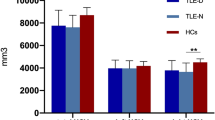
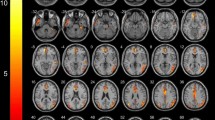
Objectives. To assess the morphological features of brain structures in patients with temporal lobe epilepsy and comorbid depression. Materials and methods. A total of 80 patients with temporal lobe epilepsy (18–60 years old, including 38 with comorbid depression) and 48 healthy subjects of comparable age were examined over the period January 1, 2017 to December 31, 2020. Brain MRI scans were obtained following an epileptic protocol using a 1.5-T scanner. Diagnoses of focal temporal lobe epilepsy were established by neurologists specializing in epilepsy in accordance with the 2017 International League Against Epilepsy classification. The presence and severity of depressive disorder was determined by psychiatrists by clinical interview and Beck Depression Inventory (BDI-II) self-reports. Volumes of subcortical structures and cortical thickness were evaluated by processing MRI data in FreeSurfer 6.0 software. At the group level, analysis of covariance with the Holm–Bonferroni correction was used for statistical analysis. Results. Morphometric analysis revealed significant decreases in the volumes of the brainstem and thalamus bilaterally, along with an increase in the volume of the choroid plexus in the left hemisphere in patients with epilepsy as compared with healthy controls. In addition, patients with epilepsy, as compared with healthy controls, had significantly greater thickness of the entorhinal cortex and the temporal pole and isthmus of the cingulate gyrus in the left hemisphere, while in the right hemisphere patients had significantly lesser thickness of the middle temporal gyrus and inferior temporal gyrus. There was no association between the presence of depression and significant MRI structural changes. Conclusions. These data identify a relationship between temporal lobe epilepsy and the morphology of brain structures, while comorbid depression showed no such link.
Similar content being viewed by others
References
Kanner, A. M., “Depression and epilepsy: a new perspective on two closely related disorders,” Epilepsy Curr., 6, No. 5, 141–146 (2006), https://doi.org/10.1111/j.1535-7511.2006.00125.x.
Baxendale, S. A., Thompson, P. J., and Duncan, J. S., “Epilepsy and depression: the effects of comorbidity on hippocampal volume – a pilot study,” Seizure, 14, No. 6, 435–438 (2005), https://doi.org/10.1016/j.seizure.2005.07.003.
Rider, F. K., Danilenko, O. A., and Grishkina, M. N., et al., “Depression and epilepsy: comorbidities, pathogenesis, principles of therapy,” Zh. Nevrol. Psikhiatr., 116, No. 9, Iss. 2, 19–24 (2016), https://doi.org/10.17116/jnevro20161169219-24.
Mula, M., “Depression in epilepsy,” Curr. Opin. Neurol., 30, No. 2, 180–186 (2017), https://doi.org/10.1097/WCO.0000000000000431.
Mula, M., Kanner, A. M., Jetté, N., and Sander, J. W., “Psychiatric comorbidities in people with epilepsy,” Neurol. Clin. Pract., 11, No. 2, 112–120 (2021), https://doi.org/10.1212/CPJ.0000000000000874.
Zinchuk, M. S., Kustov, G. V., and Pashnin, E. V., et al., “Screening for anxiety and depressive disorders in epilepsy: current state of the art,” Ross. Psikhiat. Zh., 121, No. 3, 87–97 (2021), https://doi.org/10.47877/1560-957X-2021-10309.
Tao, K. and Wang, X., “The comorbidity of epilepsy and depression: diagnosis and treatment,” Expert Rev. Neurother., 16, No. 11, 1321–1333 (2016), https://doi.org/10.1080/14737175.2016.1204233.
Josephson, C. B., Lowerison, M., Vallerand, I., et al., “Association of depression and treated depression with epilepsy and seizure outcomes,” JAMA Neurol., 74, No. 5, 533–539 (2017), https://doi.org/10.1001/jamaneurol.2016.5042.
