Abstract
Purpose
Up to 30% of patients with glioblastoma (GBM) develop venous thromboembolism (VTE) over the course of the disease. Although not as high, the risk for VTE is also increased in patients with meningioma. Direct measurement of peak thrombin generation (TG) allows quantitative assessment of systemic coagulation activation in patients with GBM and meningioma. Our aim was to determine the extent of systemic coagulation activation induced by brain tumors, to measure the shift between pre- and post-operative peak TG in patients with GBM, and to assess the relationship between pre-surgical peak TG and pre-operative brain tumor volume on imaging.
Methods
Pre- and post-surgical plasma samples were obtained from successive patients with GBM and once from patients with meningioma and healthy age- and sex-matched blood donor controls. TG was measured using the calibrated automated thrombogram (CAT) assay, and tumor volumes were measured in pre-surgical MRI scans.
Results
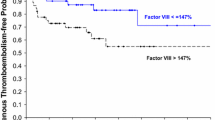
Pre-surgical peak TG was higher in patients with GBM than in controls (288.6 ± 54.1 nM vs 187.1 ± 41.7 nM, respectively, P < 0.001), and, in the nine patients with GBM and paired data available, peak TG was significantly reduced after surgery (323 ± 38 nM vs 265 ± 52 nM, respectively, P = 0.007). Similarly, subjects with meningioma demonstrated higher peak TG compared to controls (242.2 ± 54.9 nM vs 177.7 ± 57.0 nM, respectively, P < 0.001). There was no association between peak TG and pre-operative tumor volume or overall survival.
Conclusion
Our results indicate that systemic coagulation activation occurs with both meningioma and GBM, but to a greater degree in the latter. Preoperative peak TG did not correlate with tumor volume, but removal of GBM caused a significant decrease in coagulation activation.


Similar content being viewed by others
References
Czap AL, Becker A, Wen PY (2019) Thrombotic Complications in Gliomas. Semin Thromb Hemost 45:326–333. https://doi.org/10.1055/s-0039-1687892
Falanga A, Russo L, Milesi V (2014) The coagulopathy of cancer. Curr Opin Hematol 21:423–429. https://doi.org/10.1097/moh.0000000000000072
Marras LC, Geerts WH, Perry JR (2000) The risk of venous thromboembolism is increased throughout the course of malignant glioma: an evidence-based review. Cancer 89:640–646
Muster V, Gary T (2020) Incidence, therapy, and bleeding risk-cancer- associated thrombosis in patients with glioblastoma. Cancers. https://doi.org/10.3390/cancers12061354
Rinaldo L, Brown DA, Bhargav AG, Rusheen AE, Naylor RM, Gilder HE, Monie DD, Youssef SJ, Parney IF (2019) Venous thromboembolic events in patients undergoing craniotomy for tumor resection: incidence, predictors, and review of literature. J Neurosurg 132:10–21. https://doi.org/10.3171/2018.7.Jns181175
Semrad TJ, O’Donnell R, Wun T, Chew H, Harvey D, Zhou H, White RH (2007) Epidemiology of venous thromboembolism in 9489 patients with malignant glioma. J Neurosurg 106:601–608. https://doi.org/10.3171/jns.2007.106.4.601
Streiff MB (2016) Thrombosis in the setting of cancer. Hematol Am Soc Hematol Educ Program 2016:196–205. https://doi.org/10.1182/asheducation-2016.1.196
Cage TA, Lamborn KR, Ware ML, Frankfurt A, Chakalian L, Berger MS, McDermott MW (2009) Adjuvant enoxaparin therapy may decrease the incidence of postoperative thrombotic events though does not increase the incidence of postoperative intracranial hemorrhage in patients with meningiomas. J Neurooncol 93:151–156. https://doi.org/10.1007/s11060-009-9886-4
Carrabba G, Riva M, Conte V, Di Cristofori A, Caroli M, Locatelli M, Castellani M, Bucciarelli P, Artoni A, Stocchetti N, Martinelli I, Rampini P (2018) Risk of post-operative venous thromboembolism in patients with meningioma. J Neurooncol 138:401–406. https://doi.org/10.1007/s11060-018-2810-z
Eisenring CV, Neidert MC, Sabanes Bove D, Held L, Sarnthein J, Krayenbuhl N (2013) Reduction of thromboembolic events in meningioma surgery: a cohort study of 724 consecutive patients. PLoS ONE 8:e79170. https://doi.org/10.1371/journal.pone.0079170
Fluss R, Kobets AJ, Inocencio JF, Hamad M, Feigen C, Altschul DJ, Lasala P (2021) The incidence of venous thromboembolism following surgical resection of intracranial and intraspinal meningioma: a systematic review and retrospective study. Clin Neurol Neurosurg 201:106460. https://doi.org/10.1016/j.clineuro.2020.106460
