Abstract
Purpose
Six years ago, in 2015, the Focused Ultrasound Foundation sponsored a workshop to discuss, and subsequently transition the landscape, of focused ultrasound as a new therapy for treating glioblastoma.
Methods
This year, in 2021, a second workshop was held to review progress made in the field. Discussion topics included blood–brain barrier opening, thermal and nonthermal tumor ablation, immunotherapy, sonodynamic therapy, and desired focused ultrasound device improvements.
Results
The outcome of the 2021 workshop was the creation of a new roadmap to address knowledge gaps and reduce the time it takes for focused ultrasound to become part of the treatment armamentarium and reach clinical adoption for the treatment of patients with glioblastoma. Priority projects identified in the roadmap include determining a well-defined algorithm to confirm and quantify drug delivery following blood–brain barrier opening, identifying a focused ultrasound-specific microbubble, exploring the role of focused ultrasound for liquid biopsy in glioblastoma, and making device modifications that better support clinical needs.
Conclusion
This article reviews the key preclinical and clinical updates from the workshop, outlines next steps to research, and provides relevant references for focused ultrasound in the treatment of glioblastoma.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Focused ultrasound is an early stage, therapeutic technology that offers possible adjuvant or alternative treatment strategies for glioblastoma (GBM). In May 2021, the Focused Ultrasound Foundation (www.fusfoundation.org) convened its second two-day GBM workshop to engage critical stakeholders, including researchers, clinicians, industry, government, and others, to share and combine knowledge to advance the field. The technology has made great advancements since the first workshop on this topic, which was held in 2015 [1]. For example, 13 clinical trials (Table 1) with three manufacturers (Fig. 1) at 20 centers worldwide are currently underway. Before the virtual workshop, experts recorded 23 educational talks that were made available to attendees one week in advance of the live event. These recordings described several different focused ultrasound mechanisms of action that are in various stages of research to treat GBM (Fig. 2A). During the workshop, attendees addressed burning questions within key topic areas through in-depth and interactive expert panel discussions. This article reviews the key preclinical and clinical updates from the workshop, outlines next steps to research, and provides relevant references for focused ultrasound in the treatment of GBM.
Focused Ultrasound Devices for GBM Treatment. The ExAblate Neuro device uses MRI images during the procedure to guide the focused ultrasound beam. The NaviFUS system is guided by neuronavigation with a previously performed MRI scan to guide the beam to the target region; it can be performed in an office setting. The CarThera SonoCloud device is implanted in the skull overlying the target region and does not use imaging guidance. Image used with Copyright Clearance Center permission from Meng Y, Hynynen K, Lipsman N, Nat Rev Neurol. 2021;17(1):7–22 [46]
Thermal and Mechanical Focused Ultrasound Mechanisms of Action include Blood–Brain Barrier Opening, Sonodynamic Therapy, Radiation Sensitization, Histotripsy, and Liquid Biopsy. A Various thermal and mechanical focused ultrasound mechanisms of action related to power. B Blood–Brain Barrier Opening for Drug Delivery. In the precise location of the focused ultrasound beam, intravenously injected intravenous microbubbles expand and contract causing: 1. Opening of the tight junctions; 2. An increase in the number of transcytotic vesicles; and 3. Decreasing efflux pumps, which contribute to enhanced therapeutic delivery of chemotherapies, antibodies, or cargo-loaded viral particles across the BBB. C Sonodynamic Therapy. An intravenously injected sonosensitizer (5-ALA) crosses the blood–brain barrier, accumulates in tumor cells, and converts to protoporphyrin IX (PpIX). Focused ultrasound activates the PpIX, which generates reactive oxygen species (ROS). ROS causes apoptosis and tumor cell death. D Radiation Sensitization. In the presence of microbubbles, the focused ultrasound beam causes oscillations of injected intravenous microbubbles, which mechanically damages the endothelium (black arrows) and releases ceramide. Along with radiation therapy, ceramide induces endothelial and tumor cell death
Blood–brain barrier opening
The blood–brain barrier (BBB) is an obstacle to the effective treatment of brain tumors with therapeutic agents. Although there are some portions of gliomas that display magnetic resonance imaging (MRI) contrast enhancement suggesting “leaky” vessels that allow extravasation of large molecules, it is known that tumor cells extend far beyond the borders of these enhancing areas; therefore, the intact BBB remains an obstacle in the effective delivery of anti-cancer therapies [2]. When combined with microbubble administration, low-intensity focused ultrasound is a promising technique for BBB opening (BBBO) that has been widely studied across preclinical models with encouraging results [3,4,5] (Fig. 2B). Early-stage clinical trials have also shown safety and feasibility for this technique [6,7,8,9].
