Abstract
Purpose
The relationship between peritumoral neuronal activity, early onset clinical seizures, and glioma survival outcomes remains poorly understood. Hyperexcitability on continuous EEG in the peri-operative period was studied as a prognostic biomarker in patients with newly diagnosed IDH-wildtype diffuse glioma.
Methods
A retrospective observational cohort study was performed including adults with newly diagnosed diffuse glioma, absence of IDH1/2 mutations, and continuous EEG monitoring prior to chemoradiation and within 1 month of initial resection. EEG hyperexcitability was defined by the presence of lateralized periodic discharges and/or electrographic seizures. The primary outcome of overall survival was estimated using the Kaplan–Meier method and compared between groups using multivariate Cox proportional hazards model.
Results
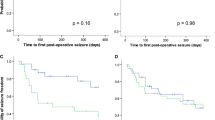
There were 424 patients without continuous EEG and 32 with continuous EEG, of whom lateralized periodic discharges and/or electrographic seizures were seen in 17 (53%). Peri-operative EEG hyperexcitability was associated with decreased overall survival in multivariate analysis (median 12.5 [95% CI 6.2–25.6] months with hyperexcitability versus median 19.9 [95% CI 8.9–53.5] months without hyperexcitability, p = 0.043). Compared to patients without continuous EEG, overall survival was decreased in patients with hyperexcitability (p < 0.0001) and similar in patients without hyperexcitability (p = 0.193). Patients with and without hyperexcitability had similar rates of exposure to anti-seizure medication at baseline, and in long-term follow-up had no difference in number of medications required for seizure control.
Conclusions
These findings indicate the potential prognostic value of a clinical EEG biomarker of glioma aggressiveness prior to the initiation of chemoradiation.



Similar content being viewed by others
Change history
06 July 2022
A Correction to this paper has been published: https://doi.org/10.1007/s11060-022-04086-5
References
Avila EK, Chamberlain M, Schiff D et al (2017) Seizure control as a new metric in assessing efficacy of tumor treatment in low-grade glioma trials. Neuro Oncol 19:12–21. https://doi.org/10.1093/neuonc/now190
Toledo M, Sarria-Estrada S, Quintana M et al (2015) Prognostic implications of epilepsy in glioblastomas. Clin Neurol Neurosurg 139:166–171. https://doi.org/10.1016/j.clineuro.2015.10.002
Toledo M, Sarria-Estrada S, Quintana M et al (2017) Epileptic features and survival in glioblastomas presenting with seizures. Epilepsy Res 130:1–6. https://doi.org/10.1016/j.eplepsyres.2016.12.013
Lote K, Stenwig AE, Skullerud K, Hirschberg H (1998) prevalence and prognostic significance of epilepsy in patients with gliomas. Eur J Cancer Oxf Engl 34:98–102. https://doi.org/10.1016/s0959-8049(97)00374-2
Berendsen S, Varkila M, Kroonen J et al (2016) Prognostic relevance of epilepsy at presentation in glioblastoma patients. Neuro Oncol 18:700–706. https://doi.org/10.1093/neuonc/nov238
Chen H, Judkins J, Thomas C et al (2017) Mutant IDH1 and seizures in patients with glioma. Neurology 88:1805–1813. https://doi.org/10.1212/WNL.0000000000003911
Venkataramani V, Tanev DI, Strahle C et al (2019) Glutamatergic synaptic input to glioma cells drives brain tumour progression. Nature 573:532–538. https://doi.org/10.1038/s41586-019-1564-x
Venkatesh HS, Morishita W, Geraghty AC et al (2019) Electrical and synaptic integration of glioma into neural circuits. Nature 573:539–545. https://doi.org/10.1038/s41586-019-1563-y
