Abstract
Purpose
Neurosurgeons adopt several different surgical approaches to deal with glioblastomas (GB) located in or near eloquent areas. Some attempt maximal safe resection by awake craniotomy (AC), but doubts persist concerning the real benefits of this type of surgery in this situation. We performed a retrospective study to evaluate the extent of resection (EOR), functional and survival outcomes after AC of patients with GB in critical locations.
Methods
Forty-six patients with primary GB treated with the Stupp regimen between 2004 and 2019, for whom brain mapping was feasible, were included. We assessed EOR, postoperative language and/or motor deficits three months after AC, progression-free survival (PFS) and overall survival (OS).
Results
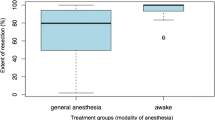
Complete resection was achieved in 61% of the 46 GB patients. The median PFS was 6.8 months (CI 6.1; 9.7) and the median OS was 17.6 months (CI 14.8; 34.1). Three months after AC, more than half the patients asymptomatic before surgery remained asymptomatic, and one third of patients with symptoms before surgery experienced improvements in language, but not motor functions. The risk of postoperative deficits was higher in patients with preoperative deficits or incomplete resection. Furthermore, the presence of postoperative deficits was an independent predictive factor for shorter PFS.
Conclusion
AC is an option for the resection of GB in critical locations. The observed survival outcomes are typical for GB patients in the Stupp era. However, the success of AC in terms of the recovery or preservation of language and/or motor functions cannot be guaranteed, given the aggressiveness of the tumor.



Similar content being viewed by others
Abbreviations
- AC:
-
Awake craniotomy
- EOR:
-
Extent of resection
- GA:
-
General anesthesia
- GB:
-
Glioblastoma
- GTR:
-
Gross total resection
- HGG:
-
High-grade glioma
- HRQoL:
-
Health-related quality of life
- IDH:
-
Isocitrate dehydrogenase
- KPS:
-
Karnofsky performance status
- LGG:
-
Low-grade glioma
- LH:
-
Left hemisphere
- OS:
-
Overall survival
- RH:
-
Right hemisphere
- PFS:
-
Progression-free survival
- PR:
-
Partial resection
- STR:
-
Subtotal resection
References
Giussani C, Di Cristofori A (2020) Awake craniotomy for glioblastomas: is it worth it? Considerations about the article entitled “Impact of intraoperative stimulation mapping on high-grade glioma surgery outcome: a meta-analysis.” Acta Neurochir (Wien) 162:427–428. https://doi.org/10.1007/s00701-019-04173-z
Müller DMJ, Robe PAJT, Eijgelaar RS et al (2019) Comparing glioblastoma surgery decisions between teams using brain maps of tumor locations, biopsies, and resections. JCO Clin Cancer Inform 3:1–12. https://doi.org/10.1200/CCI.18.00089
Duffau H (2018) Is non-awake surgery for supratentorial adult low-grade glioma treatment still feasible? Neurosurg Rev 41:133–139. https://doi.org/10.1007/s10143-017-0918-9
Gerritsen JKW, Viëtor CL, Rizopoulos D et al (2019) Awake craniotomy versus craniotomy under general anesthesia without surgery adjuncts for supratentorial glioblastoma in eloquent areas: a retrospective matched case-control study. Acta Neurochir (Wien) 161:307–315. https://doi.org/10.1007/s00701-018-03788-y
Gerritsen JKW, Arends L, Klimek M et al (2019) Impact of intraoperative stimulation mapping on high-grade glioma surgery outcome: a meta-analysis. Acta Neurochir (Wien) 161:99–107. https://doi.org/10.1007/s00701-018-3732-4
Nakajima R, Kinoshita M, Okita H et al (2019) Awake surgery for glioblastoma can preserve independence level, but is dependent on age and the preoperative condition. J Neurooncol. https://doi.org/10.1007/s11060-019-03216-w
Zhang JJY, Lee KS, Voisin MR et al (2020) Awake craniotomy for resection of supratentorial glioblastoma: a systematic review and meta-analysis. Neuro-Oncol Adv 2:vdaa111. https://doi.org/10.1093/noajnl/vdaa111
Delion M, Klinger E, Bernard F et al (2020) Immersing patients in a virtual reality environment for brain mapping during awake surgery: safety study. World Neurosurg 134:e937–e943. https://doi.org/10.1016/j.wneu.2019.11.047
Pallud J, Rigaux-Viode O, Corns R et al (2017) Direct electrical bipolar electrostimulation for functional cortical and subcortical cerebral mapping in awake craniotomy. Pract Consid Neuroch 63:164–174. https://doi.org/10.1016/j.neuchi.2016.08.009