Microbubble administration protocol
Microbubbles are an essential component for focused ultrasound–induced BBBO, because the focused ultrasound makes them oscillate, and this vibration creates penetrable gaps in the BBB’s tight endothelial junctions. Various microbubbles have been used for focused ultrasound–induced BBBO, including commercial ultrasound contrast agents and bubbles specifically designed for focused ultrasound BBBO. Agents that are designed for BBBO should (i) easily reach stable cavitation with ultrasound, (ii) have in vivo stability in the blood circulation, and (iii) have shelf stability for storage purposes [10, 11]. The most commonly used commercially available microbubbles for focused ultrasound BBBO are Definity™ (Lantheus Medical Imaging), SonoVue™ (Bracco), Optison™ (GE Healthcare) and Sonazoid™ (GE Healthcare). In a prerecorded talk, Francesco Prada, MD, reviewed various microbubble administration protocols, which can be safely administered via intravenous bolus injection or continuous infusion. More data are needed to conclude the optimal administration protocol [12, 13]. An expert panel featuring Nathan McDannold, PhD, Francesco Prada, MD, Elisa Konofagou, PhD, and Kullervo Hynynen, PhD, discussed this conundrum and shared that, in clinical trials, continuous infusion of microbubbles is being used for safety reasons, but most preclinical work was carried out using bolus injections. There was enthusiastic consensus that a microbubble should be designed specifically for focused ultrasound–induced BBBO.
Sonication parameters
Several focused ultrasound parameters should be considered for safely and effectively inducing BBBO. The sonication parameters used affect the depth of ultrasound penetration and the duration of opening. Nathan McDannold, PhD, reviewed these variables and their common values (Table 2). Other factors that might affect the degree of BBBO are anesthesia, supplemental oxygen, steroid administration, and timing of focused ultrasound in relationship to microbubble administration. Dr. McDannold explained that the penetration depth and the duration of opening is affected by the sonication parameters used. Panelists Nathan McDannold, PhD, Francesco Prada, MD, Elisa Konofagou, PhD, and Kullervo Hynynen, PhD, agreed that there are no well-defined optimal sonication parameters for BBBO; ideally, the parameters used for each patient will lead to maximum drug delivery with minimal tissue damage. They agreed that the best focused ultrasound settings for inducing BBBO will vary based on the size of the molecule being delivered and the type of microbubble being used.
Confirmation of BBBO
After microbubble administration and the application of low-intensity focused ultrasound to the target area, the desired effect of increased permeability of the BBB must be confirmed. Michael Canney, PhD, Nathan McDannold, PhD, Antonis Pouliopoulos, PhD, and Raag Airan, MD, PhD, discussed methods used to confirm BBBO [14, 15]. There was consensus that the most common methods to confirm BBBO are T1-weighted and dynamic contrast-enhanced (DCE) MR imaging, especially in clinical studies. Other methods used, mostly in preclinical models, include fluorescent tracers, mass spectrometry, acoustic backscatter, and passive acoustic mapping. Although MRI works well to confirm increased leakiness of the BBB, better imaging modalities must be investigated to quantify or confirm that the desired drug is reaching the target area in increased concentrations.
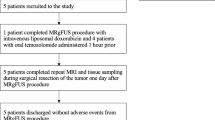
Targeted drug delivery across the BBB
Four presentations highlighted clinical trials involving targeted drug delivery with focused ultrasound–induced BBBO. Nir Lipsman, MD, PhD, Graeme Woodworth, MD, Adam Sonabend, MD, and Ko-Ting Chen, MD, each shared their Phase I and II clinical trial experience. To date, the safety and feasibility of focused ultrasound–induced BBBO has been established with three different clinical devices: InSightec ExAblate, CarThera Sonocloud, and NaviFUS (Fig. 1). Ongoing clinical trials continue to examine safety, feasibility, and outcome data using various chemotherapeutics (Table 1).
The panel discussion moderated by Nir Lipsman, MD, PhD, included Jin Woo Chang, MD, PhD, Alexandra Golby, MD, Adam Sonabend, MD, Roger Stupp, MD, and Graeme Woodworth, MD, who raised important unanswered questions surrounding ongoing and future clinical trials. Most of the current clinical trials are treating patients with recurrent GBM, but there should be more consideration for upfront treatment when there is less tumor heterogeneity. Outcome measures should include progression-free survival and overall survival. Previous studies have shown that greater doses of temozolomide (TMZ) do not affect outcome, so increasing the concentration of TMZ at the site of BBBO is not likely to increase efficacy [16]. A control arm is important to include in focused ultrasound–induced BBBO clinical studies, and Bayesian-designed studies to simultaneously evaluate multiple therapies should be explored.