Hoefnagel D, Kwee LE, van Putten EH, Kros JM, Dirven CM, Dammers R (2014) The incidence of postoperative thromboembolic complications following surgical resection of intracranial meningioma: a retrospective study of a large single center patient cohort. Clin Neurol Neurosurg 123:150–154. https://doi.org/10.1016/j.clineuro.2014.06.001
Sughrue ME, Rutkowski MJ, Shangari G, Chang HQ, Parsa AT, Berger MS, McDermott MW (2011) Risk factors for the development of serious medical complications after resection of meningiomas. Clin Article J Neurosurg 114:697–704. https://doi.org/10.3171/2010.6.Jns091974
Di Nisio M, Porreca E, Otten HM, Rutjes AW (2014) Primary prophylaxis for venous thromboembolism in ambulatory cancer patients receiving chemotherapy. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD008500.pub3
Mantia C, Uhlmann EJ, Puligandla M, Weber GM, Neuberg D, Zwicker JI (2017) Predicting the higher rate of intracranial hemorrhage in glioma patients receiving therapeutic enoxaparin. Blood 129:3379–3385. https://doi.org/10.1182/blood-2017-02-767285
Riedl J, Ay C (2019) Venous thromboembolism in brain tumors: risk factors, molecular mechanisms, and clinical challenges. Semin Thromb Hemost 45:334–341. https://doi.org/10.1055/s-0039-1688493
Becattini C, Di Nisio M, Franco L, Lee A, Agnelli G, Mandalà M (2021) Treatment of venous thromboembolism in cancer patients: the dark side of the moon. Cancer Treat Rev 96:102190. https://doi.org/10.1016/j.ctrv.2021.102190
Lyman GH, Carrier M, Ay C, Di Nisio M, Hicks LK, Khorana AA, Leavitt AD, Lee AYY, Macbeth F, Morgan RL, Noble S, Sexton EA, Stenehjem D, Wiercioch W, Kahale LA, Alonso-Coello P (2021) American Society of Hematology 2021 guidelines for management of venous thromboembolism: prevention and treatment in patients with cancer. Blood Adv 5:927–974. https://doi.org/10.1182/bloodadvances.2020003442
Dicke C, Langer F (2015) Pathophysiology of Trousseau’s syndrome. Hamostaseologie 35:52–59. https://doi.org/10.5482/hamo-14-08-0037
Donati MB, Lorenzet R (2012) Thrombosis and cancer: 40 years of research. Thromb Res 129:348–352. https://doi.org/10.1016/j.thromres.2011.12.022
Geddings JE, Mackman N (2013) Tumor-derived tissue factor-positive microparticles and venous thrombosis in cancer patients. Blood 122:1873–1880. https://doi.org/10.1182/blood-2013-04-460139
Van Dreden P, Epsilonlalamy I, Gerotziafas GT (2017) The role of tissue factor in cancer-related hypercoagulability, tumor growth, angiogenesis and metastasis and future therapeutic strategies. Crit Rev Oncog 22:219–248. https://doi.org/10.1615/CritRevOncog.2018024859
Blix K, Gran OV, Severinsen MT, Cannegieter SC, Jensvoll H, Overvad K, Hammerstrom J, Tjonneland A, Naess IA, Braekkan SK, Rosendaal FR, Kristensen SR, Hansen JB (2018) Impact of time since diagnosis and mortality rate on cancer-associated venous thromboembolism: the Scandinavian Thrombosis and Cancer (STAC) cohort. J Thromb Haemost. https://doi.org/10.1111/jth.14130
Khorana AA, Francis CW (2018) Risk prediction of cancer-associated thrombosis: appraising the first decade and developing the future. Thromb Res 164(Suppl 1):S70-s76. https://doi.org/10.1016/j.thromres.2018.01.036
Khorana AA, Kuderer NM, Culakova E, Lyman GH, Francis CW (2008) Development and validation of a predictive model for chemotherapy-associated thrombosis. Blood 111:4902–4907. https://doi.org/10.1182/blood-2007-10-116327
Konigsbrugge O, Pabinger I, Ay C (2014) Risk factors for venous thromboembolism in cancer: novel findings from the Vienna Cancer and Thrombosis Study (CATS). Thromb Res 133(Suppl 2):S39-43. https://doi.org/10.1016/s0049-3848(14)50007-2
Pabinger I, van Es N, Heinze G, Posch F, Riedl J, Reitter EM, Di Nisio M, Cesarman-Maus G, Kraaijpoel N, Zielinski CC, Buller HR, Ay C (2018) A clinical prediction model for cancer-associated venous thromboembolism: a development and validation study in two independent prospective cohorts. Lancet Haematol 5:e289–e298. https://doi.org/10.1016/s2352-3026(18)30063-2
