Abstract
Background
Aspergillus species are important causes of invasive fungal disease, particularly among those with an impaired immune system. Increasing reports have revealed a rising incidence of antifungal drug resistance among Aspergillus spp., particularly among cryptic species. Understanding local antifungal susceptibility patterns is paramount to delivering optimal clinical care.
Methods
Aspergillus spp. recovered from clinical specimens between 2000 and 2021 from Pathology Queensland were collected. Aspergillus spp. were identified routinely morphologically, and where there was ambiguity or a lack of sporulation, by sequencing of the internal transcribed spacer (ITS) region. All Aspergillus spp. that underwent antifungal susceptibility testing according to the CLSI M38-A3 method and were recorded and included in the study. Amphotericin B, voriconazole, posaconazole, isavuconazole, micafungin, caspofungin, and anidulafungin were tested. Pathology Queensland services all public healthcare facilities in Queensland, Australia.
Results
236 Aspergillus spp. were identified from clinical specimens during the study period. The most frequent species identified were Aspergillus section Fumigati (n = 119), Aspergillus section Flavi (n = 35), Aspergillus terreus (n = 32) and Aspergillus niger (n = 29). Overall, MIC50/90 values for voriconazole, posaconazole, itraconazole, and isavuconazole were 0.25/1, 0.25/0.5, 0.25/0.5, and 0.5/2 mg/L respectively. Echinocandins demonstrated low MIC values overall with micafungin and anidulafungin both having an MIC50/90 of 0.015/0.03 mg/L. A total of 15 cryptic species were identified; high triazole MIC values were observed with a voriconazole MIC50/90 of 2/8 mg/L. From 2017 to 2021 we observed an increase in incidence of isolates with high voriconazole MIC values. There was no difference in voriconazole MIC values between Aspergillus spp. acquired in North Queensland when compared to Southeast Queensland, Australia.
Conclusion
Increasing reports of antifungal resistance among Aspergillus spp. is concerning and warrants further investigation both locally and worldwide. Active surveillance of both the emergence of different Aspergillus spp. and changes in antifungal susceptibility patterns over time is crucial to informing clinicians and treatment guidelines.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Invasive aspergillosis (IA) is associated with increased mortality in immunocompromised persons. Patients with acute leukaemia and allogeneic stem cell transplantation comprise the largest risk group, with mortality rates reaching 45% in this population [1]. There has been a steady increase in the incidence of IA (i.e., 4.4% per year per 100,000 persons) over the years, particularly among those with haematological malignancies, solid organ transplant recipients, patients with solid tumours, or chronic renal failure [2].
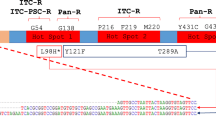
Azole antifungals are the mainstay of treatment and prophylaxis of IA and have been widely used for these indications [3, 4]. In accordance with widespread clinical and environmental azole use, azole resistant Aspergillus spp. are increasingly reported worldwide, both for the azole-naïve and azole-experienced populations, with a prevalence of 3–4% in Aspergillus section Fumigati isolates [5,6,7,8]. Mortality rates can surpass 80% for infections due to azole-resistant Aspergillus spp. [9]. International guidelines recommend against azole monotherapy for detected azole resistance and for the settings where Aspergillus spp. azole resistance exceeds 10%; less favourable therapeutic recommendations such as amphotericin monotherapy or echinocandin plus azole combination therapy have been proposed [3, 4, 10]. Implementation of this approach for the management of acute IA requires close surveillance of antifungal resistance at a local, regional, and global level. This is hampered by the lack of availability of routine antifungal susceptibility testing (AFST) in most clinical microbiology laboratories due to the challenges associated with AFST [11].