Delivery of immuno-therapeutics across the BBB
Manmeet Ahluwalia, MD, moderated a panel that included John de Groot, MD, Amy Heimberger, MD, and Patrick Wen, MD, who commented on focused ultrasound–enhanced delivery of immunotherapeutic agents to brain tumors. Immunotherapy has become a pillar of cancer therapy, yet GBMs have yet to be impacted by immunotherapeutics that have helped treat other cancers. Focused ultrasound is a promising technology to potentiate immunotherapeutics [17]. No clinical trials are currently using combination immunotherapy with focused ultrasound, but the group suggested the following therapeutics for GBM therapy during BBBO: immune checkpoint-directed antibodies, adoptive T cells, natural killer (NK) cells, chimeric antigen receptor T cells, and genetically modified antigen-presenting cells. The panel agreed that additional preclinical work was needed, but that it may be too risky to base a large, phase III trial off preclinical data, because mouse models do not sufficiently recapitulate human GBM. Neoadjuvant trials prior to surgery to study whether combination with focused ultrasound could evoke the desired response might be a better approach. Additionally, Dr. Heimberger advised that performing pathology on a small sample of the tumor could provide misleading results because it is unknown whether there is uniform immune cell dispersal throughout the tumor microenvironment (i.e., in GBM, T cells are limited to the perivascular space).
Immunomodulation
Kelsie Timbie, PhD, presented a prerecorded talk on the current state of focused ultrasound immunomodulation research. She provided a review of the literature [18,19,20,21,22,23,24] and described the Foundation’s first multisite GBM consortium project, which began in 2016, to investigate the effects of different focused ultrasound modalities on the immune system and cancer immunity cycle. Each of the seven participating centers used the same animal model of GBM, and results varied. The group using thermal ablation was the only one to achieve tumor growth control. Thermal ablation did not achieve an immune response in the tumor, but hyperthermia increased infiltration of activated NK, effector CD8 cells, and myeloid-derived suppressor cells (MDSC). In contrast, mechanical ablation with histotripsy increased proliferation of CD3-positive, CD4-positive, and CD8-positive T cells. Histotripsy also enhanced dendritic cell activation, decreased MDSCs, and increased interferon gamma production. Overall, the main takeaway was that different focused ultrasound mechanisms have vastly different effects on the immune system.
During the panel discussion, moderator Michael Lim, MD, and panelists Costas Arvanitis, PhD, Timothy Bullock, PhD, Theresa LaVallee, PhD, and Tao Sun, PhD, described several of these immune responses to focused ultrasound and discussed ways to monitor them. Future research suggestions included considering the intersection of focused ultrasound–enhanced immunomodulation with GBM lymphatics and more exactly determining the role of focused ultrasound for GBM immunomodulation. Additional studies are needed to understand the interplay between the various focused ultrasound mechanisms and immunomodulation. New projects could investigate whether focused ultrasound can induce trafficking and activation of immune cells and explore whether focused ultrasound can activate microglia and whether this microglia activation is beneficial in GBM.
Other mechanisms of action
Other focused ultrasound mechanisms of action, such as sonodynamic therapy (SDT), radiation sensitization, and histotripsy have been investigated in preclinical models and are emerging in clinical trials.
SDT
Francesco Prada, MD, discussed “Sonodynamic Therapy: Concept, Mechanisms, and Application to Brain Cancer” in his prerecorded presentation (see Resources section below). Sonodynamic therapy involves activating a sonosensitizing agent (e.g., 5-ALA, fluorescein) with ultrasound, which results in the creation of reactive oxygen species leading to cell death. Sonosensitizers are chemical compounds that selectively accumulate in tumor cells, such as glioblastomas, and are currently used to guide surgical resection because they are also activated by light, which allows for improved intraoperative visualization of the tumor [25]. Panel moderator Jason Sheehan, MD, PhD, and panelists Kullervo Hynynen, PhD, Hao-li Liu, PhD, Stuart Marcus, MD, PhD, and Francesco Prada, MD, all agreed that preclinical data support SDT as a potential treatment for GBM. Although the exact mechanism by which focused ultrasound activates 5-aminolevulinic acid (5-ALA) is not definitively understood, ablation of GBM tumor models due to apoptosis (Fig. 2C) has been achieved in preclinical studies, as evidenced by MRI and histologic evaluation [26,27,28]. Various sonosensitizers, such as 5-ALA and fluorescein, preferentially accumulate in tumoral tissue. Based on the in vivo study on large animals, there is no damage identified to the normal brain with the maximum 5-ALA dose of 100 mg/kg body weight and fluorescein dose of 20 mg/kg body weight, respectively. Intravenous 5-ALA formulation may prove safer than the oral route, because it bypasses the stomach and liver, preventing side effects (e.g., nausea, vomiting) and diminishing changes in liver function tests. In addition, the intravenous formulation may allow for more efficient delivery of 5-ALA to the tumor. There is a current clinical trial (NCT 04559685) using intravenous 5-ALA with focused ultrasound for SDT of GBM in the United States and another study (NCT 04845919) that is using oral 5-ALA in Italy (Table 2).
