Abstract
Background
Acetaminophen (paracetamol, APAP) overdose is the principal cause of acute liver injury (ALI) that leads to liver failure typified with oxidative stress, mitochondrial and lysosomal dysfunction and with few antidotes for this condition. Therefore, more effective therapeutics are urgently required. Sinapic acid is a phenolic phytochemical with significant antioxidant, anti-inflammatory and hepatoprotective potential.
Rationale and purpose of the study
This study was conducted to evaluate hepatoprotective effect of this phytochemical in acetaminophen-induced model of ALI.
Methods and results
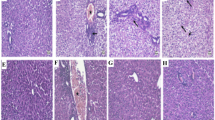
Male C57BL/6 mice were treated p.o. with sinapic acid (10 or 50 mg/kg) 3 times at 72, 24, and 1 h before APAP (300 mg/kg; i.p.) challenge. Functional factors of liver dysfunction were determined along with hepatic assessment of oxidative stress and inflammatory indexes and histopathological analysis was also conducted. Sinapic acid (50 mg/kg) properly decreased serum levels of ALT, ALP, and AST besides reducing liver level of ROS, MDA, IL-6, TNF-α, NF-kB, and MPO and improved sirtuin 1, HO-1, Nrf2, SOD activity, and MMP with no significant effect on IL-1β and catalase activity in addition to decreasing activity of lysosomal enzymes including cathepsin B and β-galactosidase. Also, sinapic acid at the higher dose ameliorated liver histopathological changes due to APAP and properly reversed NF-kB and Nrf2 immunoreactivity.
Conclusions
These findings show that sinapic acid pretreatment effectively protects liver against adverse and hepatotoxic effect of APAP through its antioxidant- and anti-inflammatory potential linked to NF-kB/Nrf2/HO-1 signaling and also via regulation of sirtuin 1, mitochondrial integrity, and lysosomal stabilization.





Similar content being viewed by others
Abbreviations
- ALI:
-
Acute liver injury
- ALT:
-
Alanine aminotransferase
- ALP:
-
Alkaline phosphatase
- APAP:
-
N-acetyl-para-aminophenol (Acetaminophen)
- AST:
-
Aspartate aminotransferase
- DCF-DA:
-
Dichlorofluorescein-diacetate
- GSH:
-
Glutathione
- HO-1:
-
Heme oxygenase 1
- IL-1β:
-
Interleukin-1β
- IL-6:
-
Interleukin-6
- MDA:
-
Malondialdehyde
- MMP:
-
Mitochondrial membrane potential
- MPO:
-
Myeloperoxidase
- NAPQI:
-
N-acetyl-para-benzo-quinone imine
- Nrf2:
-
Nuclear factor erythroid 2–related factor 2
- NF-kB:
-
Nuclear factor kappa-light-chain-enhancer of activated B cells
- ROS:
-
Reactive oxygen species
- SOD:
-
Superoxide dismutase
- TNFα:
-
Tumor necrosis factor α
References
Chen T, Li R, Chen P (2021) Gut microbiota and chemical-induced acute liver injury. Front Physiol 12:688780. https://doi.org/10.3389/fphys.2021.688780
Stravitz RT, Lee WM (2019) Acute liver failure. The Lancet 394:869–881. https://doi.org/10.1016/S0140-6736(19)31894-X
Yoon E, Babar A, Choudhary M, Kutner M, Pyrsopoulos N (2016) Acetaminophen-Induced Hepatotoxicity: a Comprehensive Update. J Clin Transl Hepatol 4:131–142
Jaeschke H, McGill MR, Ramachandran A (2012) Oxidant stress, mitochondria, and cell death mechanisms in drug-induced liver injury: lessons learned from acetaminophen hepatotoxicity. Drug Metab Rev 44:88–106. https://doi.org/10.3109/03602532.2011.602688