Hesdorffer, D. C., Lúðvígsson, P., Hauser, W. A., et al., “Co-occurrence of major depression or suicide attempt with migraine with aura and risk for unprovoked seizure,” Epilepsy Res., 75, No. 2–3, 220–223 (2007), https://doi.org/10.1016/j.eplepsyres.2007.05.001.
MacKenzie, G. and Maguire, J., “Chronic stress shifts the GABA reversal potential in the hippocampus and increases seizure susceptibility,” Epilepsy Res., 109, 13–27 (2015), https://doi.org/10.1016/j.eplepsyres.2014.10.003.
Hutton, C., De Vita, E., Ashburner, J., et al., “Voxel-based cortical thickness measurements in MRI,” NeuroImage, 40, No. 4, 1701–1710 (2008), https://doi.org/10.1016/j.neuroimage.2008.01.027.
Bernhardt, B. C., Hong, S. J., Bernasconi, A., and Bernasconi, N., “Imaging structural and functional brain networks in temporal lobe epilepsy,” Front. Hum. Neurosci., 7, 624 (2013), https://doi.org/10.3389/fnhum.2013.00624.
Whelan, C. D., Altmann, A., Botía, J. A., et al., “Structural brain abnormalities in the common epilepsies assessed in a worldwide ENIGMA study,” Brain, 141, No. 2, 391–408 (2018), https://doi.org/10.1093/brain/awx341.
Wilczyńska, K., Simonienko, K., Konarzewska, B., et al., “Morphological changes of the brain in mood disorders,” Psychiatr. Pol., 52, No. 5, 797–805 (2018), https://doi.org/10.12740/PP/89553.
Richardson, E. J., Griffith, H. R., Martin, R. C., et al., “Structural and functional neuroimaging correlates of depression in temporal lobe epilepsy,” Epilepsy Behav., 10, No. 2, 242–249 (2007), https://doi.org/10.1016/j.yebeh.2006.11.013.
Briellmann, R. S., Hopwood, M. J., and Jackson, G. D., “Major depression in temporal lobe epilepsy with hippocampal sclerosis: Clinical and imaging correlates,” J. Neurol. Neurosurg. Psychiatry, 78, No. 11, 1226–1230 (2007), https://doi.org/10.1136/jnnp.2006.104521.
Butler, T., Blackmon, K., McDonald, C. R., et al., “Cortical thickness abnormalities associated with depressive symptoms in temporal lobe epilepsy,” Epilepsy Behav., 23, No. 1, 64–67 (2012), https://doi.org/10.1016/j.yebeh.2011.10.001.
Finegersh, A., Avedissian, C., Shamim, S., et al., “Bilateral hippocampal atrophy in temporal lobe epilepsy: effect of depressive symptoms and febrile seizures,” Epilepsia, 52, No. 4, 689–697 (2011), https://doi.org/10.1111/j.1528-1167.2010.02928.x.
Scheffer, I. E., Berkovic, S., Capovilla, G., et al., “ILAE classification of the epilepsies: Position paper of the ILAE Commission for Classification and Terminology,” Epilepsia, 58, No. 4, 512–521 (2017), https://doi.org/10.1111/epi.13709.
ICD-10: International Statistical Classification of Diseases and Related Health Problems, World Health Organization, 10th revis., https://apps.who.int/iris/handle/10665/42980, acc. April 23, 2023.
Lasa, L., Ayuso-Mateos, J., Vázquez-Barquero, J., et al., “The use of the Beck Depression Inventory to screen for depression in the general population: a preliminary analysis,” J. Affect. Disord., 57, No. 1–3, 261–265 (2000), https://doi.org/10.1016/S0165-0327(99)00088-9.
Avedisova, A. S., Zakharova, K. V., Gaskin, V. V., et al., “Apathetic depression – clinical and neurophysiological analysis,” Nevrol. Vestnik, 4, No. 48, 5–9 (2016), https://doi.org/10.17116/jnevro20171178111-17.