Duffau H (2011) Brain mapping. Springer, Vienna
Ortiz GA, Sacco RL (2014) National Institutes of Health Stroke Scale (NIHSS). In: Balakrishnan N, Colton T, Everitt B et al (eds) Wiley StatsRef: statistics reference online. Wiley, Chichester
McCormick PC, Torres R, Post KD, Stein BM (1990) Intramedullary ependymoma of the spinal cord. J Neurosurg 72:523–532. https://doi.org/10.3171/jns.1990.72.4.0523
Wen PY, Macdonald DR, Reardon DA et al (2010) Updated response assessment criteria for high-grade gliomas: response assessment in neuro-oncology working group. J Clin Oncol Off J Am Soc Clin Oncol 28:1963–1972. https://doi.org/10.1200/JCO.2009.26.3541
Hrabalek L, Kalita O, Vaverka M et al (2015) Resection versus biopsy of glioblastomas in eloquent brain areas. Biomed Pap Med Fac Univ Palacky Olomouc Czechoslov 159:150–155. https://doi.org/10.5507/bp.2013.052
Coluccia D, Roth T, Marbacher S, Fandino J (2018) Impact of laterality on surgical outcome of glioblastoma patients: a retrospective single-center study. World Neurosurg 114:e121–e128. https://doi.org/10.1016/j.wneu.2018.02.084
McGirt MJ, Mukherjee D, Chaichana KL et al (2009) Association of surgically acquired motor and language deficits on overall survival after resection of glioblastoma multiforme. Neurosurgery 65:463–469. https://doi.org/10.1227/01.NEU.0000349763.42238.E9
Rahman M, Abbatematteo J, De Leo EK et al (2017) The effects of new or worsened postoperative neurological deficits on survival of patients with glioblastoma. J Neurosurg 127:123–131. https://doi.org/10.3171/2016.7.JNS16396
Sanai N, Martino J, Berger MS (2012) Morbidity profile following aggressive resection of parietal lobe gliomas. J Neurosurg 116:1182–1186. https://doi.org/10.3171/2012.2.JNS111228
Altieri R, Raimondo S, Tiddia C et al (2019) Glioma surgery: from preservation of motor skills to conservation of cognitive functions. J Clin Neurosci Off J Neurosurg Soc Australas 70:55–60. https://doi.org/10.1016/j.jocn.2019.08.091
De Witt Hamer PC, Robles SG, Zwinderman AH et al (2012) Impact of intraoperative stimulation brain mapping on glioma surgery outcome: a meta-analysis. J Clin Oncol Off J Am Soc Clin Oncol 30:2559–2565. https://doi.org/10.1200/JCO.2011.38.4818
Sacko O, Lauwers-Cances V, Brauge D, et al (2011) Awake craniotomy vs surgery under general anesthesia for resection of supratentorial lesions. Neurosurgery 68:1192–1198; discussion 1198–1199. https://doi.org/https://doi.org/10.1227/NEU.0b013e31820c02a3
Roca E, Pallud J, Guerrini F et al (2019) Stimulation-related intraoperative seizures during awake surgery: a review of available evidences. Neurosurg Rev. https://doi.org/10.1007/s10143-019-01214-0
Duffau H (2005) Lessons from brain mapping in surgery for low-grade glioma: insights into associations between tumour and brain plasticity. Lancet Neurol 4:476–486. https://doi.org/10.1016/S1474-4422(05)70140-X
Eseonu CI, Rincon-Torroella J, ReFaey K et al (2017) Awake craniotomy vs craniotomy under general anesthesia for perirolandic gliomas: evaluating perioperative complications and extent of resection. Neurosurgery 81:481–489. https://doi.org/10.1093/neuros/nyx023
Kim SS, McCutcheon IE, Suki D et al (2009) Awake craniotomy for brain tumors near eloquent cortex: correlation of intraoperative cortical mapping with neurological outcomes in 309 consecutive patients. Neurosurgery 64:836–845. https://doi.org/10.1227/01.NEU.0000342405.80881.81
Paiva WS, Fonoff ET, Beer-Furlan A et al (2019) Evaluation of postoperative deficits following motor cortex tumor resection using small craniotomy. Surg J N Y N 5:e8–e13. https://doi.org/10.1055/s-0039-1679931
Serletis D, Bernstein M (2007) Prospective study of awake craniotomy used routinely and nonselectively for supratentorial tumors. J Neurosurg 107:1–6. https://doi.org/10.3171/JNS-07/07/0001
Grossman R, Nossek E, Sitt R et al (2013) Outcome of elderly patients undergoing awake-craniotomy for tumor resection. Ann Surg Oncol 20:1722–1728. https://doi.org/10.1245/s10434-012-2748-x
Sanai N, Mirzadeh Z, Berger MS (2008) Functional outcome after language mapping for glioma resection. N Engl J Med 358:18–27. https://doi.org/10.1056/NEJMoa067819