In addition, recently there has been an emergence of cryptic Aspergillus species as a cause of invasive disease. These species are difficult to differentiate from other related species by phenotypic and morphologic features alone. Molecular methods for accurate identification have been developed which include targeted sequencing of genetic markers including the internal transcribed spacer (ITS) regions of the rRNA, a portion of the beta-tubulin gene (BenA), a fragment of the calmodulin gene (CaM), and part of the RNA polymerase II second largest subunit gene (RPB2)[12]. Whole genome sequencing (WGS) approaches have also been used for precise species identification [13].
Queensland Health provides a range of serves including haematopoietic stem cell and solid organ transplantation, haematology, medical oncology, intensive care, major surgical sub-specialties, and burns. Queensland is a large state with diverse geography that includes subtropical and tropical coastal regions and inland dry desert areas. Approximately two thirds of the population are concentrated around the Greater Brisbane, Gold Coast, and Sunshine Coast areas in the Southeast corner of the state. For the purposes of this study, we defined North Queensland as a latitude including and above 23.4300° S (Rockhampton Region), and Southeast Queensland as locations below this latitude.
In this study, we aim to characterize Aspergillus spp. causing invasive fungal disease in Queensland, Australia, over a 20-year period. This includes the description of the antifungal resistance profile, with an emphasis on azole resistance, thereby demonstrating antifungal resistance trends over time. We will also determine the effect of geography (e.g. tropical and subtropical climate) on antifungal resistance patterns.
Methods
Aspergillus spp. recovered from clinical specimens between 2000 and 2021 from Pathology Queensland Laboratories were identified. Isolates recovered from sterile material and not deemed a contaminant are always sent for susceptibility testing. Other isolates typically require host factors (e.g. haematological malignancy) and/or clinical features (e.g. dense, well circumscribed lesions on computed tomography [CT] chest) to be noted by the Clinical Microbiologist, after consultation with the treating clinician, in order to justify susceptibility testing. Clinical specimen type included tissue (n = 81), bronchoalveolar lavage fluid (n = 65), upper respiratory tract specimens (n = 47), intra-operative or deep swab (n = 26), and sterile site fluid (n = 17). These samples were set up for fungal culture using a Sabouraud Dextrose Agar (SDA) supplemented with chloramphenicol and gentamicin, which was incubated at 28 degrees Celsius in air for four weeks. Aspergillus spp. were initially identified using phenotypic and morphologic methods, which included growth at different temperatures and morphological characteristics on lactophenol cotton blue staining. From 2011, any isolate thought to be clinically significant (as determined by the clinical microbiologist), and that required identification (e.g. failure to sporulate) or AFST, would undergo Sanger sequencing of the ITS region at a reference laboratory. Prior to 2011, the laboratory relied solely on phenotypic and morphologic methods for identification of moulds. Briefly, fungal DNA was extracted using the QIAGEN DNease® UltraClean® Microbial Kit with the addition of Lyticase to the PowerBead tube containing PowerBead and SL solution. Amplicon sequence was undertaken using a 579 base pair fragment of the ITS using the primary pairs P-ITS-1 and P-ITS-4. Analysis using BLASTNR, MycoBank and MycologyLab were utilised.
All Aspergillus spp. that underwent AFST were recorded and included in the study. Pathology Queensland does not perform AFST on mould isolates, which are sent to the Australian Mycology Reference Laboratory in Adelaide, South Australia for AFST on a case-by-case basis. Australian laboratories that perform AFST rely on commercial methods; as such, the Sensititre YeastOne (ThermoFisher) was used for Aspergillus spp. susceptibility testing [14]. Inoculum suspensions of Aspergillus spp. were prepared according to the CLSI M38-A3 document and A. flavus ATCC 204,304 and A. fumigatus ATCC MYA-3626 were used as CLSI reference strains. Amphotericin B (range, 0.12 to 8 mg/L), voriconazole (range, 0.008 to 8 mg/L), posaconazole (range, 0.008 to 8 mg/L), isavuconazole (range, 0.008 to 8 mg/L), micafungin (range, 0.008 to 8 mg/L), caspofungin (range, 0.008 to 8 mg/L), and anidulafungin (range, 0.015 to 8 mg/L) were tested and recorded. CLSI interpretive criteria were used for susceptibility categorization into wild-type and non-wild-type isolates (CLSI M59 document).