Mayorova, L. A., Samotaeva, I. S., Lebedeva, N. N., et al., “Neuronet restructuring in focal and generalized epilepsy according to resting state fMRI,” Zh. Nevrol. Psikhiat., 117, No. 9, Iss. 2, 4–9 (2017), https://doi.org/10.17116/jnevro2017117924-9.
Fischl, B., “Automatically parcellating the human cerebral cortex,” Cereb. Cortex, 14, No. 1, 11–22 (2004), https://doi.org/10.1093/cercor/bhg087.
Fjell, A. M. and Walhovd, K. B., “Structural brain changes in aging: Courses, causes and cognitive consequences,” Rev. Neurosci., 21, No. 3, 187–222 (2010), https://doi.org/10.1515/REVNEURO.2010.21.3.187.
Fama, R. and Sullivan, E. V., “Thalamic structures and associated cognitive functions: Relations with age and aging,” Neurosci. Biobehav. Rev., 54, 29–37 (2015), https://doi.org/10.1016/j.neubiorev.2015.03.008.
Singh, T. and Goel, R. K., “Epilepsy associated depression: An update on current scenario, suggested mechanisms, and opportunities,” Neurochem. Res., 46, No. 6, 1305–1321 (2021), https://doi.org/10.1007/s11064-021-03274-5.
Elkommos, S. and Mula, M., “A systematic review of neuroimaging studies of depression in adults with epilepsy,” Epilepsy Behav., 115, 107695 (2021), https://doi.org/10.1016/j.yebeh.2020.107695.
Alhusaini, S., Doherty, C. P., Palaniyappan, L., et al., “Asymmetric cortical surface area and morphology changes in mesial temporal lobe epilepsy with hippocampal sclerosis,” Epilepsia, 53, No. 6, 995–1003 (2012), https://doi.org/10.1111/j.1528-1167.2012.03457.x.
Park, K. M., Kim, T. H., Mun, C. W., et al., “Reduction of ipsilateral thalamic volume in temporal lobe epilepsy with hippocampal sclerosis,” J. Clin. Neurosci., 55, 76–81 (2018), https://doi.org/10.1016/j.jocn.2018.06.025.
Cai, L., He, Q., Luo, H., et al., “Is depression in patients with temporal lobe epilepsy related to hippocampal sclerosis? A meta-analysis,” Clin. Neurol. Neurosurg., 225, 107602 (2023), https://doi.org/10.1016/j.clineuro.2023.107602.
Vinti, V., Dell’Isola, G. B., Tascini, G., et al., “Temporal lobe epilepsy and psychiatric comorbidity,” Front. Neurol., 12, 775781 (2021), https://doi.org/10.3389/fneur.2021.775781.
De Figueiredo, N. S. V., Gaça, L. B., Assunção-Leme, I. B., et al., “A pioneering FreeSurfer volumetric study of a series of patients with mesial temporal lobe epilepsy and hippocampal sclerosis with comorbid depression,” Psychiatry Res. Neuroimaging, 311, 111281 (2021), https://doi.org/10.1016/j.pscychresns.2021.111281.
Acciai, F. and Hardy, M., “Depression in later life: A closer look at the gender gap,” Soc. Sci. Res., 68, 163–175 (2017), https://doi.org/10.1016/j.ssresearch.2017.08.003.
Swetlitz, N., “Depression’s problem with men,” AMA J. Ethics, 23, No. 7, 586–589 (2021), https://doi.org/10.1001/amajethics.2021.586.
Gonçalves, E. B., de Oliveira Cardoso, T. A. M., Yasuda, C. L., and Cendes, F., “Depressive disorders in patients with pharmaco-resistant mesial temporal lobe epilepsy,” J. Int. Med. Res., 46, No. 2, 752–760 (2018), https://doi.org/10.1177/0300060517717825.
Salgado, P. C. B., Yasuda, C. L., and Cendes, F., “Neuroimaging changes in mesial temporal lobe epilepsy are magnified in the presence of depression,” Epilepsy Behav., 19, No. 3, 422–427 (2010), https://doi.org/10.1016/j.yebeh.2010.08.012.
