Abstract
Background
Glutathione is a tripeptide detoxifying a variety of exogenous and endogenous free radicals and carcinogens, and a deficiency of glutathione is associated with an increased host susceptibility to oxidative stress, a pathological condition implicated in the development and progression of cancer. The catalytic subunit of glutamate-cysteine ligase (GCLC) is an enzyme responsible for the initial and rate-limiting step of glutathione biosynthesis.
Methods and results
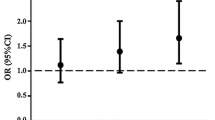
The aim of this pilot study was to investigate whether genetic variation at the GCLC gene contributes to the risk of colorectal cancer (CRC). DNA samples from 681 unrelated Russian individuals (283 patients with CRC and 398 age- and sex-matched healthy controls) were genotyped for six common functional SNPs of the GCLC gene (SNPs) such as rs12524494, rs17883901, rs606548, rs636933, rs648595 and rs761142 of the GCLC gene using the MassARRAY-4 system. We found that genotype rs606548-C/T is significantly associated with increased risk of CRC regardless of sex and age (OR 2.24; 95% CI 1.24–4.03; P = 0.007, FDR = 0.04). Moreover, ten GCLC genotype combinations showed association with the risk of CRC (P < 0.05). Functional SNP annotation enabled establishing the CRC-associated polymorphisms are associated with a decreased GCLC expression that may be attributed to epigenetic effects of histone modifications operating in a colon-specific manner.
Conclusions
The present study was the first to show that genetic variation at the catalytic subunit of glutamate-cysteine ligase may contribute to the risk of colorectal cancer risk. However, further genetic association studies with a larger sample size are required to substantiate the role of GCLC gene polymorphisms in the development of sporadic colorectal cancer.
Similar content being viewed by others
References
Ferlay J, Soerjomataram I, Dikshit R et al (2015) Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer 136(5):E359–E386. https://doi.org/10.1002/ijc.29210
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F (2021) Global Cancer Statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 71(3):209–249. https://doi.org/10.3322/caac.21660
Ferlay J, Colombet M, Soerjomataram I, Parkin DM, Piñeros M, Znaor A, Bray F (2020) Cancer statistics for the year 2020: an overview. Int J Cancer. https://doi.org/10.1002/ijc.33588
Keum N, Giovannucci E (2019) Global burden of colorectal cancer: emerging trends, risk factors and prevention strategies. Nat Rev Gastroenterol Hepatol 16(12):713–732. https://doi.org/10.1038/s41575-019-0189-8
Aran V, Victorino AP, Thuler LC, Ferreira CG (2016) Colorectal cancer: epidemiology, disease mechanisms and interventions to reduce onset and mortality. Clin Colorectal Cancer 15(3):195–203. https://doi.org/10.1016/j.clcc.2016.02.008
Wan ML, Wang Y, Zeng Z, Deng B, Zhu BS, Cao T, Li YK, Xiao J, Han Q, Wu Q (2020) Colorectal cancer (CRC) as a multifactorial disease and its causal correlations with multiple signaling pathways. Biosci Rep 40(3):BSR2020065
Azarova I, Klyosova E, Lazarenko V, Konoplya A, Polonikov A (2020) Genetic variants in glutamate cysteine ligase confer protection against type 2 diabetes. Mol Biol Rep 47(8):5793–5805. https://doi.org/10.1007/s11033-020-05647-5
Fearon ER (2011) Molecular genetics of colorectal cancer. Annu Rev Pathol 6:479–507. https://doi.org/10.1146/annurev-pathol-011110-130235
Siegert S, Hampe J, Schafmayer C, von Schönfels W, Egberts JH, Försti A, Chen B, Lascorz J, Hemminki K, Franke A, Nothnagel M, Nöthlings U, Krawczak M (2013) Genome-wide investigation of gene-environment interactions in colorectal cancer. Hum Genet 132(2):219–231. https://doi.org/10.1007/s00439-012-1239-2