Radiation sensitization
A prerecorded lecture by Frederic Padilla, PhD, the “Role of Focused Ultrasound for Radiosensitization of GBM,” (see Resources section below) provided an overview of the proposed mechanisms of action for how focused ultrasound causes radiosensitization of tissues. Because resistance to radiation therapy results from tumor hypoxia [29], increasing blood flow and oxygenation could increase radiation sensitization. Various modes of focused ultrasound, such as mild hyperthermia, can increase oxygenation and perfusion [30, 31], and nonthermal effects from focused ultrasound and microbubbles combined to open the BBB have been reported to also improve oxygenation and recruit immune cells (see Chia-Jung Lin brain tumor oral presentation and Hao-Li Liu brain tumor panel at the 2020 Focused Ultrasound International Symposium) [32]. Focused ultrasound and microbubbles can also cause vascular shut down, leading to complete anoxia and contributing to tumor cell death downstream (Fig. 2D) [33, 34]. Greg Czarnota, MD, PhD, moderated a discussion with panelists Hao-Li Liu, PhD, and Frederic Padilla, PhD. The first-in-human clinical trial using the NaviFUS focused ultrasound system for radiosensitization of GBM (NCT 04988750) is now recruiting in Taiwan.
Histotripsy
Zhen Xu, PhD, moderated a discussion on histotripsy as a form of mechanical focused ultrasound ablation. Panelists Tatiana Khoklova, PhD, Joan Vidal-Jove, MD, PhD, and Eli Vlaisavljevich, PhD, provided prerecorded videos on histotripsy for brain applications (see Resources section below). Histotripsy uses focused ultrasound to mechanically destroy tissue, similar to lithotripsy, and can target brain tissue and tumors in a more well-defined region and faster than focused ultrasound thermal ablation with the added benefit of avoiding skull heating. In animal models, some swelling and bleeding have been noted following intracranial histotripsy; therefore, beam parameters (e.g., frequency, number of sonications, treatment time) need to be optimized to avoid complications [35]. Early preclinical results suggest that histotripsy may elicit an immune response. For example, mouse studies in GBM models treated with focused ultrasound released tumor antigens and recruited and activated immune cells, changing the tumor microenvironment from cold to hot [36]. To date, there are no clinical trials with histotripsy for brain tumors.
Technology
Although three clinically available focused ultrasound devices are currently being used for focused ultrasound–induced BBBO in GBM, additional clinical devices are at various stages of development at three institutions. During the workshop, the expert panel on technology gaps and desired features and functionalities was moderated by Elisa Konofagou, PhD, and included Kullervo Hynynen, PhD, Ying Meng, MD, PhD, Graeme Woodworth, MD, and Fred Wu, MD, PhD. The group listed several desired focused ultrasound system improvements, including the ability to expand the treatment envelope so that a greater tumor volume or a two-centimeter margin of tissue around a resection cavity could be treated. They added that brain treatment head frames should be more patient friendly, comfortable, and customized for each skull and tumor location. The current head frames being used for MRI-guided focused ultrasound BBBO are pinned stereotactic head frames that were designed for radiosurgery. Although complete stillness and precision is required for focused ultrasound thermal ablation of brain targets, a less invasive and more comfortable headframe could be designed for the distinct needs of BBBO procedures. Avoiding the need for head shaving is also important for patients. Accurate mathematical modeling algorithms are needed for treatment prediction, and a quality assurance process is needed.
Treatment monitoring
Various imaging modalities and liquid biopsy (LB) are being developed for use in treatment monitoring in focused ultrasound GBM applications.
Radiologic assessment
Benjamin Ellingson, PhD, provided an overview lecture on imaging modalities for GBM monitoring (see Resources below). The modified Response Assessment Neuro Oncology (RANO) criteria is used to evaluate for tumor growth versus pseudo progression and is especially helpful for longitudinal follow-up during adaptive clinical trials to mitigate false negative and false positive results [37]. Other advanced techniques to quantify vascular permeability with focused ultrasound studies include DCE MRI [38] and contrast-enhanced (CE) T1 digital subtraction maps [39]. Dynamic susceptibility contrast (DSC) MRI also allows for quantification of blood volume, flow, and vessel size [40, 41]. These imaging studies can be incorporated into clinical trials to evaluate mechanisms of action.
