Abstract
Purpose
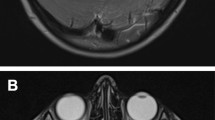
Targeted treatment for brainstem lesions requires above all a precise histopathological and molecular diagnosis. In the current technological era, robot-assisted stereotactic biopsies represent an accurate and safe procedure for tissue diagnosis. We present our center’s experience in frameless robot-assisted biopsies for brainstem lesions.
Methods
We performed a retrospective analysis of all patients benefitting from a frameless robot-guided stereotactic biopsy at our University Hospital, from 2001 to 2017. Patients consented to the use of data and/or images. The NeuroMate® robot (Renishaw™, UK) was used. We report on lesion location, trajectory strategy, histopathological diagnosis and procedure safety.
Results
Our series encompasses 96 patients (103 biopsies) treated during a 17 years period. Mean age at biopsy: 34.0 years (range 1–78). Most common location: pons (62.1%). Transcerebellar approach: 61 procedures (59.2%). Most common diagnoses: diffuse glioma (67.0%), metastases (7.8%) and lymphoma (6.8%). Non conclusive diagnosis: 10 cases (9.7%). After second biopsy this decreased to 4 cases (4.1%). Overall biopsy diagnostic yield: 95.8%. Permanent disability was recorded in 3 patients (2.9%, all adults), while transient complications in 17 patients (17.7%). Four cases of intra-tumoral hematoma were recorded (one case with rapid decline and fatal issue). Adjuvant targeted treatment was performed in 72.9% of patients. Mean follow-up (in the Neurosurgery Department): 2.2 years.
Conclusion
Frameless robot-assisted stereotactic biopsies can provide the initial platform towards a safe and accurate management for brainstem lesions, offering a high diagnostic yield with low permanent morbidity.



Similar content being viewed by others
Data Availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Johnson KJ et al (2014) Childhood brain tumor epidemiology: a brain tumor epidemiology consortium review. Cancer Epidemiol Biomarkers Prev 23(12):2716–2736
Ostrom QT et al (2015) CBTRUS statistical report: primary brain and central nervous system tumors diagnosed in the United States in 2008–2012. Neuro Oncol. https://doi.org/10.1093/neuonc/nov189
Hughes-Hallett A et al (2014) Quantifying innovation in surgery. Ann Surg 260(2):205–211
Kwoh YS et al (1988) A robot with improved absolute positioning accuracy for CT guided stereotactic brain surgery. IEEE Trans Biomed Eng 35(2):153–160
Ughratdar I, Samuel M, Ashkan K (2015) Technological advances in deep brain stimulation. J Parkinsons Dis 5(3):483–496
Gonzalez-Martinez J et al (2016) Technique, results, and complications related to robot-assisted stereoelectroencephalography. Neurosurgery 78(2):169–180
Pillai A et al (2019) Expanding the spectrum of robotic assistance in cranial neurosurgery. Oper Neurosurg (Hagerstown) 17(2):164–173
Marcus HJ et al (2018) Robot-assisted stereotactic brain biopsy: systematic review and bibliometric analysis. Childs Nerv Syst 34(7):1299–1309
Spiegelmann R, Friedman WA (1991) Stereotactic suboccipital transcerebellar biopsy under local anesthesia using the Cosman-Roberts-Wells frame. Technical note. J Neurosurg 75(3):486–488
Bahrami E et al (2020) An experience with frame-based stereotactic biopsy of posterior fossa lesions via transcerebellar route. World Neurosurg. https://doi.org/10.1016/j.wneu.2020.01.003
Quick-Weller J et al (2016) Stereotactic biopsy of brainstem lesions: 21 years experiences of a single center. J Neurooncol 129(2):243–250
Coca HA et al (2016) Diffuse intrinsic pontine gliomas in children: Interest of robotic frameless assisted biopsy. A technical note. Neurochirurgie 62(6):327–331
Williams JR et al (2020) Progress in diffuse intrinsic pontine glioma: advocating for stereotactic biopsy in the standard of care. Neurosurg Focus 48(1):E4
Haegelen C et al (2010) Stereotactic robot-guided biopsies of brain stem lesions: Experience with 15 cases. Neurochirurgie 56(5):363–367
Carai A et al (2017) Robot-assisted stereotactic biopsy of diffuse intrinsic pontine glioma: a single-center experience. World Neurosurg 101:584–588
Dawes W et al (2019) Robot-assisted stereotactic brainstem biopsy in children: prospective cohort study. J Robot Surg 13(4):575–579
Gupta, M., et al., Robot-assisted stereotactic biopsy of pediatric brainstem and thalamic lesions. J Neurosurg Pediatr, 2020: p. 1–8.
