Abstract
Background
Though meningioma is the most common primary brain tumor, there is a paucity of epidemiologic studies investigating disparities in treatment and patient outcomes. Therefore, we sought to explore how sociodemographic factors are associated with rates of gross total resection (GTR) and radiotherapy as well as survival.
Methods
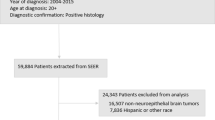
The National Cancer Institute's Surveillance, Epidemiology, and End Results (SEER) database was queried to identify adult patients with meningioma diagnosed between 2005 and 2015. Socioeconomic status (SES) was determined using a validated composite index in which patients were stratified into tertiles and quintiles. Multivariable logistic regression and Cox proportional hazards analyses were used to identify predictors of treatment and survival, respectively.
Results
71,098 patients met our inclusion criteria. Low SES quintile was associated with reduced odds of receiving GTR (OR 0.76, 95% CI 0.69–0.83, p < 0.0001) and radiotherapy (OR 0.83, 95% CI 0.76–0.91, p < 0.0001) as well as worse survival (HR 1.48, 95% CI 1.41–1.56) as compared to the highest SES quintile. Black patients had reduced odds of GTR (OR 0.74, 95% CI 0.67–0.71, p < 0.0001) and worse survival (HR 1.23, 95% CI 1.18–1.29, p < 0.0001) as compared to white patients.
Conclusions
This national study of patients with meningioma found socioeconomic status and race to be independent inverse correlates of likelihood of GTR, radiotherapy, and survival. Limited access to care may underlie these disparities in part, and future studies are warranted to identify specific causes for these findings.

Similar content being viewed by others
References
Ostrom QT, Gittleman H, Xu J et al (2016) CBTRUS statistical report: primary brain and other central nervous system tumors diagnosed in the United States in 2009–2013. Neuro Oncol 18(suppl_5):v1–v75
Buerki RA, Horbinski CM, Kruser T, Horowitz PM, James CD, Lukas RV (2018) An overview of meningiomas. Fut Oncol (London, England) 14(21):2161–2177
Bi WL, Dunn IF (2017) Current and emerging principles in surgery for meningioma. Chin Clin Oncol 6(Suppl 1):S7
Kalamarides M, Stemmer-Rachamimov AO, Niwa-Kawakita M et al (2011) Identification of a progenitor cell of origin capable of generating diverse meningioma histological subtypes. Oncogene 30(20):2333–2344
Apra C, Peyre M, Kalamarides M (2018) Current treatment options for meningioma. Expert Rev Neurother 18(3):241–249
Goldbrunner R, Minniti G, Preusser M et al (2016) EANO guidelines for the diagnosis and treatment of meningiomas. Lancet Oncol 17(9):e383–391
Hwang KL, Hwang WL, Bussiere MR, Shih HA (2017) The role of radiotherapy in the management of high-grade meningiomas. Chin Clin Oncol 6(Suppl 1):S5
Pinzi V, Biagioli E, Roberto A et al (2017) Radiosurgery for intracranial meningiomas: a systematic review and meta-analysis. Crit Rev Oncol/Hematol 113:122–134
Rogers L, Barani I, Chamberlain M et al (2015) Meningiomas: knowledge base, treatment outcomes, and uncertainties. A RANO review. J Neurosurg 122(1):4–23
Sun SQ, Hawasli AH, Huang J, Chicoine MR, Kim AH (2015) An evidence-based treatment algorithm for the management of WHO Grade II and III meningiomas. Neurosurg Focus 38(3):E3
Curry WT Jr, Barker FG 2nd (2009) Racial, ethnic and socioeconomic disparities in the treatment of brain tumors. J Neurooncol 93(1):25–39
Surveillance Epidemiology and End Results program (www.seer.cancer.gov). Database: Census Tract-level SES and Rurality Database (2000–2015)
Yost K, Perkins C, Cohen R, Morris C, Wright W (2001) Socioeconomic status and breast cancer incidence in California for different race/ethnic groups. Cancer Causes Control 12:703–711
Ostrom QT, Gittleman H, Liao P et al (2017) CBTRUS statistical report: Primary brain and other central nervous system tumors diagnosed in the United States in 2010–2014. Neuro Oncol 19(suppl_5):v1–v88
Cahill KS, Claus EB (2011) Treatment and survival of patients with nonmalignant intracranial meningioma: results from the Surveillance, Epidemiology, and End Results Program of the National Cancer Institute Clinical article. J Neurosurg 115(2):259–267
Mukherjee D, Patil CG, Todnem N et al (2013) Racial disparities in Medicaid patients after brain tumor surgery. J Clin Neurosci 20(1):57–61
Wong J, Mendelsohn D, Nyhof-young J, Bernstein M (2011) A qualitative assessment of the supportive care and resource needs of patients undergoing craniotomy for benign brain tumours. Support Care Cancer 19(11):1841–1848
Baba A, McCradden MD, Rabski J, Cusimano MD (2019) Determining the unmet needs of patients with intracranial meningioma—a qualitative assessment. Neuro-Oncol Pract. https://doi.org/10.1093/nop/npz054
Rinehart CD, Yang AI, Fathy R, Hitti FL, Brant J et al (2019) Inequalities in meningioma survival: results from the National Cancer Database. Neurooncol Open Access 4(1):2
Rogers A, Flowers J, Pencheon D (1999) Improving access needs a whole systems approach. BMJ 319:866–867
Basu J, Clancy C (2001) Racial disparity, primary care, and specialty referral. Health Serv Res 36(6 Pt 2):64–77
Bach PB, Pham HH, Schrag D et al (2004) Primary care physicians who treat blacks and whites. N Engl J Med 351:575–584
Greenberg CC, Weeks JC, Stain SC (2008) Disparities in oncologic surgery. World J Surg 32(4):522–528
Tammemagi CM, Nerenz D, Neslund-Dudas C et al (2005) Comorbidity and survival disparities among black and white patients with breast cancer. JAMA 294:1765–1772
Dein S (2004) Explanatory models of and attitudes towards cancer in different cultures. Lancet Oncol 5:119–124
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to report. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Bhambhvani, H.P., Rodrigues, A.J., Medress, Z.A. et al. Racial and socioeconomic correlates of treatment and survival among patients with meningioma: a population-based study. J Neurooncol 147, 495–501 (2020). https://doi.org/10.1007/s11060-020-03455-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-020-03455-2