Patrick Wen, MD, moderated a discussion with Benjamin Ellingson, PhD, Ali Nabavizadeh, MD, and Max Wintermark, MD, as panelists. Various challenges still exist while evaluating MR imaging studies for extent of tumor infiltration, treatment response, and differentiating progression from pseudo progression. Positron emission tomography scanning with varying tracers has contributed to our understanding of tumor metabolism and can be used to understand how focused ultrasound works and help differentiate progression from pseudo progression. In the future, machine learning and artificial intelligence will assist in evaluating subtle changes in imaging findings during treatment monitoring.
Liquid biopsy (LB)
Ying Meng, MD, PhD, summarized the current knowledge of focused ultrasound–enabled LB for brain tumors (see Resources below). Typically, LB for brain tumors has been limited due to the lower amounts of circulating tumor DNA compared to systemic cancers. This is likely due to decreased flow across the BBB. Several preclinical publications demonstrated the ability to detect analytes from the brain in the peripheral circulation after focused ultrasound–induced BBBO, detailing the possibility of bidirectional flow across the BBB for creating a “window” into the brain (Fig. 3—reprinted with permission from Chen, et. al) [31, 42, 43]. Dr. Meng presented the results of first-in-human data, revealing an increase in the amount of cell-free DNA and neural derived extracellular vesicles released into the peripheral blood after focused ultrasound–induced BBBO to improve temozolomide delivery in clinical trial patients with GBM [44]. In addition, the analytes had a distinct signature with more hypermethylation, making them likely derived from glial and neuronal tissue.
Blood–Brain Barrier Opening for Liquid Biopsy. Blood–brain barrier opening with focused ultrasound (FUS) allows bidirectional flow of molecules. DNA, RNA, and protein tumor markers enter the peripheral circulation, where they can be collected and analyzed. Unpublished image courtesy of Hong Chen, PhD, Washington University in St. Louis
Moderator Chetan Bettegowda, MD, PhD, and panelists Hong Chen, PhD, Ying Meng, MD, and Houtan Noushmehr, PhD, discussed numerous technical issues, such as when to obtain LB after focused ultrasound–induced BBBO, what volume of tissue should be targeted, and which sonication parameters are optimal and how they will vary depending on the size of the analyte. There was consensus regarding the promise of focused ultrasound–induced LB to be used as a progression monitoring tool and to discern progression from pseudo progression. A specific advantage of focused ultrasound is its ability to spatially target a discrete region of the tumor or peritumoral tissues to interrogate the analytes in that specific region.
Clinical trial design
Gautam Mehta, MD, and Gregory Clement, PhD, provided the US Food and Drug Administration perspective on how oncology trials are monitored and described regulatory considerations for conducting combination trials using focused ultrasound. Jessica Foley, PhD, moderated a panel discussion that included Amy Barone, MD, Bennet Blumenkopf, MD, Greg Clement, PhD, Subha Maruvada, PhD, Gautam Mehta, MD, and Matthew Myers, PhD, who commented on on what the FDA requires for drug-device combination procedures and those that combine the use of microbubbles and focused ultrasound. The FDA considers both microbubbles and focused ultrasound devices. A lively discussion covered several aspects of this type of clinical trial design. Evidence for reimbursement, another important aspect of clinical trial design, was discussed by Stephanie Kennan, MBA, and Dee Kolanek, AAS, and moderated by Jessica Foley, PhD. The workshop’s white paper includes more information on these topics [45].
Future directions
The Focused Ultrasound Foundation’s second glioblastoma workshop convened an expert group of clinicians and scientists to share the most current preclinical and clinical advancements in the field of focused ultrasound for GBM. The most advanced application is focused ultrasound–induced BBBO to enhance the delivery of therapeutics to brain tumors, with several ongoing clinical trials. Gaps still exist with this therapy, and most notably include the lack of a well-defined algorithm to confirm and quantify drug delivery following BBBO and a lack of generalizable knowledge on the effect that the type and administration route of microbubbles has on BBBO. These gaps have been identified, and the Foundation is actively working with teams of researchers to address them.
In addition to focused ultrasound–induced BBBO, other promising mechanisms are beginning to gain traction for treating brain tumors. SDT and histotripsy are among the newer focused ultrasound techniques that have particularly encouraging outlooks. Focused ultrasound–enhanced LB is another promising application. The Foundation is dedicated to leveraging its resources to strengthen the science, encourage collaboration, and move these applications forward to improve the lives of patients with GBM as soon as possible.
