Abstract
Background and objective
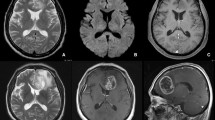
Differentiating neoplastic and non-neoplastic brain lesions is essential to make management recommendations and convey prognosis, but the distinction between brain tumors and their mimics in practice may prove challenging. The aim of this study is to provide the incidence of brain tumor mimics in the neuro-oncology setting and describe this patient subset.
Methods
Retrospective study of adult patients referred to the Division of Neuro-oncology for a presumed diagnosis of brain tumor from January 1, 2005 through December 31, 2017, who later satisfied the diagnosis of a non-neoplastic entity based on neuroimaging, clinical course, and/or histopathology evaluation. We classified tumor mimic entities according to clinical, radiologic, and laboratory characteristics that correlated with the diagnosis.
Results
The incidence of brain tumor mimics was 3.4% (132/3897). The etiologies of the non-neoplastic entities were vascular (35%), inflammatory non-demyelinating (26%), demyelinating (15%), cysts (10%), infectious (9%), and miscellaneous (5%). In our study, 38% of patients underwent biopsy to determine diagnosis, but in 26%, the biopsy was inconclusive.
Discussion
Brain tumor mimics represent a small but important subset of the neuro-oncology referrals. Vascular, inflammatory, and demyelinating etiologies represent two-thirds of cases. Recognizing the clinical, radiologic and laboratory characteristics of such entities may improve resource utilization and prevent unnecessary as well as potentially harmful diagnostic and therapeutic interventions.



Similar content being viewed by others
Data availability
The datasets generated during and analysed during the current study are available from the corresponding author on reasonable request.
References
Anderson MD, Colen RR, Tremont-Lukats IW (2014) Imaging mimics of primary malignant tumors of the central nervous system (CNS). Curr Oncol Rep 16(8):399
Bradley D, Ress J (2013) Brain tumour mimics and chameleons. Pract Neurol 13(6):359–371
Cha S, Pierce S, Knopp EA, Johnson G, Yang C, Ton A et al (2001) Dynamic contrast-enhanced T2*-weighted MR imaging of tumefactive demyelinating lesions. AJNR Am J Neuroradiol 22(6):1109–1116
Chiang IC, Hsieh TJ, Chiu ML, Liu GC, Kuo YT, Lin WC (2009) Distinction between pyogenic brain abscess and necrotic brain tumour using 3-tesla MR spectroscopy, diffusion and perfusion imaging. Br J Radiol 82(982):813–820
Dibble EH, Boxerman JL, Baird GL, Donahue JE, Rogg JM (2017) Toxoplasmosis versus lymphoma: cerebral lesion characterization using DSC-MRI revisited. Clin Neurol Neurosurg 152:84–89
Peterson K, Rosenblum MK, Powers JM, Alvord E, Walker RW, Posner JB (1993) Effect of brain irradiation on demyelinating lesions. Neurology 43(10):2105–2112
Fakhran S, Escott EJ (2008) Pineocytoma mimicking a pineal cyst on imaging: true diagnosis or dilemma or a case of incomplete imaging? AJNR Am J Neuroradiol 29(1):159–163
Llufriu S, Pujol T, Blanco Y et al (2010) T2 hypointense rims and ring-enhancing lesions in MS. Mult Scler 16(11):1317–1325
Pastel DA, Mamourian AC, Duhaime AC (2009) Internal structure in pineal cysts on high-resolution magnetic resonance imaging: not a sign of malignancy. J Neurosurg Pediatr. 4(1):81–4. https://doi.org/10.3171/2008.5.17681
Osborn AG, Preece MT (2006) Intracranial cysts: radiologic-pathologic correlation and imaging approach. Radiology 239(3):650–664
Goldring S, Gregorie EM (1986) Experience with lesions that mimic gliomas in patients presenting with a chronic seizure disorder. Clin Neurosurg 33:43–70
Michael AS, Levy JM, Paige ML (1990) Cysticercosis mimicking brain neoplasm: MR and CT appearance. J Comput Assist Tomogr 14(5):708–711
Okamoto K, Furusawa T, Ishikawa K, Quadery FA, Sasai K, Tokiguchi S (2004) Mimics of brain tumor on neuroimaging: part I. Radiat Med 22(2):63–76
Okamoto K, Furusawa T, Ishikawa K, Quadery FA, Sasai K, Tokiguchi S (2004) Mimics of brain tumor on neuroimaging: part II. Radiat Med 22(3):135–142
Go JL, Acharya J, Rajamohan AG (2018) Is it or is it not? Brain Tumor Mimics Semin Roentgenol 53(1):62–76
Nakayama M, Naganawa S, Ouyang M, Jones KA, Kim J, Capizzano AA et al (2021) A review of clinical and imaging findings in tumefactive demyelination. AJR Am J Roentgenol. 217:186–197