Yang R, Song C, Chen J, Zhou L, Jiang X, Cao X et al (2020) Limonin ameliorates acetaminophen-induced hepatotoxicity by activating Nrf2 antioxidative pathway and inhibiting NF-κB inflammatory response via upregulating Sirt1. Phytomedicine 69:153211. https://doi.org/10.1016/j.phymed.2020.153211
Olivo R, Guarrera JV, Pyrsopoulos NT (2018) Liver Transplantation for Acute Liver Failure. Clin Liver Dis 22:409–417. https://doi.org/10.1016/j.cld.2018.01.014
Jin Y, Wang H, Yi K, Lv S, Hu H, Li M et al (2020) Applications of nanobiomaterials in the therapy and imaging of acute liver failure. Nano-micro letters 13:25. https://doi.org/10.1007/s40820-020-00550-x
Ma L, Zheng J, Chen H, Zeng X, Wang S, Yang C et al (2021) A systematic screening of traditional Chinese medicine identifies two novel inhibitors against the cytotoxic aggregation of amyloid beta. Front Pharmacol. https://doi.org/10.3389/fphar.2021.637766
Nićiforović N, Abramovič H (2014) Sinapic acid and its derivatives: natural sources and bioactivity. Comprehen Rev Food Sci Food Safety 13:34–51. https://doi.org/10.1111/1541-4337.12041
Zare K, Eidi A, Roghani M, Rohani AH (2015) The neuroprotective potential of sinapic acid in the 6-hydroxydopamine-induced hemi-parkinsonian rat. Metab Brain Dis 30:205–213. https://doi.org/10.1007/s11011-014-9604-6
Yang C, Deng Q, Xu J, Wang X, Hu C, Tang H et al (2019) Sinapic acid and resveratrol alleviate oxidative stress with modulation of gut microbiota in high-fat diet-fed rats. Food Res Int (Ottawa, Ont) 116:1202–1211. https://doi.org/10.1016/j.foodres.2018.10.003
Shin DS, Kim KW, Chung HY, Yoon S, Moon JO (2013) Effect of sinapic acid against carbon tetrachloride-induced acute hepatic injury in rats. Arch Pharmacal Res 36:626–633. https://doi.org/10.1007/s12272-013-0050-5
Shin DS, Kim KW, Chung HY, Yoon S, Moon JO (2013) Effect of sinapic acid against dimethylnitrosamine-induced hepatic fibrosis in rats. Arch Pharmacal Res 36:608–618. https://doi.org/10.1007/s12272-013-0033-6
Ahmad A, Alkharfy KM, Bin Jardan YA, Shahid M, Ansari MA, Alqahtani S et al (2021) Sinapic acid mitigates methotrexate-induced hepatic injuries in rats through modulation of Nrf-2/HO-1 signaling. Environ Toxicol 36:1261–1268. https://doi.org/10.1002/tox.23123
Ansari MA, Raish M, Bin Jardan YA, Ahmad A, Shahid M, Ahmad SF et al (2021) Sinapic acid ameliorates D-galactosamine/lipopolysaccharide-induced fulminant hepatitis in rats: Role of nuclear factor erythroid-related factor 2/heme oxygenase-1 pathways. World J Gastroenterol 27:592–608. https://doi.org/10.3748/wjg.v27.i7.592
Roy SJ, Stanely Mainzen Prince P (2012) Protective effects of sinapic acid on lysosomal dysfunction in isoproterenol induced myocardial infarcted rats. Food Chem Toxicol 50:3984–3989. https://doi.org/10.1016/j.fct.2012.08.017
Stanely Mainzen Prince P, Dey P, Roy SJ (2020) Sinapic acid safeguards cardiac mitochondria from damage in isoproterenol-induced myocardial infarcted rats. J Biochem Mol Toxicol 34:e22556. https://doi.org/10.1002/jbt.22556
Wimborne HJ, Hu J, Takemoto K, Nguyen NT, Jaeschke H, Lemasters JJ et al (2020) Aldehyde dehydrogenase-2 activation decreases acetaminophen hepatotoxicity by prevention of mitochondrial depolarization. Toxicol Appl Pharmacol 396:114982. https://doi.org/10.1016/j.taap.2020.114982
Silambarasan T, Manivannan J, Raja B, Chatterjee S (2016) Prevention of cardiac dysfunction, kidney fibrosis and lipid metabolic alterations in l-NAME hypertensive rats by sinapic acid–Role of HMG-CoA reductase. Eur J Pharmacol 777:113–123. https://doi.org/10.1016/j.ejphar.2016.03.004