If you have research or research questions that align with the Focused Ultrasound Foundation’s mission and would like to speak to one of the Brain Tumor Program leads, please contact Lauren Powlovich or Suzanne LeBlang or submit an abstract for funding at: https://www.fusfoundation.org/the-foundation/programs/research.
Data availability
Data sharing is not applicable to this article. No datasets were generated or analyzed.
References
(2015) Focused ultrasound for glioblastoma workshop summary. http://www.fusfoundation.org/images/FUSF_Focused_Ultrasound_for_Glioblastoma_Workshop_May_2021.pdf
Bunevicius A, McDannold NJ, Golby AJ (2020) Focused ultrasound strategies for brain tumor therapy. Oper Neurosurg 19:9–18. https://doi.org/10.1093/ons/opz374
Anastasiadis P, Gandhi D, Guo Y et al (2021) Localized blood–brain barrier opening in infiltrating gliomas with MRI-guided acoustic emissions–controlled focused ultrasound. Proc Natl Acad Sci. https://doi.org/10.1073/pnas.2103280118
Englander ZK, Wei H-J, Pouliopoulos AN et al (2021) Focused ultrasound mediated blood–brain barrier opening is safe and feasible in a murine pontine glioma model. Sci Rep 11:6521. https://doi.org/10.1038/s41598-021-85180-y
Wu S-K, Tsai C-L, Hynynen K (2021) Novel treatment approaches for brain tumour from a blood-brain barrier perspective. Handb Exp Pharmacol. https://doi.org/10.1007/164_2020_408
Park SH, Kim MJ, Jung HH et al (2020) One-year outcome of multiple blood-brain barrier disruptions with temozolomide for the treatment of glioblastoma. Front Oncol 10:1663. https://doi.org/10.3389/fonc.2020.01663
Park SH, Kim MJ, Jung HH et al (2020) Safety and feasibility of multiple blood-brain barrier disruptions for the treatment of glioblastoma in patients undergoing standard adjuvant chemotherapy. J Neurosurg. https://doi.org/10.3171/2019.10.JNS192206
Mainprize T, Lipsman N, Huang Y et al (2019) Blood-brain barrier opening in primary brain tumors with non-invasive MR-guided focused ultrasound: a clinical safety and feasibility study. Sci Rep 9:321. https://doi.org/10.1038/s41598-018-36340-0
Idbaih A, Canney M, Belin L et al (2019) Safety and feasibility of repeated and transient blood-brain barrier disruption by pulsed ultrasound in patients with recurrent glioblastoma. Clin Cancer Res Off J Am Assoc Cancer Res 25:3793–3801. https://doi.org/10.1158/1078-0432.CCR-18-3643
Dauba A, Delalande A, Kamimura HAS et al (2020) Recent advances on ultrasound contrast agents for blood-brain barrier opening with focused ultrasound. Pharmaceutics 12:E1125. https://doi.org/10.3390/pharmaceutics12111125
Wu S-K, Chu P-C, Chai W-Y et al (2017) Characterization of different microbubbles in assisting focused ultrasound-induced blood-brain barrier opening. Sci Rep 7:46689. https://doi.org/10.1038/srep46689
Lapin NA, Gill K, Shah BR, Chopra R (2020) Consistent opening of the blood brain barrier using focused ultrasound with constant intravenous infusion of microbubble agent. Sci Rep 10:16546. https://doi.org/10.1038/s41598-020-73312-9
Quaia E, Gennari AG, Angileri R, Cova MA (2016) Bolus versus continuous infusion of microbubble contrast agent for liver ultrasound by using an automatic power injector in humans: a pilot study. J Clin Ultrasound JCU 44:136–142. https://doi.org/10.1002/jcu.22293
Karakatsani ME, Pouliopoulos AN, Liu M et al (2021) Contrast-free detection of focused ultrasound-induced blood-brain barrier opening using diffusion tensor imaging. IEEE Trans Biomed Eng 68:2499–2508. https://doi.org/10.1109/TBME.2020.3047575
Fan C-H, Lin W-H, Ting C-Y et al (2014) Contrast-enhanced ultrasound imaging for the detection of focused ultrasound-induced blood-brain barrier opening. Theranostics 4:1014–1025. https://doi.org/10.7150/thno.9575
Gilbert MR, Wang M, Aldape KD et al (2013) Dose-dense temozolomide for newly diagnosed glioblastoma: a randomized phase III clinical trial. J Clin Oncol Off J Am Soc Clin Oncol 31:4085–4091. https://doi.org/10.1200/JCO.2013.49.6968