Cunliffe CH, Fischer I, Monoky D, Law M, Revercomb C, Elrich S et al (2009) Intracranial lesions mimicking neoplasms. Arch Pathol Lab Med 133(1):101–123
Hatzoglou V, Omuro AM, Haque S, Khakoo Y, Ganly I, Oh JH et al (2016) Second-opinion interpretations of neuroimaging studies by oncologic neuroradiologists can help reduce errors in cancer care. Cancer 122(17):2708–2714
Mohammad HR, Boardman J, Howell L, Mills RJ, Emsley HC (2016) Urgent referral for suspected CNS cancer: which clinical features are associated with a positive predictive value of 3 % or more? BMC Neurol 16(1):152
Barboriak DP, Lee L, Provenzale JM (2001) Serial MR imaging of pineal cysts: implications for natural history and follow-up. AJR Am J Roentgenol 176(3):737–743
Mamourian AC, Yarnell T (1991) Enhancement of pineal cysts on MR images. AJNR Am J Neuroradiol 12(4):773–774
Suh CH, Kim HS, Jung SC, Choi CG, Kim SJ (2018) MRI findings in tumefactive demyelinating lesions: a systematic review and meta-analysis. AJNR Am J Neuroradiol 39(9):1643–1649
Wang KY, Idowu OR, Lin DDM (2017) Radiology and imaging for cavernous malformations. Handb Clin Neurol 143:249–266
de Souza JM, Domingues RC, Cruz LC Jr, Domingues FS, Iasbeck T, Gasparetto EL (2008) Susceptibility-weighted imaging for the evaluation of patients with familial cerebral cavernous malformations: a comparison with t2-weighted fast spin-echo and gradient-echo sequences. AJNR Am J Neuroradiol 29(1):154–158
Karonen JO, Partanen PL, Vanninen RL, Vainio PA, Aronen HJ (2001) Evolution of MR contrast enhancement patterns during the first week after acute ischemic stroke. AJNR Am J Neuroradiol 22(1):103–111
Siskas N, Lefkopoulos A, Ioannidis I, Charitandi A, Dimitriadis AS (2003) Cortical laminar necrosis in brain infarcts: serial MRI. Neuroradiology 45(5):283–288
Rawal S, Croul SE, Willinsky RA, Tymianski M, Krings T (2014) Subcortical cystic lesions within the anterior superior temporal gyrus: a newly recognized characteristic location for dilated perivascular spaces. AJNR Am J Neuroradiol 35(2):317–322
Sung J, Jang J, Choi HS, Jung SL, Ahn KJ, Kim BS (2017) Linear sign in cystic brain lesions ≥5 mm: a suggestive feature of perivascular space. Eur Radiol 27(11):4747–4755
Donkol RH, Moghazy KM, Abolenin A (2012) Assessment of gray matter heterotopia by magnetic resonance imaging. World J Radiol. 4(3):90–96
Huang YC, Weng HH, Tsai YT, Huang YC, Hsiao MC, Wu CY, Lin YH, Hsu HL, Lee JD (2009) Periictal magnetic resonance imaging in status epilepticus. Epilepsy Res 86(1):72–81
Kim JE, Kim DG, Paek SH, Jung HW (2003) Stereotactic biopsy for intracranial lesions: reliability and its impact on the planning of treatment. Acta Neurochir (Wien). 145(7):547–54
Williams JA, Bede P, Doherty CP (2017) An exploration of the spectrum of peri-ictal MRI change; a comprehensive literature review. Seizure 50:19–32
Noujaim SE, Rossi MD, Rao SK, Cacciarelli AA, Mendonca RA, Wang AM, Coelho FH (1999) CT and MR imaging of neurocysticercosis. AJR Am J Roentgenol 173(6):1485–1490
Martinez HR, Rangel-Guerra R, Elizondo G, Gonzalez J, Todd LE, Ancer J, Prakash SS (1989) MR imaging in neurocysticercosis: a study of 56 cases. AJNR Am J Neuroradiol 10(5):1011–1019
Starkey J, Kobayashi N, Numaguchi Y, Moritani T (2017) Cytotoxic lesions of the corpus callosum that show restricted diffusion: mechanisms, causes, and manifestations. Radiographics 37(2):562–576
Schaefer PW, Grant PE, Gonzalez RG (2000) Diffusion-weighted MR imaging of the brain. Radiology 217(2):331–345
Feraco P, Donner D, Gagliardo C, Leonardi I, Piccinini S, Del Poggio A, Franciosi R, Petralia B, van den Hauwe L (2020) Cerebral abscesses imaging: a practical approach. J Popul Ther Clin Pharmacol 27(3):e11–e24
Toh CH, Wei KC, Chang CN, Hsu PW, Wong HF, Ng SH et al (2012) Differentiation of pyogenic brain abscesses from necrotic glioblastomas with use of susceptibility-weighted imaging. AJNR Am J Neuroradiol 33(8):1534–1538
Sasagawa A, Mikami T, Kimura Y, Akiyama Y, Sugita S, Hasegawa T et al (2021) Stroke mimics and chameleons from the radiological viewpoint of glioma diagnosis. Neurol Med Chir (Tokyo) 61(2):134–143