Qin, Y., Tong, X., Li, W., et al., “Divergent anatomical correlates and functional network connectivity patterns in temporal lobe epilepsy with and without depression,” Brain Topogr., 34, No. 4, 525–536 (2021), https://doi.org/10.1007/s10548-021-00848-y.
Mueller, S. G., Laxer, K. D., Barakos, J., et al., “Involvement of the thalamocortical network in TLE with and without mesiotemporal sclerosis,” Epilepsia, 51, No. 8, 1436–1445 (2009), https://doi.org/10.1111/j.1528-1167.2009.02413.x.
Shapey, J., Toma, A., and Saeed, S. R., “Physiology of cerebrospinal fluid circulation,” Curr. Opin. Otolaryngol. Head Neck Surg., 27, No. 5, 326-333 (2019), https://doi.org/10.1097/MOO.0000000000000576.
Hubert, V., Chauveau, F., Dumot, C., et al., “Clinical imaging of choroid plexus in health and in brain disorders: A mini-review,” Front. Mol. Neurosci., 12, 34 (2019), https://doi.org/10.3389/fnmol.2019.00034.
Egorova, N., Gottlieb, E., Khlif, M. S., et al., “Choroid plexus volume after stroke,” Int. J. Stroke, 14, No. 9, 923–930 (2019), https://doi.org/10.1177/1747493019851277.
Ricigliano, V. A. G., Morena, E., Colombi, A., et al., “Choroid plexus enlargement in inflammatory multiple sclerosis: 3.0-T MRI and translocator protein PET evaluation,” Radiology, 301, No. 1, 166–177 (2021), https://doi.org/10.1148/radiol.2021204426.
Zhou, Y. F., Huang, J. C., Zhang, P., et al., “Choroid plexus enlargement and allostatic load in schizophrenia,” Schizophr. Bull., 46, No. 3, 722–731 (2020), https://doi.org/10.1093/schbul/sbz100.
Bernasconi, N., Andermann, F., Arnold, D. L., and Bernasconi, A., “Entorhinal cortex MRI assessment in temporal, extratemporal, and idiopathic generalized epilepsy,” Epilepsia, 44, No. 8, 1070–1074 (2003), https://doi.org/10.1046/j.1528-1157.2003.64802.x.
Kuhn, T., Gullett, J. M., Boutzoukas, A. E., et al., “Temporal lobe epilepsy affects spatial organization of entorhinal cortex connectivity,” Epilepsy Behav., 88, 87–95 (2018), https://doi.org/10.1016/j.yebeh.2018.06.038.
Froriep, U. P., Kumar, A., Cosandier-Rimélé, D., et al., “Altered theta coupling between medial entorhinal cortex and dentate gyrus in temporal lobe epilepsy,” Epilepsia, 53, No. 11, 1937–1947 (2012), https://doi.org/10.1111/j.1528-1167.2012.03662.x.
Glauser, T., Santel, D., DelBello, M., et al., “Identifying epilepsy psychiatric comorbidities with machine learning,” Acta Neurol. Scand., 141, No. 5, 388–396 (2020), https://doi.org/10.1111/ane.13216.
Höller, Y., Butz, K. H., Thomschewski, A. C., et al., “Prediction of cognitive decline in temporal lobe epilepsy and mild cognitive impairment by EEG, MRI, and neuropsychology,” Comput. Intell. Neurosci., 2020, 1–16 (2020), https://doi.org/10.1155/2020/8915961.
Author information
Authors and Affiliations
Corresponding author
Additional information
Translated from Zhurnal Nevrologii i Psikhiatrii imeni S. S. Korsakova, Vol. 123, No. 9, pp. 83–89, September, 2023.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ierusalimsky, N.V., Karimova, E.D., Samotaeva, I.S. et al. Structural Changes in the Brain in Patients with Temporal Lobe Epilepsy and Comorbid Depression. Neurosci Behav Physi 54, 228–234 (2024). https://doi.org/10.1007/s11055-024-01589-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11055-024-01589-8