Cohen-Inbar O, Xu Z, Sheehan JP (2016) Focused ultrasound-aided immunomodulation in glioblastoma multiforme: a therapeutic concept. J Ther Ultrasound 4:2. https://doi.org/10.1186/s40349-016-0046-y
van den Bijgaart RJE, Eikelenboom DC, Hoogenboom M et al (2017) Thermal and mechanical high-intensity focused ultrasound: perspectives on tumor ablation, immune effects and combination strategies. Cancer Immunol Immunother 66:247–258. https://doi.org/10.1007/s00262-016-1891-9
Sheybani ND, Price RJ (2019) Perspectives on recent progress in focused ultrasound immunotherapy. Theranostics 9:7749–7758. https://doi.org/10.7150/thno.37131
Sheybani ND, Batts AJ, Mathew AS et al (2020) Focused ultrasound hyperthermia augments release of glioma-derived extracellular vesicles with differential immunomodulatory capacity. Theranostics 10:7436–7447. https://doi.org/10.7150/thno.46534
Chen P-Y, Hsieh H-Y, Huang C-Y et al (2015) Focused ultrasound-induced blood–brain barrier opening to enhance interleukin-12 delivery for brain tumor immunotherapy: a preclinical feasibility study. J Transl Med 13:93. https://doi.org/10.1186/s12967-015-0451-y
Sheybani ND, Breza VR, Paul S et al (2021) ImmunoPET-informed sequence for focused ultrasound-targeted mCD47 blockade controls glioma. J Control Release 331:19–29. https://doi.org/10.1016/j.jconrel.2021.01.023
Ye D, Yuan J, Yue Y et al (2021) Focused ultrasound-enhanced delivery of intranasally administered anti-programmed cell death-ligand 1 antibody to an intracranial murine glioma model. Pharmaceutics 13:190. https://doi.org/10.3390/pharmaceutics13020190
Alkins R, Burgess A, Kerbel R et al (2016) Early treatment of HER2-amplified brain tumors with targeted NK-92 cells and focused ultrasound improves survival. Neuro-Oncol 18:974–981. https://doi.org/10.1093/neuonc/nov318
D’Ammando A, Raspagliesi L, Gionso M et al (2021) Sonodynamic therapy for the treatment of intracranial gliomas. J Clin Med 10:1101. https://doi.org/10.3390/jcm10051101
Yoshida M, Kobayashi H, Terasaka S et al (2019) Sonodynamic therapy for malignant glioma using 220-kHz transcranial magnetic resonance imaging-guided focused ultrasound and 5-aminolevulinic acid. Ultrasound Med Biol 45:526–538. https://doi.org/10.1016/j.ultrasmedbio.2018.10.016
Wu S-K, Santos MA, Marcus SL, Hynynen K (2019) MR-guided focused ultrasound facilitates sonodynamic therapy with 5-aminolevulinic acid in a rat glioma model. Sci Rep 9:10465. https://doi.org/10.1038/s41598-019-46832-2
Prada F, Sheybani N, Franzini A et al (2020) Fluorescein-mediated sonodynamic therapy in a rat glioma model. J Neurooncol 148:445–454. https://doi.org/10.1007/s11060-020-03536-2
Sørensen BS, Horsman MR (2020) Tumor hypoxia: impact on radiation therapy and molecular pathways. Front Oncol 10:562. https://doi.org/10.3389/fonc.2020.00562
Schneider CS, Woodworth GF, Vujaskovic Z, Mishra MV (2020) Radiosensitization of high-grade gliomas through induced hyperthermia: Review of clinical experience and the potential role of MR-guided focused ultrasound. Radiother Oncol J Eur Soc Ther Radiol Oncol 142:43–51. https://doi.org/10.1016/j.radonc.2019.07.017
Zhu L, Altman MB, Laszlo A et al (2019) Ultrasound hyperthermia technology for radiosensitization. Ultrasound Med Biol 45:1025–1043. https://doi.org/10.1016/j.ultrasmedbio.2018.12.007
White papers, symposia and workshop proceedings. In: Focus. Ultrasound found. https://www.fusfoundation.org/for-researchers/resources/white-papers. Accessed 2 Nov 2021
Czarnota GJ, Karshafian R, Burns PN et al (2012) Tumor radiation response enhancement by acoustical stimulation of the vasculature. Proc Natl Acad Sci 109:E2033–E2041. https://doi.org/10.1073/pnas.1200053109
El Kaffas A, Gangeh MJ, Farhat G et al (2018) Tumour vascular shutdown and cell death following ultrasound-microbubble enhanced radiation therapy. Theranostics 8:314–327. https://doi.org/10.7150/thno.19010
Sukovich JR, Cain CA, Pandey AS et al (2018) In vivo histotripsy brain treatment. J Neurosurg. https://doi.org/10.3171/2018.4.JNS172652