Patell R, Rybicki L, McCrae KR, Khorana AA (2017) Predicting risk of venous thromboembolism in hospitalized cancer patients: Utility of a risk assessment tool. Am J Hematol 92:501–507. https://doi.org/10.1002/ajh.24700
Shi S, Cheng J, Chen H, Zhang Y, Zhao Y, Wang B (2020) Preoperative and intraoperative predictors of deep venous thrombosis in adult patients undergoing craniotomy for brain tumors: a Chinese single-center, retrospective study. Thromb Res 196:245–250. https://doi.org/10.1016/j.thromres.2020.09.005
Ay C, Dunkler D, Simanek R, Thaler J, Koder S, Marosi C, Zielinski C, Pabinger I (2011) Prediction of venous thromboembolism in patients with cancer by measuring thrombin generation: results from the Vienna Cancer and Thrombosis Study. J Clin Oncol 29:2099–2103. https://doi.org/10.1200/jco.2010.32.8294
Thaler J, Ay C, Kaider A, Reitter EM, Haselbock J, Mannhalter C, Zielinski C, Marosi C, Pabinger I (2014) Biomarkers predictive of venous thromboembolism in patients with newly diagnosed high-grade gliomas. Neuro Oncol 16:1645–1651. https://doi.org/10.1093/neuonc/nou106
Reynes G, Vila V, Martin M, Parada A, Fleitas T, Reganon E, Martinez-Sales V (2011) Circulating markers of angiogenesis, inflammation, and coagulation in patients with glioblastoma. J Neurooncol 102:35–41. https://doi.org/10.1007/s11060-010-0290-x
Reynes G, Vila V, Fleitas T, Reganon E, Font de Mora J, Jorda M, Martinez-Sales V (2013) Circulating endothelial cells and procoagulant microparticles in patients with glioblastoma: prognostic value. PLoS ONE 8:e69034. https://doi.org/10.1371/journal.pone.0069034
Macey MG, Enniks N, Bevan S (2011) Flow cytometric analysis of microparticle phenotype and their role in thrombin generation. Cytometry B 80:57–63. https://doi.org/10.1002/cyto.b.20551
Passamonti SM, Artoni A, Carrabba G, Merati G, Abbattista M, Capecchi M, Castellani M, Marenghi C, Trombetta E, Giammattei L, Caroli M, Bucciarelli P, Scalambrino E, Peyvandi F, Martinelli I (2021) Plasma levels of extracellular vesicles and the risk of post-operative pulmonary embolism in patients with primary brain tumors: a prospective study. J Thromb Thrombolys. https://doi.org/10.1007/s11239-021-02441-3
Ruf W, Mueller BM (2006) Thrombin generation and the pathogenesis of cancer. Semin Thromb Hemost 32(Suppl 1):61–68. https://doi.org/10.1055/s-2006-939555
Ay C, Pabinger I (2010) Tests predictive of thrombosis in cancer. Thromb Res 125(Suppl 2):S12-15. https://doi.org/10.1016/s0049-3848(10)70005-0
Debaugnies F, Azerad MA, Noubouossie D, Rozen L, Hemker HC, Corazza F, Efira A, Demulder A (2010) Evaluation of the procoagulant activity in the plasma of cancer patients using a thrombin generation assay. Thromb Res 126:531–535. https://doi.org/10.1016/j.thromres.2010.09.002
Hemker HC, Giesen PL, Ramjee M, Wagenvoord R, Beguin S (2000) The thrombogram: monitoring thrombin generation in platelet-rich plasma. Thromb Haemost 83:589–591
Fadul CE, Zacharski LR (2005) Coagulation biology in glioma pathogenesis: a missing link? J Thromb Haemost 3:1915–1916. https://doi.org/10.1111/j.1538-7836.2005.01511.x
Haciyakupoğlu E, Yilmaz DM, Walter J, Erdoğan Ş, Haciyakupoğlu S, Kuhn SA (2018) Immunohistochemical evaluation of hemostatic changes in glioblastoma multiforme and low-grade astrocytoma. Turk Neurosurg. https://doi.org/10.5137/1019-5149.Jtn.22739-18.3
Magnus N, D’Asti E, Garnier D, Meehan B, Rak J (2013) Brain neoplasms and coagulation. Semin Thromb Hemost 39:881–895. https://doi.org/10.1055/s-0033-1357483
Navone SE, Guarnaccia L, Locatelli M, Rampini P, Caroli M, La Verde N, Gaudino C, Bettinardi N, Riboni L, Marfia G, Campanella R (2019) Significance and prognostic value of the coagulation profile in patients with glioblastoma: implications for personalized therapy. World Neurosurg 121:e621–e629. https://doi.org/10.1016/j.wneu.2018.09.177
Ornstein DL, Meehan KR, Zacharski LR (2002) The coagulation system as a target for the treatment of human gliomas. Semin Thromb Hemost 28:19–28. https://doi.org/10.1055/s-2002-20561
Sartori MT, Della Puppa A, Ballin A, Campello E, Radu CM, Saggiorato G, d’Avella D, Scienza R, Cella G, Simioni P (2013) Circulating microparticles of glial origin and tissue factor bearing in high-grade glioma: a potential prothrombotic role. Thromb Haemost 110:378–385. https://doi.org/10.1160/th12-12-0957