Zeng C, Matsuda K, Jia WH, Chang J, Kweon SS, Xiang YB, Shin A, Jee SH, Kim DH, Zhang B, Cai Q, Guo X, Long J, Wang N, Courtney R, Pan ZZ, Wu C, Takahashi A, Shin MH, Matsuo K, Matsuda F, Gao YT, Oh JH, Kim S, Jung KJ, Ahn YO, Ren Z, Li HL, Wu J, Shi J, Wen W, Yang G, Li B, Ji BT, Genetics and Epidemiology of Colorectal Cancer Consortium (GECCO), Brenner H, Schoen RE, Küry S, Colorectal Transdisciplinary (CORECT) Study, Gruber SB, Schumacher FR, Stenzel SL, Colon Cancer Family Registry (CCFR), Casey G, Hopper JL, Jenkins MA, Kim HR, Jeong JY, Park JW, Tajima K, Cho SH, Kubo M, Shu XO, Lin D, Zeng YX, Zheng W (2016) Identification of Susceptibility Loci and Genes for Colorectal Cancer Risk. Gastroenterology 150(7):1633–1645. https://doi.org/10.1053/j.gastro.2016.02.076
Song M, Garrett WS, Chan AT (2015) Nutrients, foods, and colorectal cancer prevention. Gastroenterology 148(6):1244–60.e16. https://doi.org/10.1053/j.gastro.2014.12.035
Murphy N, Moreno V, Hughes DJ, Vodicka L, Vodicka P, Aglago EK, Gunter MJ, Jenab M (2019) Lifestyle and dietary environmental factors in colorectal cancer susceptibility. Mol Aspects Med 69:2–9. https://doi.org/10.1016/j.mam.2019.06.005
Wu G, Fang YZ, Yang S, Lupton JR, Turner ND (2004) Glutathione metabolism and its implications for health. J Nutr 134(3):489–492. https://doi.org/10.1093/jn/134.3.489
Pizzorno J (2014) Glutathione! Integr Med (Encinitas) 13(1):8–12
Richie JP Jr (1992) The role of glutathione in aging and cancer. Exp Gerontol 27(5–6):615–626. https://doi.org/10.1016/0531-5565(92)90015-r
Richie JP Jr, Komninou D, Albino AP (2007) Induction of colon tumorigenesis by glutathione depletion in p53-knock-out mice. Int J Oncol 30(6):1539–1543
Jones DP, Coates RJ, Flagg EW, Eley JW, Block G, Greenberg RS, Gunter EW, Jackson B (1992) Glutathione in foods listed in the National Cancer Institute’s Health Habits and History Food Frequency Questionnaire. Nutr Cancer 17(1):57–75. https://doi.org/10.1080/01635589209514173
Traverso N, Ricciarelli R, Nitti M, Marengo B, Furfaro AL, Pronzato MA, Marinari UM, Domenicotti C (2013) Role of glutathione in cancer progression and chemoresistance. Oxid Med Cell Longev 2013:972913. https://doi.org/10.1155/2013/972913
Shiraishi R, Fujise T, Kuroki T, Kakimoto T, Miao L, Sakata Y, Tsunada S, Noda T, Iwakiri R, Fujimoto K (2009) Long-term ingestion of reduced glutathione suppressed an accelerating effect of beef tallow diet on colon carcinogenesis in rats. J Gastroenterol 44(10):1026–1035. https://doi.org/10.1007/s00535-009-0101-3
Hoensch H, Peters WH, Roelofs HM, Kirch W (2006) Expression of the glutathione enzyme system of human colon mucosa by localisation, gender and age. Curr Med Res Opin 22(6):1075–1083. https://doi.org/10.1185/030079906X112480
Kim AD, Zhang R, Han X, Kang KA, Piao MJ, Maeng YH, Chang WY, Hyun JW (2015) Involvement of glutathione and glutathione metabolizing enzymes in human colorectal cancer cell lines and tissues. Mol Med Rep 12(3):4314–4319. https://doi.org/10.3892/mmr.2015.3902
Moskalev AS, Barysheva EM, Soldatov VO, Frolova OG, Bobyntseva OV, Samgina TA, Churnosov MI, Ivanov VP, Polonikov AV, Bushueva OYu (2019) Association of C3435T (rs1045642) polymorphism of the MDR1 gene with the increased risk of colorectal cancer in Russian Females from Central Russia. Russ J Genet 55(12):1514–1519
Moskalev AS (2020) Association of L432V (rs1056836) polymorphism of the CYP1B1 gene with the increased risk of colorectal cancer in the population of Central Russia. Res Results Biomed 6(3):318–322
Polonikov AV, Klyosova EY, Azarova IE (2021) Bioinformatic tools and internet resources for functional annotation of polymorphic loci detected by genome wide association studies of multifactorial diseases (review). Res Results Biomed 7(1):15–31. https://doi.org/10.18413/2658-6533-2020-7-1-0-2
Solé X, Guinó E, Valls J, Iniesta R, Moreno V (2006) SNPStats: a web tool for the analysis of association studies. Bioinformatics 22(15):1928–1929. https://doi.org/10.1093/bioinformatics/btl268