Mondal M, Hossain MM, Hasan MR, Tarun MTI, Islam MAF, Choudhuri MSK et al (2020) Hepatoprotective and antioxidant capacity of mallotus repandus ethyl acetate stem extract against d-galactosamine-induced hepatotoxicity in rats. ACS Omega 5:6523–6531. https://doi.org/10.1021/acsomega.9b04189
Mohamadi-Zarch SM, Baluchnejadmojarad T, Nourabadi D, Khanizadeh AM, Roghani M (2020) Protective effect of diosgenin on LPS/D-Gal-induced acute liver failure in C57BL/6 mice. Microb Pathog 146:104243. https://doi.org/10.1016/j.micpath.2020.104243
Sedlak J, Lindsay RH (1968) Estimation of total, protein-bound, and nonprotein sulfhydryl groups in tissue with Ellman’s reagent. Anal Biochem 25:192–205. https://doi.org/10.1016/0003-2697(68)90092-4
Nandi A, Chatterjee IB (1988) Assay of superoxide dismutase activity in animal tissues. J Biosci 13:305–315. https://doi.org/10.1007/BF02712155
Aebi H. [13] Catalase in vitro. Methods Enzymol. 105: Academic Press; 1984. p. 121–6.
Khosravi Z, Sedaghat R, Baluchnejadmojarad T, Roghani M (2019) Diosgenin ameliorates testicular damage in streptozotocin-diabetic rats through attenuation of apoptosis, oxidative stress, and inflammation. Int Immunopharmacol 70:37–46
Baluchnejadmojarad T, Mohamadi-Zarch SM, Roghani M (2019) Safranal, an active ingredient of saffron, attenuates cognitive deficits in amyloid β-induced rat model of Alzheimer’s disease: underlying mechanisms. Metab Brain Dis 34:1747–1759. https://doi.org/10.1007/s11011-019-00481-6
Korolenko TA, Johnston TP, Tuzikov FV, Tuzikova NA, Pupyshev AB, Spiridonov VK et al (2016) Early-stage atherosclerosis in poloxamer 407-induced hyperlipidemic mice: pathological features and changes in the lipid composition of serum lipoprotein fractions and subfractions. Lipids Health Dis 15:16. https://doi.org/10.1186/s12944-016-0186-7
Barrett AJ, Kirschke H (1981) Cathepsin B, Cathepsin H, and cathepsin L. Methods Enzymol. https://doi.org/10.1016/s0076-6879(81)80043-2
Lyu Z, Ji X, Chen G, An B (2019) Atractylodin ameliorates lipopolysaccharide and d-galactosamine-induced acute liver failure via the suppression of inflammation and oxidative stress. Int Immunopharmacol 72:348–357. https://doi.org/10.1016/j.intimp.2019.04.005
Ali SA, Sharief NH, Mohamed YS (2019) Hepatoprotective activity of some medicinal plants in Sudan. Evid Based Complement Alternat Med 2019:2196315. https://doi.org/10.1155/2019/2196315
Giannini EG, Testa R, Savarino V (2005) Liver enzyme alteration: a guide for clinicians. CMAJ 172:367–379. https://doi.org/10.1503/cmaj.1040752
Xiong W, Yuan Z, Wang T, Wu S, Xiong Y, Yao Y et al (2021) Quercitrin attenuates acetaminophen-induced acute liver injury by maintaining mitochondrial complex I Activity. Front Pharmacol 12:586010. https://doi.org/10.3389/fphar.2021.586010
Araujo J, Zhang M, Yin F (2012) Heme oxygenase-1, oxidation, inflammation, and atherosclerosis. Front Pharmacol. https://doi.org/10.3389/fphar.2012.00119
Baluchnejadmojarad T, Zeinali H, Roghani M (2018) Scutellarin alleviates lipopolysaccharide-induced cognitive deficits in the rat: Insights into underlying mechanisms. Int Immunopharmacol 54:311–319. https://doi.org/10.1016/j.intimp.2017.11.033
