Abstract
Purpose
This study seeks to expound upon risk factor etiologies for surgical site infection (SSI) and investigate their combinatorial effects on infection rate following craniotomy for neuro-oncologic pathology.
Methods
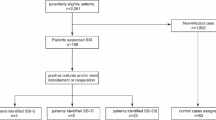
Patients who underwent neuro-oncologic craniotomy between 2006 and 2020 were included. Medical records were reviewed to identify the occurrence of wound infection at ≤ 3 months postoperatively. Potential risk factors for infection included tumor pathology, location, anesthesia type, indication, ventricular entry, foreign body, brachytherapy, lumbar drain, prior operation, prior cranial radiation, prior infection, bevacizumab, and medical comorbidities (hypertension, obesity, diabetes, hyperlipidemia, other cancer, cirrhosis). Logistic regression was implemented to determine risk factors for SSI. Chi-square tests were used to assess whether the number of risk factors (e.g., 0, ≥ 1, ≥2, ≥ 3, ≥4) increases the risk of SSI compared to patients with fewer risk factors. The relative increase with each additional risk factor was also evaluated.
Results
A total of 1209 patients were included. SSI occurred in 42 patients (3.5%) by 90 days after surgery. Significant risk factors on multivariate logistic regression were bevacizumab (OR 40.84; p < 0.001), cirrhosis (OR 14.20, p = 0.03), foreign body placement (OR 4.06; P < 0.0001), prior radiation (OR 2.20; p = 0.03), and prior operation (OR 1.92; p = 0.04). Infection rates in the combinatorial analysis were as follows: ≥1 risk factor = 5.9% (OR 2.74; p = 0.001), ≥ 2 = 6.7% (OR 2.28; p = 0.01), ≥ 3 = 19.0% (OR 6.5; p < 0.0001), ≥ 4 = 100% (OR 30.2; p < 0.0001).
Conclusions
Risk factors in aggregate incrementally increase the risk of postoperative SSI after craniotomy for tumor.

Similar content being viewed by others
Data availability
The datasets generated or analyzed during the current study are available from the corresponding author on reasonable request.
References
Jiménez-Martínez E, Cuervo G, Hornero A et al (2019) Risk factors for surgical site infection after craniotomy: a prospective cohort study. Antimicrob Resist Infect Control 8:69. https://doi.org/10.1186/s13756-019-0525-3
Wang LY, Cao XH, Shi LK, Ma ZZ, Wang Y, Liu Y (2020) Risk factors for intracranial infection after craniotomy: a case-control study. Brain Behav 10(7):e01658. https://doi.org/10.1002/brb3.1658
Patel S, Thompson D, Innocent S, Narbad V, Selway R, Barkas K (2019) Risk factors for surgical site infections in neurosurgery. Ann R Coll Surg Engl 101(3):220–225. https://doi.org/10.1308/rcsann.2019.0001
Fang C, Zhu T, Zhang P, Xia L, Sun C (2017) Risk factors of neurosurgical site infection after craniotomy: a systematic review and meta-analysis. Am J Infect Control 45(11):e123–e134. https://doi.org/10.1016/j.ajic.2017.06.009
Chiang HY, Kamath AS, Pottinger JM et al (2014) Risk factors and outcomes associated with surgical site infections after craniotomy or craniectomy. J Neurosurg 120(2):509–521. https://doi.org/10.3171/2013.9.JNS13843
Maayan O, Babu C, Tusa Lavieri ME, Chua J, Christos PJ, Schwartz TH (2022) Combined use of vancomycin powder and betadine irrigation lowers the incidence of postcraniotomy wound infection in low-risk cases: a single-center risk-stratified cohort analysis. Acta Neurochir (Wien) 164(3):867–874. https://doi.org/10.1007/s00701-021-05075-9
Buchanan IA, Donoho DA, Patel A et al (2018) Predictors of Surgical site infection after nonemergent craniotomy: a Nationwide Readmission Database Analysis. World Neurosurg 120:e440–e452. https://doi.org/10.1016/j.wneu.2018.08.102