Marangoni S, Argentiero V, Tavolato B (2006) Neurosarcoidosis. Clinical description of 7 cases with a proposal for a new diagnostic strategy. J Neurol 253(4):488–495
Abdoli M, Freedman MS (2015) Neuro-oncology dilemma: tumour or tumefactive demyelinating lesion. Mult Scler Relat Disord 4(6):555–566
Dagher AP, Smirniotopoulos J (1996) Tumefactive demyelinating lesions. Neuroradiology 38(6):560–565
Omuro AM, Leite CC, Mokhtari K, Delattre JY (2006) Pitfalls in the diagnosis of brain tumours. The Lancet Neurology 5(11):937–948
Altintas A, Petek B, Isik N, Terzi M, Bolukbasi F, Tavsanli M et al (2012) Clinical and radiological characteristics of tumefactive demyelinating lesions: follow-up study. Mult Scler 18(10):1448–1453
Lapointe E, Li DKB, Traboulsee AL, Rauscher A (2018) What have we learned from perfusion MRI in multiple sclerosis? AJNR Am J Neuroradiol 39(6):994–1000
Mistry N, Dixon J, Tallantyre E, Tench C, Abdel-Fahim R, Jaspan T et al (2013) Central veins in brain lesions visualized with high-field magnetic resonance imaging: a pathologically specific diagnostic biomarker for inflammatory demyelination in the brain. JAMA Neurol 70(5):623–628
Ontaneda D, Sati P, Raza P, Kilbane M, Gombos E, Alvarez E, Azevedo C et al (2021) North American imaging in MS cooperative. Central vein sign: a diagnostic biomarker in multiple sclerosis (CAVS-MS) study protocol for a prospective multicenter trial. Neuroimage Clin. 32:102834
Kim SH, Chang KH, Song IC, Han MH, Kim HC, Kang HS, Han MC (1997) Brain abscess and brain tumor: discrimination with in vivo H-1 MR spectroscopy. Radiology 204(1):239–245
Fritz D, van de Beek D, Brouwer MC (2016) Clinical features, treatment and outcome in neurosarcoidosis: systematic review and meta-analysis. BMC Neurol 16(1):220
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
LVY: design and conceptualization of the study; acquisition of data; analysis and interpretation of data; drafting and revising the manuscript for intellectual content. TK: acquisition of data; analysis and interpretation of data; drafting and revising the manuscript for intellectual content. JD: design and conceptualization of the study; acquisition of data; analysis and interpretation of data; drafting and revising the manuscript for intellectual content. HA: acquisition of data; analysis and interpretation of data; drafting and revising the manuscript for intellectual content. KAP: acquisition of data; analysis and interpretation of data; drafting and revising the manuscript for intellectual content. NMC: acquisition of data; analysis and interpretation of data; drafting and revising the manuscript for intellectual content. MBL: analysis and interpretation, acquisition of data; revising the manuscript for intellectual content. ARA: revising the manuscript for intellectual content. BP: revising the manuscript for intellectual content. DS: provision of data, revising the manuscript for intellectual content. SHP: acquisition of data; analysis and interpretation of data; revising the manuscript for intellectual content. CEF: design and conceptualization of the study; acquisition of data; analysis and interpretation of data; drafting and revising the manuscript for intellectual content.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethical approval
This retrospective study was Health Insurance Portability and Accountability Act compliant and approved by the University of Virginia (UVA) Institutional Review Board, and confirmed that no ethical approval is required.
Informed consent
This is a retrospective study, and we reviewed our IRB-approved database, therefore informed consent was not required from all individual participants included in the study.
Consent for publication
The authors affirm we have a retrospective IRB-approved study in neuroradiology at the University of Virginia for evaluating MRI and associated clinical findings. The IRB at the University of Virginia has waived requirement for consent for these purposes.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Yogendran, L.V., Kalelioglu, T., Donahue, J.H. et al. The landscape of brain tumor mimics in neuro-oncology practice. J Neurooncol 159, 499–508 (2022). https://doi.org/10.1007/s11060-022-04087-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-022-04087-4