Wojtukiewicz MZ, Mysliwiec M, Matuszewska E, Sulkowski S, Zimnoch L, Politynska B, Wojtukiewicz AM, Tucker SC, Honn KV (2021) Imbalance in coagulation/fibrinolysis inhibitors resulting in extravascular thrombin generation in gliomas of varying levels of malignancy. Biomolecules. https://doi.org/10.3390/biom11050663
Tawil N, Spinelli C, Bassawon R, Rak J (2020) Genetic and epigenetic regulation of cancer coagulome: lessons from heterogeneity of cancer cell populations. Thromb Res 191(Suppl 1):S99-s105. https://doi.org/10.1016/s0049-3848(20)30405-9
Sartori MT, Della Puppa A, Ballin A, Saggiorato G, Bernardi D, Padoan A, Scienza R, d’Avella D, Cella G (2011) Prothrombotic state in glioblastoma multiforme: an evaluation of the procoagulant activity of circulating microparticles. Journal Neurooncol 104:225–231. https://doi.org/10.1007/s11060-010-0462-8
Thaler J, Preusser M, Ay C, Kaider A, Marosi C, Zielinski C, Pabinger I, Hainfellner JA (2013) Intratumoral tissue factor expression and risk of venous thromboembolism in brain tumor patients. Thromb Res 131:162–165. https://doi.org/10.1016/j.thromres.2012.09.020
Falanga A, Russo L, Milesi V, Vignoli A (2017) Mechanisms and risk factors of thrombosis in cancer. Crit Rev Oncol Hematol 118:79–83. https://doi.org/10.1016/j.critrevonc.2017.08.003
Ellingson BM, Harris RJ, Woodworth DC, Leu K, Zaw O, Mason WP, Sahebjam S, Abrey LE, Aftab DT, Schwab GM, Hessel C, Lai A, Nghiemphu PL, Pope WB, Wen PY, Cloughesy TF (2017) Baseline pretreatment contrast enhancing tumor volume including central necrosis is a prognostic factor in recurrent glioblastoma: evidence from single and multicenter trials. Neuro Oncol 19:89–98. https://doi.org/10.1093/neuonc/now187
Ornstein DL (2008) A nickel’s worth of cancer. Ann Intern Med 149:350–352. https://doi.org/10.7326/0003-4819-149-5-200809020-00010
Acknowledgements
This study was supported by grants from the Northern New England Clinical Oncology Society (NNECOS), the Brain Tumor Research Fund at Dartmouth-Hitchcock Medical Center, and by the Imaging Sciences Group of the Dartmouth Clinical and Translational Science Institute, under award number UL1TR001086 from the National Center for Advancing Translational Sciences (NCATS) of the National Institutes of Health (NIH). The content is solely the responsibility of the author(s) and does not necessarily represent the official views of the funding agencies.
Funding
This study was supported by grants from the Northern New England Clinical Oncology Society (NNECOS), the Brain Tumor Research Fund at Dartmouth-Hitchcock Medical Center, and by the Imaging Sciences Group of the Dartmouth Clinical and Translational Science Institute, under Award Number UL1TR001086 from the National Center for Advancing Translational Sciences (NCATS) of the National Institutes of Health (NIH). The content is solely the responsibility of the author(s) and does not necessarily represent the official views of the funding agencies.
Author information
Authors and Affiliations
Contributions
BLG, CEF and DLO conceived, designed and conducted the study and analyzed thrombin generation data. SY enrolled subjects, collected and analyzed study data. SY, HAW, CEF and DLO provided critical writing of the manuscript. JCF, SRA, SJG, MP and HAW performed tumor volume analyses. MSE contributed to design of the study and provided laboratory support for specimen collection and processing. All authors have reviewed, revised and approved the final submitted manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
Camilo E. Fadul MD is a member of the Editorial Board of the Journal of Neuro-Oncology. Otherwise, the authors declare they have no relevant conflicts of interest or competing interests.
Ethical approval
This study was approved by the Committee for the Protection of Human Subjects (CPHS) of Dartmouth College (study #D12096).
Consent to participate
All study subjects provided written informed consent for participation in this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yerrabothala, S., Gourley, B.L., Ford, J.C. et al. Systemic coagulation is activated in patients with meningioma and glioblastoma. J Neurooncol 155, 173–180 (2021). https://doi.org/10.1007/s11060-021-03865-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-021-03865-w