Mounier R, Lobo D, Cook F et al (2015) From the skin to the brain: pathophysiology of colonization and infection of external ventricular drain, a prospective observational study. PLoS ONE 10(11):e0142320. https://doi.org/10.1371/journal.pone.0142320
Smith K, Bergeron E, Hire R, Chandler E, Rosado-Odom V (2022) 780: Antibiotic prophylaxis in postoperative neurosurgical patients with a drain: brief versus extended. Crit Care Med 50(1):384. https://doi.org/10.1097/01.ccm.0000809444.94667.19
Clark AJ, Butowski NA, Chang SM et al (2011) Impact of bevacizumab chemotherapy on craniotomy wound healing. J Neurosurg 114(6):1609–1616. https://doi.org/10.3171/2010.10.JNS101042
Saran F, Chinot OL, Henriksson R et al (2016) Bevacizumab, temozolomide, and radiotherapy for newly diagnosed glioblastoma: comprehensive safety results during and after first-line therapy. Neuro Oncol 18(7):991–1001. https://doi.org/10.1093/neuonc/nov300
Yang Z, Jin C, Chen T et al (2012) Changes in cell cycle, apoptosis and necrosis following the establishment of a (125)I brachytherapy model in the spinal cord in Banna mini-pigs. Oncol Lett 3(2):315–320. https://doi.org/10.3892/ol.2011.489
Dormand EL, Banwell PE, Goodacre TEE (2005) Radiotherapy and wound healing. Int Wound J 2(2):112–127. https://doi.org/10.1111/j.1742-4801.2005.00079.x
Hussein M, Abdellatif M (2019) Continuous lumbar drainage for the Prevention and Management of Perioperative Cerebrospinal Fluid Leakage. Asian J Neurosurg 14(2):473–478. https://doi.org/10.4103/ajns.AJNS_265_18
Kourbeti IS, Vakis AF, Ziakas P et al (2015) Infections in patients undergoing craniotomy: risk factors associated with post-craniotomy meningitis. J Neurosurg 122(5):1113–1119. https://doi.org/10.3171/2014.8.JNS132557
Rutkowski M, Sankaran S (2019) Preoperative risk stratification of patient mortality following elective craniotomy; a comparative analysis of prediction algorithms. J Clin Neurosci 67:24–31. https://doi.org/10.1016/j.jocn.2019.06.037
Anderson DJ (2014) Prevention of surgical site infection: beyond SCIP. AORN J 99(2):315–319. https://doi.org/10.1016/j.aorn.2013.11.007
Anderson DJ, Podgorny K, Berríos-Torres SI et al (2014) Strategies to prevent surgical site infections in acute care hospitals: 2014 update. Infect Control Hosp Epidemiol 35(6):605–627. https://doi.org/10.1086/676022
Potter T, Murayi R, Ahorukomeye P et al (2023) Immediate Titanium Mesh Cranioplasty after Debridement and Craniectomy for Postcraniotomy Surgical Site Infections and Risk factors for reoperation. World Neurosurg 171:e493–e499. https://doi.org/10.1016/j.wneu.2022.12.057
Funding
Jason Chua, MPH and Paul Christos, DrPH, were partially supported by the following grant: Clinical and Translational Science Center at Weill Cornell Medical College (1-UL1-TR002384-01).
Author information
Authors and Affiliations
Contributions
All authors contributed to study conception, material preparation, and data collection/analysis. The manuscript was written by OM and THS. All authors commented on previous versions of the manuscript, as well as approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors report no conflict of interest concerning the materials, methods, or findings specified in this study.
Ethics approval and patient consent
This is a retrospective cohort study. The Institutional Review Board at NewYork-Presbyterian Hospital-Weill Cornell Medicine has confirmed that no ethical approval or patient consent was required (IRB 0606008601).
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Maayan, O., Tusa Lavieri, M.E., Babu, C. et al. Additive risk of surgical site infection from more than one risk factor following craniotomy for tumor. J Neurooncol 162, 337–342 (2023). https://doi.org/10.1007/s11060-023-04294-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-023-04294-7