Hendricks-Wenger A, Hutchison R, Vlaisavljevich E, Allen IC (2021) Immunological effects of histotripsy for cancer therapy. Front Oncol 11:1999. https://doi.org/10.3389/fonc.2021.681629
Ellingson BM, Wen PY, Cloughesy TF (2017) Modified criteria for radiographic response assessment in glioblastoma clinical trials. Neurotherapeutics 14:307–320. https://doi.org/10.1007/s13311-016-0507-6
Keil VC, Gielen GH, Pintea B et al (2021) DCE-MRI in glioma, infiltration zone and healthy brain to assess angiogenesis: a biopsy study. Clin Neuroradiol 31:1049–1058. https://doi.org/10.1007/s00062-021-01015-3
Ellingson BM, Aftab DT, Schwab GM et al (2018) Volumetric response quantified using T1 subtraction predicts long-term survival benefit from cabozantinib monotherapy in recurrent glioblastoma. Neuro Oncol 20:1411–1418. https://doi.org/10.1093/neuonc/noy054
Sanders JW, Chen HS-M, Johnson JM et al (2021) Synthetic generation of DSC-MRI-derived relative CBV maps from DCE MRI of brain tumors. Magn Reson Med 85:469–479. https://doi.org/10.1002/mrm.28432
Quan G, Zhang K, Liu Y et al (2021) Role of dynamic susceptibility contrast perfusion MRI in glioma progression evaluation. J Oncol 2021:1696387. https://doi.org/10.1155/2021/1696387
Zhu L, Cheng G, Ye D et al (2018) Focused ultrasound-enabled brain tumor liquid biopsy. Sci Rep 8:6553. https://doi.org/10.1038/s41598-018-24516-7
Pacia CP, Zhu L, Yang Y et al (2020) Feasibility and safety of focused ultrasound-enabled liquid biopsy in the brain of a porcine model. Sci Rep 10:7449. https://doi.org/10.1038/s41598-020-64440-3
Meng Y, Pople CB, Suppiah S et al (2021) MR-guided focused ultrasound liquid biopsy enriches circulating biomarkers in patients with brain tumors. Neuro Oncol 23:1789–1797. https://doi.org/10.1093/neuonc/noab057
Foundation hosts glioblastoma workshop. In: Focus. Ultrasound found. https://www.fusfoundation.org/news/foundation-hosts-glioblastoma-workshop?highlight=WyJnbGlvYmxhc3RvbWEiLCJnbGlvYmxhc3RvbWFzIiwid29ya3Nob3AiLCJ3b3Jrc2hvcHMiLCJ3b3Jrc2hvcCdzIiwiZ2xpb2JsYXN0b21hIHdvcmtzaG9wIl0=. Accessed 1 Nov 2021
Meng Y, Hynynen K, Lipsman N (2021) Applications of focused ultrasound in the brain: from thermoablation to drug delivery. Nat Rev Neurol 17:7–22. https://doi.org/10.1038/s41582-020-00418-z
Acknowledgements
The GBM workshop was planned by the Focused Ultrasound Foundation in partnership with the Society for Neuro-Oncology and the Journal of Neuro-oncology AANS Tumor Section. This article is based on the workshop white paper written by Heather Gorby, PhD. Figures 2B, 2C, and 2D were created by Focused Ultrasound Foundation Intern Jackie Brenner. Figure 3 was provided by Hong Chen, PhD, Departments of Biomedical Engineering and Radiation Oncology, Washington University in St. Louis, St. Louis, Missouri, USA.
Resources
A comprehensive summary of the GBM Workshop can be found in the Foundation’s White Paper [45]. To view the workshop video content, including all panel discussions and pre-recorded content, visit the Foundation’s YouTube GBM Workshop Playlist.
Funding
The GBM workshop and the writing of this manuscript were funded by the Focused Ultrasound Foundation.
Author information
Authors and Affiliations
Contributions
All authors contributed to the article’s outline and design. The first draft of the manuscript was divided into sections with each author writing different sections. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interest
None of the authors has financial or other competing interests to disclose that are directly or indirectly related to the work submitted for publication.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Consent to participate
This article does not contain human subjects research.
Consent to publish
This article does not contain human subjects research.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Roberts, J.W., Powlovich, L., Sheybani, N. et al. Focused ultrasound for the treatment of glioblastoma. J Neurooncol 157, 237–247 (2022). https://doi.org/10.1007/s11060-022-03974-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-022-03974-0