Venkatesh HS, Johung TB, Caretti V et al (2015) Neuronal activity promotes glioma growth through neuroligin-3 secretion. Cell 161:803–816. https://doi.org/10.1016/j.cell.2015.04.012
Touat M, Li YY, Boynton AN et al (2020) Mechanisms and therapeutic implications of hypermutation in gliomas. Nature 580:517–523. https://doi.org/10.1038/s41586-020-2209-9
Louis DN, Perry A, Wesseling P et al (2021) The 2021 WHO Classification of tumors of the central nervous system: a summary. Neuro-Oncol 23:1231–1251. https://doi.org/10.1093/neuonc/noab106
Lee JW, LaRoche S, Choi H et al (2016) Development and feasibility testing of a critical care EEG monitoring database for standardized clinical reporting and multicenter collaborative research. J Clin Neurophysiol 33:133–140. https://doi.org/10.1097/WNP.0000000000000230
Hirsch LJ, Fong MWK, Leitinger M et al (2021) American clinical neurophysiology society’s standardized critical care EEG terminology: 2021 version. J Clin Neurophysiol 38:1–29. https://doi.org/10.1097/WNP.0000000000000806
Wagle N, Berger MF, Davis MJ et al (2012) High-throughput detection of actionable genomic alterations in clinical tumor samples by targeted, massively parallel sequencing. Cancer Discov 2:82–93. https://doi.org/10.1158/2159-8290.CD-11-0184
Garcia EP, Minkovsky A, Jia Y et al (2017) Validation of oncopanel: a targeted next-generation sequencing assay for the detection of somatic variants in cancer. Arch Pathol Lab Med 141:751–758. https://doi.org/10.5858/arpa.2016-0527-OA
Derks J, Wesseling P, Carbo EWS et al (2018) Oscillatory brain activity associates with neuroligin-3 expression and predicts progression free survival in patients with diffuse glioma. J Neurooncol 140:403–412. https://doi.org/10.1007/s11060-018-2967-5
Belgers V, Numan T, Kulik SD et al (2020) Postoperative oscillatory brain activity as an add-on prognostic marker in diffuse glioma. J Neurooncol 147:49–58. https://doi.org/10.1007/s11060-019-03386-7
Numan T, Kulik SD, Moraal B et al (2021) Non-invasively measured brain activity and radiological progression in diffuse glioma. Sci Rep 11:18990. https://doi.org/10.1038/s41598-021-97818-y
Schevon CA, Tobochnik S, Eissa T et al (2019) Multiscale recordings reveal the dynamic spatial structure of human seizures. Neurobiol Dis 127:303–311. https://doi.org/10.1016/j.nbd.2019.03.015
Iliadis G, Kotoula V, Chatzisotiriou A et al (2012) Volumetric and MGMT parameters in glioblastoma patients: survival analysis. BMC Cancer 12:3. https://doi.org/10.1186/1471-2407-12-3
Henker C, Kriesen T, Glass Ä et al (2017) Volumetric quantification of glioblastoma: experiences with different measurement techniques and impact on survival. J Neurooncol 135:391–402. https://doi.org/10.1007/s11060-017-2587-5
Hammoud MA, Sawaya R, Shi W et al (1996) Prognostic significance of preoperative MRI scans in glioblastoma multiforme. J Neurooncol 27:65–73. https://doi.org/10.1007/BF00146086
Pope WB, Sayre J, Perlina A et al (2005) MR imaging correlates of survival in patients with high-grade gliomas. AJNR Am J Neuroradiol 26:2466–2474
Li W-B, Tang K, Chen Q et al (2012) MRI manifestions correlate with survival of glioblastoma multiforme patients. Cancer Biol Med 9:120–123. https://doi.org/10.3969/j.issn.2095-3941.2012.02.007
Palpan Flores A, Vivancos Sanchez C, Roda JM et al (2020) Assessment of pre-operative measurements of tumor size by MRI methods as survival predictors in wild type IDH glioblastoma. Front Oncol 10:1662. https://doi.org/10.3389/fonc.2020.01662
Lee JW, Wen PY, Hurwitz S et al (2010) Morphological characteristics of brain tumors causing seizures. Arch Neurol 67:336–342. https://doi.org/10.1001/archneurol.2010.2