Results
Overall, 236 Aspergillus spp. isolates identified from clinical specimens in patients with suspected invasive Aspergillus spp. infection underwent susceptibility testing (Table 1). The most frequent species identified were Aspergillus section Fumigati (n = 119), Aspergillus section Flavi (n = 36), Aspergillus terreus (n = 32), and Aspergillus niger (n = 29). Other uncommon species identified (n = 20) included A. nidulans, A. calidoustus, A. sydowii, A. ochraceus, A. viridinutans, A. insuetus, A. unguis, A. ustus, A. wisconsinensis, and A. lentulus,. These isolates were identified using molecular techniques. For pooled Aspergillus spp., MIC50/90 values for voriconazole, posaconazole, itraconazole, and isavuconazole were 0.25/1, 0.25/0.5, 0.25/0.5, and 0.5/2 mg/L respectively. Azole antifungals tested against Aspergillus section Fumigati demonstrated favourable in vitro activity overall, with voriconazole and itraconazole having wild-type rates of 95% and 99%, respectively.
Echinocandins demonstrated low MIC values overall, with micafungin and anidulafungin both having an MIC50/90 of 0.015/0.03 mg/L on pooled Aspergillus spp.. Amphotericin B displayed intermediate activity against Aspergillus section Fumigati with approximately half of the isolates having an MIC ≥ 2 mg/L. A total of 15 cryptic species underwent susceptibility testing (Table 2). High triazole MIC values were observed among cryptic species with a voriconazole MIC50/90 of 2/8 mg/L.
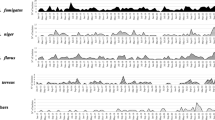
Voriconazole and anidulafungin MIC values of isolates obtained between 2017 and 2021 (n = 150) were analysed according to year (Figs. 1 and 2). In 2021, there were a total of 6 isolates (13%) with a voriconazole MIC value of ≥ 2 mg/L; this compared to a total of 3 (8%), 2 (8%), 2 (10%), and 1 (6%) identified in 2020, 2019, 2018 and 2017, respectively. Anidulafungin MIC values did not appear to change during this 5-year period with > 95% of isolates obtained between 2017 and 2021 having an MIC value between 0.03 and 0.06 mg/L. Thirty-seven isolates (15.7%) came from North Queensland; MIC distribution was not different between North and Southeast Queensland isolates (Fig. 3).
Discussion
Here we describe the speciation and antifungal resistance profiles of 236 Aspergillus spp. causing invasive fungal disease in Queensland, Australia; analyses incorporating the year collected, geographic location, antifungal, and species (inc. cryptic) were undertaken. Aspergillus spp. identified, followed a similar frequency distribution to other datasets with the most frequently encountered species being Aspergillus section Fumigati [15]. More cryptic Aspergillus spp. were identified (n = 15, 6.4%) later in the study period, most likely contributed by the incorporation and increased use of molecular identification techniques. It is estimated that between 3 and 15% of IA infections are caused by cryptic species [16, 17]. Correct identification is paramount as some of the cryptic species, particularly A. lentulus, A. alliaceus, A. sydowii, A. calidoustus, A. keveii, A. insuetus, and A. fumigatiaffinis, demonstrate resistance to both azole and polyene antifungals [18, 19] as was demonstrated in this study where many cryptic isolates exhibited a voriconazole MIC between 4 and 8 mg/L.
Overall, our isolates displayed similar MIC values to those presented in other regions, both locally and worldwide [20] [21]. We noted that recovery of Aspergillus spp. with high voriconazole MIC values occurred more frequently later during the study period. Although, there was an overall increase in isolates being sent for AFST during this time. This is similar to the global trend of rising azole resistance [21,22,23,24,25,26,27,28,29,30,31,32,33,34]. A Dutch survey of unselected clinical Aspergillus section Fumigati isolates demonstrated an increase in resistance from 7% in 2014 to 15% in 2017 [35]. This is of particular concern given that azole resistance is associated with treatment failure [36,37,38].