Hoon DSB, Rahimzadeh N, Bustos MA (2021) EpiMap: fine-tuning integrative epigenomics maps to understand complex human regulatory genomic circuitry. Signal Transduct Target Ther 6(1):179. https://doi.org/10.1038/s41392-021-00620-5
Wang Z, Zang C, Rosenfeld JA, Schones DE, Barski A, Cuddapah S, Cui K, Roh TY, Peng W, Zhang MQ, Zhao K (2008) Combinatorial patterns of histone acetylations and methylations in the human genome. Nat Genet 40(7):897–903. https://doi.org/10.1038/ng.154
Chen L, Ge B, Casale FP, Vasquez L, Kwan T, Garrido-Martín D, Watt S, Yan Y, Kundu K, Ecker S, Datta A, Richardson D, Burden F, Mead D, Mann AL, Fernandez JM, Rowlston S, Wilder SP, Farrow S, Shao X, Lambourne JJ, Redensek A, Albers CA, Amstislavskiy V, Ashford S, Berentsen K, Bomba L, Bourque G, Bujold D, Busche S, Caron M, Chen SH, Cheung W, Delaneau O, Dermitzakis ET, Elding H, Colgiu I, Bagger FO, Flicek P, Habibi E, Iotchkova V, Janssen-Megens E, Kim B, Lehrach H, Lowy E, Mandoli A, Matarese F, Maurano MT, Morris JA, Pancaldi V, Pourfarzad F, Rehnstrom K, Rendon A, Risch T, Sharifi N, Simon MM, Sultan M, Valencia A, Walter K, Wang SY, Frontini M, Antonarakis SE, Clarke L, Yaspo ML, Beck S, Guigo R, Rico D, Martens JHA, Ouwehand WH, Kuijpers TW, Paul DS, Stunnenberg HG, Stegle O, Downes K, Pastinen T, Soranzo N (2016) Genetic drivers of epigenetic and transcriptional variation in human immune cells. Cell 167(5):1398-1414.e24. https://doi.org/10.1016/j.cell.2016.10.026
Sies H (1999) Glutathione and its role in cellular functions. Free Radic Biol Med 27(9–10):916–921. https://doi.org/10.1016/s0891-5849(99)00177-x
Lu SC (2009) Regulation of glutathione synthesis. Mol Aspects Med 30(1–2):42–59. https://doi.org/10.1016/j.mam.2008.05.005
Suthanthiran M et al (1990) Glutathione regulates activation-dependent DNA synthesis in highly purified normal human T lymphocytes stimulated via the CD2 and CD3 antigens. Proc Natl Acad Sci 87(9):3343–3347
Joncourt F, Oberli-Schrämmli AE, Stadler M, Buser K, Franscini L, Fey MF, Cerny T (1995) Patterns of drug resistance parameters in adult leukemia. Leuk Lymphoma 17(1–2):101–109. https://doi.org/10.3109/10428199509051709
Jardim BV, Moschetta MG, Leonel C, Gelaleti GB, Regiani VR, Ferreira LC, Lopes JR, Zuccari DA (2013) Glutathione and glutathione peroxidase expression in breast cancer: an immunohistochemical and molecular study. Oncol Rep 30(3):1119–1128. https://doi.org/10.3892/or.2013.2540
Cook JA, Pass HI, Iype SN, Friedman N, DeGraff W, Russo A, Mitchell JB (1991) Cellular glutathione and thiol measurements from surgically resected human lung tumor and normal lung tissue. Cancer Res 51(16):4287–4294
Mougiakakos D, Okita R, Ando T, Dürr C, Gadiot J, Ichikawa J, Zeiser R, Blank C, Johansson CC, Kiessling R (2012) High expression of GCLC is associated with malignant melanoma of low oxidative phenotype and predicts a better prognosis. J Mol Med (Berl) 90(8):935–944. https://doi.org/10.1007/s00109-012-0857-4
Nguyen LN, Munshi A, Hobbs ML, Story MD, Meyn RD (2001) Paclitaxel restores radiation-induced apoptosis in a bcl-2-expressing, radiation-resistant lymphoma cell line. Int J Radiat Oncol Biol Phys 49(4):1127–1132. https://doi.org/10.1016/s0360-3016(00)01435-8
Bolger JC, McCartan D, Walsh CA, Hao Y, Hughes E, Byrne C, Young LS (2012) Global analysis of breast cancer metastasis suggests cellular reprogramming is central to the endocrine resistant phenotype. In: Cancer research (vol 72). American Association of Cancer Research, Philadelphia
Nguyen A, Loo JM, Mital R, Weinberg EM, Man FY, Zeng Z, Paty PB, Saltz L, Janjigian YY, de Stanchina E, Tavazoie SF (2016) PKLR promotes colorectal cancer liver colonization through induction of glutathione synthesis. J Clin Invest 126(2):681–694. https://doi.org/10.1172/JCI83587
