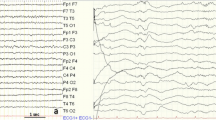
Objectives. To assess the dynamics of the index of epileptiform activity (IEA) as indicator of the efficacy and tolerance of treatment with valproic acid formulations in patients with new diagnoses of generalized and focal epilepsy. Materials and Methods. The study included 93 patients (53 men, 38 women) with focal (n = 27) and idiopathic generalized (n = 66) epilepsy. Patients with idiopathic and age-dependent focal epilepsy were not included in the study. Video EEG monitoring was run at each visit and diffuse and generalized epileptiform activity in waking to sleep, during sleep, after sleep, and during fragmentary waking was evaluated, with assessment of the quantitative IEA, at the beginning of treatment and at 1, 3, 6, and 12 months. Therapeutic drug monitoring was run by titrating drug at one month of treatment or at treatment adjustment. Treatment efficacy was assessed in terms of the absence of seizures and decreases in seizure frequency by more than 50% (responders) and less than 50% (inadequate effect). Adverse events were evaluated on the SIDAED scale. Results. The highest IEA values were seen in both subgroups of patients – with focal and idiopathic generalized epilepsy – before valproic acid treatment initiation. Total IEA in patients with idiopathic generalized epilepsy (52.8 ± 7.8) was significantly greater, while during waking to sleep (3.4 ± 0.8) and during sleep (4.3 ± 0.8) IEA was significantly lower than in patients with focal epilepsy, where the index was 27.1 ± 5.5 (p = 0.027) and 10.5 ± 5.5 (p = 0.003), 8.9 ± 3.7 (p = 0.046), respectively. Valproic acid displayed high efficacy and good tolerance in the treatment of idiopathic generalized and focal epilepsy: by the end of 12 months of observations, remission was obtained in 69 patients (74.2%) and decreases in seizures by more than 50% were seen in 22 patients (23.7%); inadequate effects were obtained in only two subjects (2.1%). Adverse events were recorded in a few cases. Conclusions. Valproic acid remains one of the drugs of choice for the treatment of idiopathic generalized and focal epilepsy. IEA may provide an additional objective criterion in difficult cases to discriminate idiopathic generalized from focal epilepsy in terms of total IEA, IEA before sleep, IEA during sleep, and IEA during fragmentary waking in the first months of treatment (1–3 months), objectively reflecting the dynamics of valproic acid treatment efficacy,
Similar content being viewed by others
References
V. A. Karlov, Epilepsy in Children and Adults, Women and Men. Guidelines for Doctors, Binom, Moscow (2019).
V. A. Karlov, “Depakin: 25 years in Russia,” Zh. Nevrol. Psikhiatr., 117, No. 11, 129–134 (2017).
K. Yu. Mukhin, L. Yu. Glukhova, and M. Yu. Bobylova, Epileptic Syndromes. Diagnosis and Treatment, Moscow (2018), 4th ed.
P. N. Vlasov,” Algorithms for the use of valproic acid formulations in women,” Zh. Nevrol. Psikhiatr., 115, No. 4, 36–40 (2015).
O. L. Badalyan, S. G. Burd, A. A. Savenkov, et al., “Comparative assessment of the efficacy and safety of valproic acid: experience of use,” Epileps. Paroks. Sost., 6, No. 2, 39–44 (2014).
I. Khachidze, M. Gugushvili, M. Makashvili, and V. Maloletnev, “The investigation of EEG specificity in epileptic children during Depakine therapy,” Int. J. Neurosci., 126, No. 10, 912–921 (2016), https://doi.org/10.3109/00207454.2015.1083991.
R. E. Appleton, A. Freeman, and J. H. Cross, “Diagnosis and management of the epilepsies in children: a summary of the partial update of the 2012 NICE epilepsy guideline,” Arch. Dis. Child., 97, No. 12, 1073–1076 (2012), https://doi.org/10.1136/archdischild-2012-302822.
E. Beghi and J. W. Sander, “The ILAE classification of seizures and epilepsies: implications for the clinic,” Expert Rev. Neurother., 18, No. 3, 179–183 (2018), https://doi.org/10.1080/14737175.2018.1427066.
T. A. Glauser and T. Loddenkemper, “Management of childhood epilepsy,” Continuum (Minneap. Minn.), 19, No. 3 Epilepsy, 656–681 (2013), https://doi.org/10.1212/01.CON.0000431381.29308.85.
M. M. Zhu, H. L. Li, L. H. Shi, et al., “The pharmacogenomics of valproic acid,” J. Hum. Genet., 62, No. 12, 1009–1014 (2017), https://doi.org/10.1038/jhg.2017.91.
V. A. Karlov, “Worldwide day of epilepsy patients,” Epileps. Paroks. Sost., 7, No. 1, 56 (2015).
P. N. Vlasov, N. V. Orekhova, M. V. Antonyuk, et al., “Efficacy and safety of valproic acid formulations with controlled release of active ingredient in adults in real clinical practice from the point of view of pharmacokinetic and pharmacogenetic approaches,” Nevrol. Neiropsikh. Psikhosom., 1, 11–20 (2017).
T. Tomson, D. Battino, and E. Perucca, “Valproic acid after five decades of use in epilepsy: time to reconsider the indications of a timehonoured drug,” Lancet Neurol., 15, No. 2, 210–218 (2016), https://doi.org/10.1016/S1474-4422(15)00314-2.