Triazole resistance among clinically significant Aspergillus spp. is much higher in other regions around the world. A study from Turkey documented a 10.2% itraconazole resistance rate when they investigated 746 isolates collected from 1999 to 2012[24]. A similar study conducted in Japan noted the prevalence of azole-resistance Aspergillus spp. to be 8.3%[39]. A study which observed resistance rates among Latin American and African isolates noted triazole-resistance in 6.9% of samples in Mexico, 8.3% in Paraguay, 9.8% in Peru, and 2.2% in Nigeria [40].
There was no difference in voriconazole MIC values between Aspergillus spp. acquired in North Queensland when compared to Southeast Queensland, Australia, although the numbers from North Queensland were small. Climate and temperature change has been posed as a contributor to the emergence of different fungal pathogens and worsening antifungal resistance [41]. In addition, agricultural fungicides are also a known contributor to azole resistance among Aspergillus spp. Queensland is a large state with variations in climate and agriculture depending on the region. This gives added importance to the surveillance of antifungal resistance patterns over time across the whole state.
There are several limitations to this study which need to be outlined. Firstly, isolates included were obtained from public laboratories only and were from individuals with a high likelihood of invasive fungal disease. True epidemiological surveillance would incorporate testing of all Aspergillus spp. isolates from all laboratories and include those obtained from the environment. Secondly, there were no strict rules or criteria enforced with regards to triggering susceptibility testing of isolates. Clinical interpretation and decision making by the clinical microbiologist occurred. Thirdly, not all isolates were identified using molecular methods. In addition, amplicon sequencing targeting the ITS region was used for molecular identification which may misidentify some species of Aspergillus when used alone. Sequencing a portion of the beta-tubulin (BenA) and calmodulin (CaM) genes has been recommended for more high-resolution speciation [42]. Fourthly, there were changes to the methodology of antifungal susceptibility testing during the study period, including the antifungals tested. Our isolates were all tested at the same reference laboratory which prevented interlaboratory variability in results.
Conclusion
IA carries a significant burden of disease globally, particularly among individuals with impaired immunity. Increasing reports of antifungal resistance among Aspergillus spp. is concerning and warrants further investigation both locally and worldwide. Reliable resistance data in Aspergillus spp. is difficult to obtain given that susceptibility testing is generally not a part of international antimicrobial resistance programs. Moreover, in Australia there is limited data on antifungal susceptibility patterns amongst clinically relevant mould species. Active surveillance of both the emergence of Aspergillus spp. and changes in antifungal susceptibility patterns over time is crucial to informing clinicians and treatment guidelines. Understanding the effects of the varied environmental pressures in different parts of Australia on clinically important Aspergillus spp. is also paramount.
References
Lortholary O, et al. Epidemiological trends in invasive aspergillosis in France: the SAIF network (2005–2007). Clin Microbiol Infect. 2011;17(12):1882–9.
Bitar D, et al. Population-based analysis of invasive fungal infections, France, 2001–2010. Emerg Infect Dis. 2014;20(7):1149–55.
Patterson TF, et al. Practice guidelines for the diagnosis and management of Aspergillosis: 2016 update by the infectious diseases society of America. Clin Infect Dis. 2016;63(4):e1–60.
Ullmann AJ, et al. Diagnosis and management of Aspergillus diseases: executive summary of the 2017 ESCMID-ECMM-ERS guideline. Clin Microbiol Infect. 2018;24(Suppl 1):e1–38.
Van Der Linden JW, Warris A, Verweij PE. Aspergillus species intrinsically resistant to antifungal agents. Med Mycol. 2011;49(Suppl 1):S82–9.
