and overall survival in patients with glioblastoma: a time-dependent analysis. J Neurosurg 129(5). https://doi.org/10.3171/2017.6.JNS17393
Botros D, Dux H, Price C, Khalafallah AM, Mukherjee D (2021) Assessing the efficacy of repeat resections in recurrent glioblastoma: a systematic review. Neurosurg Rev 44(3). https://doi.org/10.1007/s10143-020-01331-1
Bloch O, Han SJ, Cha S et al (2012) Impact of extent of resection for recurrent glioblastoma on overall survival: clinical article. J Neurosurg 117(6). https://doi.org/10.3171/2012.9.JNS12504
Gabayan AJ, Green SB, Sanan A et al (2006) GliaSite brachytherapy for treatment of recurrent malignant gliomas: a retrospective multi-institutional analysis. Neurosurgery 58(4). https://doi.org/10.1227/01.NEU.0000194836.07848.69
Larson DA, Suplica JM, Chang SM et al (2004) Permanent iodine 125 brachytherapy in patients with progressive or recurrent glioblastoma multiforme. Neuro Oncol 6(2). https://doi.org/10.1215/S1152851703000425
Florell RC, Macdonald DR, Irish WD et al (1992) Selection bias, survival, and brachytherapy for glioma. J Neurosurg 76(2). https://doi.org/10.3171/jns.1992.76.2.0179
Koch MJ, Agarwalla PK, Royce TJ et al (2019) Brachytherapy as an adjuvant for recurrent atypical and malignant meningiomas. Clin Neurosurg 85(5). https://doi.org/10.1093/neuros/nyz115
Brachman D, Youssef E, Dardis C, Smith K, Pinnaduwage D, Nakaji P (2019) Surgically targeted Radiation Therapy: Safety Profile of Collagen Tile Brachytherapy in 79 recurrent, previously irradiated Intracranial Neoplasms on a prospective clinical trial. Brachytherapy 18(3). https://doi.org/10.1016/j.brachy.2019.04.076
Brachman DG, Youssef E, Dardis CJ et al (2019) Resection and permanent intracranial brachytherapy using modular, biocompatible cesium-131 implants: results in 20 recurrent, previously irradiated meningiomas. J Neurosurg 131(6). https://doi.org/10.3171/2018.7.JNS18656
Blonigen BJ, Steinmetz RD, Levin L, Lamba MA, Warnick RE, Breneman JC (2010) Irradiated volume as a predictor of Brain Radionecrosis after Linear Accelerator Stereotactic Radiosurgery. Int J Radiat Oncol Biol Phys 77(4). https://doi.org/10.1016/j.ijrobp.2009.06.006
Minniti G, Clarke E, Lanzetta G et al (2011) Stereotactic radiosurgery for brain metastases: analysis of outcome and risk of brain radionecrosis. Radiat Oncol 6(1). https://doi.org/10.1186/1748-717X-6-48
Aoyama H, Shirato H, Onimaru R et al (2003) Hypofractionated stereotactic radiotherapy alone without whole-brain irradiation for patients with solitary and oligo brain metastasis using noninvasive fixation of the skull. Int J Radiat Oncol Biol Phys 56(3). https://doi.org/10.1016/S0360-3016(03)00014-2
Elaimy AL, MacKay AR, Lamoreaux WT et al (2011) Clinical outcomes of stereotactic radiosurgery in the treatment of patients with metastatic brain tumors. World Neurosurg 75(5–6). https://doi.org/10.1016/j.wneu.2010.12.006
Linskey ME, Andrews DW, Asher AL et al (2010) The role of stereotactic radiosurgery in the management of patients with newly diagnosed brain metastases: a systematic review and evidence-based clinical practice guideline. J Neurooncol 96(1). https://doi.org/10.1007/s11060-009-0073-4
Acknowledgements
EDB is a Leon Levy Research Fellow, Feil Family Brain and Mind Research Institute.
Funding
n/a.
Author information
Authors and Affiliations
Contributions
Conception and design: THS, EDB, AK . Acquisition, analysis, or interpretation of primary data: AK, EDB, RR, ST, JPSK, PES, GW, THS. Drafting of the manuscript: EDB, AK, THS. Critical revision of the manuscript for important intellectual content: All authors. Statistical analysis: XM, PJC. Administrative, technical, or material support: THS. Supervision: THS.
Corresponding author
Ethics declarations
Conflict of Interest
None to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Evan D. Bander and Alexander Kelly contributed equally to this study.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Bander, E.D., Kelly, A., Ma, X. et al. Safety and efficacy of Cesium-131 brachytherapy for brain tumors. J Neurooncol 163, 355–365 (2023). https://doi.org/10.1007/s11060-023-04352-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-023-04352-0