Zaatreh MM, Firlik KS, Spencer DD, Spencer SS (2003) Temporal lobe tumoral epilepsy: characteristics and predictors of surgical outcome. Neurology 61:636–641. https://doi.org/10.1212/01.wnl.0000079374.78589.1b
Zaatreh MM, Spencer DD, Thompson JL et al (2002) Frontal lobe tumoral epilepsy: clinical, neurophysiologic features and predictors of surgical outcome. Epilepsia 43:727–733. https://doi.org/10.1046/j.1528-1157.2002.39501.x
Chaichana KL, Parker SL, Olivi A, Quiñones-Hinojosa A (2009) Long-term seizure outcomes in adult patients undergoing primary resection of malignant brain astrocytomas. Clin Art J Neurosurg 111:282–292. https://doi.org/10.3171/2009.2.JNS081132
van Breemen MSM, Wilms EB, Vecht CJ (2007) Epilepsy in patients with brain tumours: epidemiology, mechanisms, and management. Lancet Neurol 6:421–430. https://doi.org/10.1016/S1474-4422(07)70103-5
Skardelly M, Brendle E, Noell S et al (2015) Predictors of preoperative and early postoperative seizures in patients with intra-axial primary and metastatic brain tumors: a retrospective observational single center study. Ann Neurol 78:917–928. https://doi.org/10.1002/ana.24522
Chang EF, Potts MB, Keles GE et al (2008) Seizure characteristics and control following resection in 332 patients with low-grade gliomas. J Neurosurg 108:227–235. https://doi.org/10.3171/JNS/2008/108/2/0227
Yu K, Lin C-CJ, Hatcher A et al (2020) PIK3CA variants selectively initiate brain hyperactivity during gliomagenesis. Nature 578:166–171. https://doi.org/10.1038/s41586-020-1952-2
Tanaka S, Batchelor TT, Iafrate AJ et al (2019) PIK3CA activating mutations are associated with more disseminated disease at presentation and earlier recurrence in glioblastoma. Acta Neuropathol Commun 7:66. https://doi.org/10.1186/s40478-019-0720-8
Tobochnik S, Pisano W, Lapinskas E et al (2021) Effect of PIK3CA variants on glioma-related epilepsy and response to treatment. Epilepsy Res 175:106681. https://doi.org/10.1016/j.eplepsyres.2021.106681
Yuan Y, Xiang W, Yanhui L et al (2017) Activation of the mTOR signaling pathway in peritumoral tissues can cause glioma-associated seizures. Neurol Sci 38:61–66. https://doi.org/10.1007/s10072-016-2706-7
Acknowledgements
The authors would like to acknowledge the Dana-Farber Cancer Institute Oncology Data Retrieval System (OncDRS) for the aggregation, management, and delivery of the clinical and operational research data used in this project. The content is solely the responsibility of the authors.
Funding
This work was supported by the National Institutes of Health (Grant No. nih/NCI 2P50CA165962-06A1 Sub-Project 5140).
Author information
Authors and Affiliations
Contributions
ST conceived of the study. ST, JWL, and KLL contributed to the study design. ST, EL, and JV contributed to data collection and analysis. ST wrote the main manuscript text and prepared the figures. All authors reviewed and edited the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors have no financial or proprietary interests in any material discussed in this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original version of this article has been revised: Some brackets have been corrected in in the second sentence of the Results paragraph in the Abstract and in the second sentence of the subsection Prognostic value of EEG hyperexcitability in the Results section.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Tobochnik, S., Lapinskas, E., Vogelzang, J. et al. Early EEG hyperexcitability is associated with decreased survival in newly diagnosed IDH-wildtype glioma. J Neurooncol 159, 211–218 (2022). https://doi.org/10.1007/s11060-022-04059-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-022-04059-8