Agha RA et al (2020) The PROCESS 2020 Guideline: Updating consensus preferred reporting of CasESeries in surgery (PROCESS) Guidelines. Int J Surg 84:231–235
Louis DN et al (2016) The 2016 World Health Organization classification of tumors of the central nervous system: a summary. Acta Neuropathol 131(6):803–820
Buchanan D (1957) Intracranial tumors in infancy and childhood. Am J Surg 93(6):935–940
Cavalcanti DD et al (2016) Microsurgical anatomy of safe entry zones to the brainstem. J Neurosurg 124(5):1359–1376
Chen SY et al (2011) Stereotactic biopsy for brainstem lesion: comparison of approaches and reports of 10 cases. J Chin Med Assoc 74(3):110–114
Hood TW et al (1986) Stereotaxic biopsy of intrinsic lesions of the brain stem. J Neurosurg 65(2):172–176
Amundson EW, McGirt MJ, Olivi A (2005) A contralateral, transfrontal, extraventricular approach to stereotactic brainstem biopsy procedures. Technical note. J Neurosurg 102(3):565–570
Cavalcanti DD et al (2019) Supracerebellar infratentorial variant approaches to the intercollicular safe entry zone. World Neurosurg 122:e1285–e1290
Recalde RJ, Figueiredo EG, de Oliveira E (2008) Microsurgical anatomy of the safe entry zones on the anterolateral brainstem related to surgical approaches to cavernous malformations. Neurosurgery 62:9–15
Kyoshima K et al (1993) A study of safe entry zones via the floor of the fourth ventricle for brain-stem lesions. Report of three cases. J Neurosurg 78(6):987–993
Quick-Weller J et al (2016) Oblique positioning of the stereotactic frame for biopsies of cerebellar and brainstem lesions. World Neurosurg 86:466–469
Capitanio JF et al (2019) Inverted positioning of Leksell Frame G for very low posterior fossa and brain stem lesions biopsies. J Neurosurg Sci 63(2):194–199
Goncalves-Ferreira AJ, Herculano-Carvalho M, Pimentel J (2003) Stereotactic biopsies of focal brainstem lesions. Surg Neurol 60(4):311–320
Machetanz K et al (2022) Rediscovery of the transcerebellar approach: improving the risk-benefit ratio in robot-assisted brainstem biopsies. Neurosurg Focus 52(1):E12
Kickingereder P et al (2013) Diagnostic value and safety of stereotactic biopsy for brainstem tumors: a systematic review and meta-analysis of 1480 cases. Neurosurgery 72(6):873–881
Hamisch C et al (2017) Update on the diagnostic value and safety of stereotactic biopsy for pediatric brainstem tumors: a systematic review and meta-analysis of 735 cases. J Neurosurg Pediatr 20(3):261–268
Gupta N et al (2018) Prospective feasibility and safety assessment of surgical biopsy for patients with newly diagnosed diffuse intrinsic pontine glioma. Neuro Oncol 20(11):1547–1555
Albright AL et al (1993) Magnetic resonance scans should replace biopsies for the diagnosis of diffuse brain stem gliomas: a report from the Children’s Cancer Group. Neurosurgery 33(6):1026–1029
Louis DN et al (2017) cIMPACT-NOW (the consortium to inform molecular and practical approaches to CNS tumor taxonomy): a new initiative in advancing nervous system tumor classification. Brain Pathol 27(6):851–852
Louis DN et al (2018) cIMPACT-NOW update 2: diagnostic clarifications for diffuse midline glioma, H3 K27M-mutant and diffuse astrocytoma/anaplastic astrocytoma, IDH-mutant. Acta Neuropathol 135(4):639–642
Louis DN et al (2020) cIMPACT-NOW update 6: new entity and diagnostic principle recommendations of the cIMPACT-Utrecht meeting on future CNS tumor classification and grading. Brain Pathol 30(4):844–856
Aziz-Bose R, Monje M (2019) Diffuse intrinsic pontine glioma: molecular landscape and emerging therapeutic targets. Curr Opin Oncol 31(6):522–530
Bush NA, Chang SM, Berger MS (2017) Current and future strategies for treatment of glioma. Neurosurg Rev 40(1):1–14
Law LY et al (2019) The spectrum of immune-mediated and inflammatory lesions of the brainstem: Clues to diagnosis. Neurology 93(9):390–405
Haralur Y, Mechtler LL (2020) Neuroimaging of multiple sclerosis mimics. Neurol Clin 38(1):149–170
Prakkamakul S et al (2017) MRI patterns of isolated lesions in the medulla oblongata. J Neuroimaging 27(1):135–143
Gass A, Filippi M, Grossman RI (2000) The contribution of MRI in the differential diagnosis of posterior fossa damage. J Neurol Sci 172(Suppl 1):S43–S49
Li QH et al (2002) The application accuracy of the NeuroMate robot–A quantitative comparison with frameless and frame-based surgical localization systems. Comput Aided Surg 7(2):90–98
Varma TR, Eldridge P (2006) Use of the NeuroMate stereotactic robot in a frameless mode for functional neurosurgery. Int J Med Robot 2(2):107–113
Lefranc M et al (2014) The impact of the reference imaging modality, registration method and intraoperative flat-panel computed tomography on the accuracy of the ROSA(R) stereotactic robot. Stereotact Funct Neurosurg 92(4):242–250
von Langsdorff D, Paquis P, Fontaine D (2015) In vivo measurement of the frame-based application accuracy of the Neuromate neurosurgical robot. J Neurosurg 122(1):191–194
Widmann G et al (2012) Frameless stereotactic targeting devices: technical features, targeting errors and clinical results. Int J Med Robot 8(1):1–16
Dorward NL et al (1999) Accuracy of true frameless stereotaxy: in vivo measurement and laboratory phantom studies. Technical note. J Neurosurg 90(1):160–168
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Iulia Peciu-Florianu and Victor Legrand. The first draft of the manuscript was written by Iulia Peciu-Florianu and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethical Approval
This research study was conducted retrospectively from data obtained for clinical purposes. We consulted extensively with the IRB of College de Neurochirurgie who determined that our study meet the criteria for ethical approval: n° IRB00011687.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Peciu-Florianu, I., Legrand, V., Monfilliette-Djelad, A. et al. Frameless robot-assisted stereotactic biopsies for lesions of the brainstem—a series of 103 consecutive biopsies. J Neurooncol 157, 109–119 (2022). https://doi.org/10.1007/s11060-022-03952-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-022-03952-6