Camps SMT, et al. Rapid induction of multiple resistance mechanisms in Aspergillus fumigatus during azole therapy: a case study and review of the literature. Antimicrob Agents Chemother. 2012;56(1):10–6.
Wu CJ, et al. Multicenter study of azole-resistant Aspergillus fumigatus clinical isolates, Taiwan. Emerg Infect Dis. 2020;26(4):804–6.
van der Linden JW, et al. Prospective multicenter international surveillance of azole resistance in Aspergillus fumigatus. Emerg Infect Dis. 2015;21(6):1041–4.
van der Linden JW, et al. Clinical implications of azole resistance in Aspergillus fumigatus, The Netherlands, 2007–2009. Emerg Infect Dis. 2011;17(10):1846–54.
Verweij PE, et al. International expert opinion on the management of infection caused by azole-resistant Aspergillus fumigatus. Drug Resist Updat. 2015;21–22:30–40.
Durand C, et al. Can we improve antifungal susceptibility testing? Front Cell Infect Microbiol. 2021;11:720609.
Siqueira JPZ, et al. Cryptic Aspergillus from clinical samples in the USA and description of a new species in section Flavipedes. Mycoses. 2018;61(11):814–25.
Kjærbølling I, et al. A comparative genomics study of 23 Aspergillus species from section Flavi. Nat Commun. 2020;11(1):1106.
Halliday CL, et al. Evaluation of a custom Sensititre YeastOne plate for susceptibility testing of isavuconazole and other antifungals against clinically relevant yeast and mould species in three Australian diagnostic mycology laboratories. Pathology. 2022;54(7):922–7.
Morris AJ, et al. Antifungal susceptibility of clinical mould isolates in New Zealand, 2001–2019. Pathology. 2021;53(5):639–44.
Lamoth F. Aspergillus fumigatus-related species in clinical practice. Front Microbiol. 2016;7:683.
Balajee SA, et al. Molecular identification of Aspergillus species collected for the transplant-associated infection surveillance network. J Clin Microbiol. 2009;47(10):3138–41.
Nematollahi S, et al. Aspergillus lentulus: an under-recognized cause of antifungal drug-resistant Aspergillosis. Open Forum Infect Dis. 2021;8(8):ofab392.
Alastruey-Izquierdo A, et al. Population-based survey of filamentous fungi and antifungal resistance in Spain (FILPOP Study). Antimicrob Agents Chemother. 2013;57(7):3380–7.
Pfaller MA, et al. In vitro activities of isavuconazole and comparator antifungal agents tested against a global collection of opportunistic yeasts and molds. J Clin Microbiol. 2013;51(8):2608–16.
Kidd SE, et al. Multi-triazole-resistant Aspergillus fumigatus infections in Australia. Mycoses. 2015;58(6):350–5.
Bader O, et al. Environmental isolates of azole-resistant Aspergillus fumigatus in Germany. Antimicrob Agents Chemother. 2015;59(7):4356–9.
Sharma C, et al. Triazole-resistant Aspergillus fumigatus harbouring G54 mutation: is it de novo or environmentally acquired? J Glob Antimicrob Resist. 2015;3(2):69–74.
Ozmerdiven GE, et al. First determination of azole resistance in Aspergillus fumigatus strains carrying the TR34/L98H mutations in Turkey. J Infect Chemother. 2015;21(8):581–6.
Vermeulen E, et al. Nationwide surveillance of azole resistance in Aspergillus diseases. Antimicrob Agents Chemother. 2015;59(8):4569–76.
Pelaez T, et al. First detection of Aspergillus fumigatus azole-resistant strain due to Cyp51A TR46/Y121F/T289A in an azole-naive patient in Spain. New Microbes New Infect. 2015;6:33–4.
Chowdhary A, et al. Prevalence and mechanism of triazole resistance in Aspergillus fumigatus in a referral chest hospital in Delhi, India and an update of the situation in Asia. Front Microbiol. 2015;6:428.