Southwell DG, Riva M, Jordan K et al (2017) Language outcomes after resection of dominant inferior parietal lobule gliomas. J Neurosurg 127:781–789. https://doi.org/10.3171/2016.8.JNS16443
Pallud J, Mandonnet E, Corns R et al (2017) Technical principles of direct bipolar electrostimulation for cortical and subcortical mapping in awake craniotomy. Neurochirurgie 63:158–163. https://doi.org/10.1016/j.neuchi.2016.12.004
Gupta DK, Chandra PS, Ojha BK et al (2007) Awake craniotomy versus surgery under general anesthesia for resection of intrinsic lesions of eloquent cortex–a prospective randomised study. Clin Neurol Neurosurg 109:335–343. https://doi.org/10.1016/j.clineuro.2007.01.008
Tuominen J, Yrjänä S, Ukkonen A, Koivukangas J (2013) Awake craniotomy may further improve neurological outcome of intraoperative MRI-guided brain tumor surgery. Acta Neurochir (Wien) 155:1805–1812. https://doi.org/10.1007/s00701-013-1837-3
Duffau H (2020) Functional mapping before and after low-grade glioma surgery: a new way to decipher various spatiotemporal patterns of individual neuroplastic potential in brain tumor patients. Cancers. https://doi.org/10.3390/cancers12092611
Cargnelutti E, Ius T, Skrap M, Tomasino B (2020) What do we know about pre- and postoperative plasticity in patients with glioma? A review of neuroimaging and intraoperative mapping studies. NeuroImage Clin 28:102435. https://doi.org/10.1016/j.nicl.2020.102435
Gibb WR, Kong NW, Tate MC (2020) Direct evidence of plasticity within human primary motor and somatosensory cortices of patients with glioblastoma. Neural Plast 2020:8893708. https://doi.org/10.1155/2020/8893708
Kim Y-J, Lee DJ, Park C-K, Kim IA (2019) Optimal extent of resection for glioblastoma according to site, extension, and size: a population-based study in the temozolomide era. Neurosurg Rev 42:937–950. https://doi.org/10.1007/s10143-018-01071-3
Stupp R, Hegi ME, Mason WP et al (2009) Effects of radiotherapy with concomitant and adjuvant temozolomide versus radiotherapy alone on survival in glioblastoma in a randomised phase III study: 5-year analysis of the EORTC-NCIC trial. Lancet Oncol 10:459–466. https://doi.org/10.1016/S1470-2045(09)70025-7
Jakola AS, Gulati S, Weber C et al (2011) Postoperative deterioration in health related quality of life as predictor for survival in patients with glioblastoma: a prospective study. PLoS ONE 6:e28592. https://doi.org/10.1371/journal.pone.0028592
Milian M, Tatagiba M, Feigl GC (2014) Patient response to awake craniotomy—a summary overview. Acta Neurochir (Wien) 156:1063–1070. https://doi.org/10.1007/s00701-014-2038-4
Manninen PH, Balki M, Lukitto K, Bernstein M (2006) Patient satisfaction with awake craniotomy for tumor surgery: a comparison of remifentanil and fentanyl in conjunction with propofol. Anesth Analg 102:237–242. https://doi.org/10.1213/01.ANE.0000181287.86811.5C
Whittle IR, Midgley S, Georges H et al (2005) Patient perceptions of “awake” brain tumour surgery. Acta Neurochir (Wien) 147:275–277. https://doi.org/10.1007/s00701-004-0445-7
Nickel K, Renovanz M, König J et al (2018) The patients’ view: impact of the extent of resection, intraoperative imaging, and awake surgery on health-related quality of life in high-grade glioma patients-results of a multicenter cross-sectional study. Neurosurg Rev 41:207–219. https://doi.org/10.1007/s10143-017-0836-x
Gerritsen JKW, Klimek M, Dirven CMF et al (2019) The SAFE-trial: safe surgery for glioblastoma multiforme: awake craniotomy versus surgery under general anesthesia. Study protocol for a multicenter prospective randomized controlled trial. Contemp Clin Trials 88:105876. https://doi.org/10.1016/j.cct.2019.105876
Acknowledgements
We thank the neuroradiologists, neuropathologists, radiation oncologists and medical oncologists who followed the patients. We also thank Gwénaëlle Soulard and Nolwenn Madec for their help in the recovery and exploitation of data and Alex Edelman and Associates for correcting the manuscript.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Clavreul, A., Aubin, G., Delion, M. et al. What effects does awake craniotomy have on functional and survival outcomes for glioblastoma patients?. J Neurooncol 151, 113–121 (2021). https://doi.org/10.1007/s11060-020-03666-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-020-03666-7