L. R. Zenkov, Clinical Electroencephalography (with elements of epileptology). Guidelines for Doctors, MIA, Moscow (2011), 3rd ed.
B. Clemens, A. Menes, P. Piros, et al., “Quantitative EEG effects of carbamazepine, oxcarbazepine, valproate, lamotrigine, and possible clinical relevance of the findings,” Epilepsy Res., 70, 190–199 (2006), https://doi.org/10.1016/j.eplepsyres.2006.05.003.
M. C. Salinsky, B. S. Oken, D. Storzbach, and C. B. Dodrill, “Assessment of CNS effects of antiepileptic drugs by using quantitative EEG measures,” Epilepsia, 44, 1042–1050 (2003), https://doi.org/10.1046/j.1528-1157.2003.60602.x.
D. Schmidt and W. Löscher, “Uncontrolled epilepsy following discontinuation of antiepileptic drug in seizure-free patients: a review of current clinical experience,” Acta Neurol. Scand., 111, 291–300 (2005), https://doi.org/10.1111/j.1600-0404.2005.00408.x.
E. Yu. Pasternak, R. N. Alyautdin, I. L. Asetskaya, and B. K. Romanov, “The challenge of the interchangeability of antiepileptic drugs: efficacy and safety of valproates,” Nevrol. Zh., 5, 34–39 (2015).
R. S. Fisher, “An overview of the 2017 ILAE operational classification of seizure types,” Epilepsy Behav., 70, Part A, 271–273 (2017), https://doi.org/10.1016/j.yebeh.2017.03.022.
S. G. Uijl, C. S. Uiterwaal, A. P. Aldenkamp, et al., “A cross-sectional study of subjective complaints in patients with epilepsy who seem to be well-controlled with anti-epileptic drugs,” Seizure, 15, No. 4, 242–248 (2006), https://doi.org/10.1016/j.seizure.2006.02.009.
S. J. Nevitt, M. Sudell, J. Weston, et al., “Antiepileptic drug monotherapy for epilepsy: a network meta-analysis of individual participant data,” Cochrane Database Syst. Rev., 12, CD011412 (2017), https://doi.org/10.1002/14651858.cd011412.pub2.
V. A. Karlov, P. N. Vlasov, and A. O. Khabibov, “Depakin 300 and Depakin-Chrono in epilepsy therapy,” Zh. Nevrol. Psikhiatr., 10, 20–25 (1999).
E. D. Belousova, “A Russian observational study of the efficacy and tolerability of Depakin Chrono as first-line monotherapy for focal epilepsy,” Nevrol. Neiropsikh. Psikhosom., 3, 47–52 (2010).
J. Jedrzejczak, M. Kuncikova, S. Magureanu, and the VIPe Study Group, “An observational study of first-line valproate monotherapy in focal epilepsy,” Eur. J. Neurol., 15, 66–72 (2008), https://doi.org/10.1111/j.1468-1331.2007.02003.x.
D. H. Huang, J. O. Zheng, J. Chen, and L. Yu, “Treatment gaps of epilepsy and retention rates of sodium valproate in rural Guangxi, China,” Genet. Mol. Res., 13, No. 3, 6202–6312 (2014), https://doi.org/10.4238/2014.august.15.3.
J. Sala-Padró, M. Toledo, E. Santamarina, et al., “Levetiracetam and valproate retention rate in juvenile myoclonic epilepsy,” Clin. Neuropharmacol., 39, No. 6, 299–301 (2016), https://doi.org/10.1097/wnf.0000000000000177.
D. Deleu, H. Al-Hail, B. Mesraoua, et al., “Short-term efficacy and safety of valproate sustained-release formulation in newly diagnosed partial epilepsy VIPe-study. A multicenter observational open-label study,” Saudi Med. J., 28, No. 9, 1402–1407 (2007), https://doi.org/10.1111/j.1468-1331.2008.02162.x.
A. Kutschenko, M. A. Nitsche, M. Sommer, et al., “Seizure aggravation by valproate in primary generalized epilepsy,” Nervenarzt, 82, No. 2, 226, 228–229 (2011), https://doi.org/10.1007/s00115-010-3080-y.
T. W. May, “Assessment of adverse effects of antiepileptic drugs: The patient’s view,” Epileptology, 1, 46–54 (2013), https://doi.org/10.1016/j.epilep.2013.01.003.
J. A. Urigüen, B. García-Zapirain, J. Artieda, et al., “Comparison of background EEG activity of different groups of patients with idiopathic epilepsy using Shannon spectral entropy and cluster-based permutation statistical testing,” PLoS One, 12, No. 9, e0184044 (2017), https://doi.org/10.1371/journal.pone.0184044.
Author information
Authors and Affiliations
Corresponding author
Additional information
Translated from Zhurnal Nevrologii i Psikhiatrii imeni S. S. Korsakova, Vol. 120, No. 7, Iss. 1, pp. 35–43, July, 2020.
Rights and permissions
About this article
Cite this article
Karlov, V.A., Kozhokaru, A.B., Vlasov, P.N. et al. Dynamics of Epileptiform Activity and the Efficacy and Tolerance of Valproic Acid Formulations in Adolescents and Adults with Newly Diagnosed Epilepsy. Neurosci Behav Physi 51, 289–297 (2021). https://doi.org/10.1007/s11055-021-01070-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11055-021-01070-w