Lavergne RA, et al. First description of azole-resistant Aspergillus fumigatus due to TR46/Y121F/T289A mutation in France. Antimicrob Agents Chemother. 2015;59(7):4331–5.
Chowdhary A, et al. Multi-azole-resistant Aspergillus fumigatus in the environment in Tanzania. J Antimicrob Chemother. 2014;69(11):2979–83.
Astvad KM, et al. First detection of TR46/Y121F/T289A and TR34/L98H alterations in Aspergillus fumigatus isolates from azole-naive patients in Denmark despite negative findings in the environment. Antimicrob Agents Chemother. 2014;58(9):5096–101.
Lockhart SR, et al. Azole resistance in Aspergillus fumigatus isolates from the ARTEMIS global surveillance study is primarily due to the TR/L98H mutation in the cyp51A gene. Antimicrob Agents Chemother. 2011;55(9):4465–8.
Howard SJ, et al. Frequency and evolution of Azole resistance in Aspergillus fumigatus associated with treatment failure. Emerg Infect Dis. 2009;15(7):1068–76.
Wu CJ, et al. Azole-resistant Aspergillus fumigatus isolates carrying TR(3)(4)/L98H mutations in Taiwan. Mycoses. 2015;58(9):544–9.
Ahmad S, et al. Concomitant occurrence of itraconazole-resistant and -susceptible strains of Aspergillus fumigatus in routine cultures. J Antimicrob Chemother. 2015;70(2):412–5.
SC, D.G. and M. JW, NethMap 2018: Consumption of antimicrobial agents and antimicrobial resistance among medically important bacteria in the Netherlands/MARAN 2018: Monitoring of Antimicrobial Resistance and Antibiotic Usage in Animals in the Netherlands in 2017. 2018, Rijksinstituut voor Volksgezondheid en Milieu RIVM
Verweij PE, Mellado E, Melchers WJ. Multiple-triazole-resistant Aspergillosis. N Engl J Med. 2007;356(14):1481–3.
van der Linden JW, et al. Aspergillosis due to voriconazole highly resistant Aspergillus fumigatus and recovery of genetically related resistant isolates from domiciles. Clin Infect Dis. 2013;57(4):513–20.
Snelders E, et al. Emergence of azole resistance in Aspergillus fumigatus and spread of a single resistance mechanism. PLoS Med. 2008;5(11): e219.
Takeda K, et al. High detection rate of azole-resistant Aspergillus fumigatus after treatment with azole antifungal drugs among patients with chronic pulmonary Aspergillosis in a single hospital setting with low azole resistance. Med Mycol. 2021;59(4):327–34.
Resendiz-Sharpe A, et al. Triazole-resistance in environmental Aspergillus fumigatus in Latin American and African Countries. J Fungi (Basel). 2021;7(4):292.
Revie NM, et al. Antifungal drug resistance: evolution, mechanisms and impact. Curr Opin Microbiol. 2018;45:70–6.
Tam EW, et al. Misidentification of Aspergillus nomius and Aspergillus tamarii as Aspergillus flavus: characterization by internal transcribed spacer, β-Tubulin, and calmodulin gene sequencing, metabolic fingerprinting, and matrix-assisted laser desorption ionization-time of flight mass spectrometry. J Clin Microbiol. 2014;52(4):1153–60.
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions. The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Adam G Stewart and Claire Heney. The first draft of the manuscript was written by Adam G Stewart and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interest to disclose.
Ethics approval
This is a laboratory-based study. The RBWH Human Research Ethics Committee has confirmed that no ethical approval is required.
Additional information
Handling Editor: Vishukumar Aimanianda.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Stewart, A.G., Isler, B., Simos, P. et al. Aspergillus Species Causing Invasive Fungal Disease in Queensland, Australia. Mycopathologia 188, 211–219 (2023). https://doi.org/10.1007/s11046-023-00713-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11046-023-00713-5