Rodrigues P, Furriol J, Bermejo B, Chaves FJ, Lluch A, Eroles P (2012) Identification of candidate polymorphisms on stress oxidative and DNA damage repair genes related with clinical outcome in breast cancer patients. Int J Mol Sci 13(12):16500–16513. https://doi.org/10.3390/ijms131216500
Koutros S, Andreotti G, Berndt SI, Hughes Barry K, Lubin JH, Hoppin JA, Kamel F, Sandler DP, Burdette LA, Yuenger J, Yeager M, Alavanja MC, Freeman LE (2011) Xenobiotic-metabolizing gene variants, pesticide use, and the risk of prostate cancer. Pharmacogenet Genomics 21(10):615–623. https://doi.org/10.1097/FPC.0b013e3283493a57
Xiong M (2007) Linkage disequilibrium and test for interaction between two loci. Curr Top Hum Genet 5:209. https://doi.org/10.1142/9789812790811_0009
Guerra R (2018) Adverse cutaneous drug eruptions: review of immunology, pathogenesis, and pharmacogenomics with focus on HIV and TEN. Diss. Harvard University
Vieira SM, Monteiro MB, Marques T, Luna AM, Fortes MA, Nery M, Queiroz M, Dib SA, Vendramini MF, Azevedo MJ, Canani LH, Parisi MC, Pavin EJ, Giannella-Neto D, Corrêa-Giannella ML (2011) Association of genetic variants in the promoter region of genes encoding p22phox (CYBA) and glutamate cysteine ligase catalytic subunit (GCLC) and renal disease in patients with type 1 diabetes mellitus. BMC Med Genet 12:129. https://doi.org/10.1186/1471-2350-12-129
Perez RV, Machado CG, Santos-Bezerra DP, Admoni SN, Patente TA, Monteiro MB, Cavaleiro AM, Queiroz MS, Nery M, Corrêa-Giannella ML (2019) Allelic variations in genes belonging to glutathione system increase proliferative retinopathy risk in type 1 diabetes individuals. Gene 703:120–124. https://doi.org/10.1016/j.gene.2019.04.015
Hama K, Fujiwara Y, Hayama T, Ozawa T, Nozawa K, Matsuda K, Hashiguchi Y, Yokoyama K (2021) Very long-chain fatty acids are accumulated in triacylglycerol and nonesterified forms in colorectal cancer tissues. Sci Rep 11(1):6163. https://doi.org/10.1038/s41598-021-85603-w
Hofmanová J, Slavík J, Ciganek M, Ovesná P, Tylichová Z, Karasová M, Zapletal O, Straková N, Procházková J, Bouchal J, Kolář Z, Ehrmann J, Levková M, Hušková Z, Skalický P, Kozubík A, Machala M, Vondráček J (2021) Complex alterations of fatty acid metabolism and phospholipidome uncovered in isolated colon cancer epithelial cells. Int J Mol Sci 22(13):6650. https://doi.org/10.3390/ijms22136650
Bocharova YA (2021) Associations between glutamate cysteine ligase catalytic subunit gene polymorphisms and clinical characteristics of ischemic stroke. Bull Russ State Med Univ 1:19–23
Pekowska A, Benoukraf T, Ferrier P, Spicuglia S (2010) A unique H3K4me2 profile marks tissue-specific gene regulation. Genome Res 20(11):1493–1502. https://doi.org/10.1101/gr.109389.110
Hussain SP, Hofseth LJ, Harris CC (2003) Radical causes of cancer. Nat Rev Cancer 3(4):276–285. https://doi.org/10.1038/nrc1046
Fedorinov DS, Lyadov VK, Sychev DA (2021) Genotype-based chemotherapy for patients with gastrointestinal tumors: focus on oxaliplatin, irinotecan, and fluoropyrimidines. Drug Metab Pers Ther. https://doi.org/10.1515/dmdi-2021-0162
Acknowledgements
This study was supported by the TRC GEN+ Genetic Research Foundation of Trans Russian Co (contract no. 474).
Funding
This study was supported by the TRC GEN + Genetic Research Foundation of Trans Russian Co (Contract No. 474).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Consent to publish
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Bykanova, M.A., Solodilova, M.A., Azarova, I.E. et al. Genetic variation at the catalytic subunit of glutamate cysteine ligase contributes to the susceptibility to sporadic colorectal cancer: a pilot study. Mol Biol Rep 49, 6145–6154 (2022). https://doi.org/10.1007/s11033-022-07406-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11033-022-07406-0