Liu FC, Yu HP, Chou AH, Lee HC, Liao CC (2020) Corilagin reduces acetaminophen-induced hepatotoxicity through MAPK and NF-κB signaling pathway in a mouse model. Am J Transl Res 12:5597–5607
Mulita F, Karpetas G, Liolis E, Vailas M, Tchabashvili L, Maroulis I (2021) Comparison of analgesic efficacy of acetaminophen monotherapy versus acetaminophen combinations with either pethidine or parecoxib in patients undergoing laparoscopic cholecystectomy: a randomized prospective study. Med Glas 18:27–32
Akakpo JY, Ramachandran A, Orhan H, Curry SC, Rumack BH, Jaeschke H (2020) 4-methylpyrazole protects against acetaminophen-induced acute kidney injury. Toxicol Appl Pharmacol 409:115317. https://doi.org/10.1016/j.taap.2020.115317
Islam MT, Quispe C, Islam MA, Ali ES, Saha S, Asha UH et al (2021) Effects of nerol on paracetamol-induced liver damage in Wistar albino rats. Biomed Pharmacotherapy. https://doi.org/10.1016/j.biopha.2021.111732
Hanawa N, Shinohara M, Saberi B, Gaarde WA, Han D, Kaplowitz N (2008) Role of JNK translocation to mitochondria leading to inhibition of mitochondria bioenergetics in acetaminophen-induced liver injury. J Biol Chem 283:13565–13577. https://doi.org/10.1074/jbc.M708916200
Nakagawa H, Maeda S, Hikiba Y, Ohmae T, Shibata W, Yanai A et al (2008) Deletion of apoptosis signal-regulating kinase 1 attenuates acetaminophen-induced liver injury by inhibiting c-Jun N-terminal kinase activation. Gastroenterology 135:1311–1321. https://doi.org/10.1053/j.gastro.2008.07.006
Huang R, Pan H, Zhou M, Jin J, Ju Z, Ren G et al (2021) Potential liver damage due to co-exposure to As, Cd, and Pb in mining areas: Association analysis and research trends from a Chinese perspective. Environ Res 201:111598. https://doi.org/10.1016/j.envres.2021.111598
Jaeschke H, Williams CD, McGill MR, Xie Y, Ramachandran A (2013) Models of drug-induced liver injury for evaluation of phytotherapeutics and other natural products. Food Chem Toxicol 55:279–289. https://doi.org/10.1016/j.fct.2012.12.063
Shan Z, Ju C (2020) Hepatic macrophages in liver injury. Front Immunol. https://doi.org/10.3389/fimmu.2020.00322
Pan CW, Pan ZZ, Hu JJ, Chen WL, Zhou GY, Lin W et al (2016) Mangiferin alleviates lipopolysaccharide and D-galactosamine-induced acute liver injury by activating the Nrf2 pathway and inhibiting NLRP3 inflammasome activation. Eur J Pharmacol 770:85–91. https://doi.org/10.1016/j.ejphar.2015.12.006
Deng JS, Jiang WP, Chen CC, Lee LY, Li PY, Huang WC et al (2020) Cordyceps cicadae mycelia ameliorate cisplatin-induced acute kidney injury by suppressing the TLR4/NF-kappaB/MAPK and activating the HO-1/Nrf2 and Sirt-1/AMPK pathways in mice. Oxid Med Cell Longev 2020:7912763. https://doi.org/10.1155/2020/7912763
Tian W, Zhao J, Choo BK, Kim IS, Ahn D, Tae HJ et al (2021) Camellia japonica diminishes acetaminophen-induced acute liver failure by attenuating oxidative stress in mice. Environ Sci Pollut Res Int. https://doi.org/10.1007/s11356-021-14530-0
Jaeschke H, Hasegawa T (2006) Role of neutrophils in acute inflammatory liver injury. Liver Int 26:912–919
He M, Horuk R, Moochhala SM, Bhatia M (2007) Treatment with BX471, a CC chemokine receptor 1 antagonist, attenuates systemic inflammatory response during sepsis. Am J Physiol Gastrointest Liver Physiol 292:G1173–G1180. https://doi.org/10.1152/ajpgi.00420.2006
Kasai S, Shimizu S, Tatara Y, Mimura J, Itoh K (2020) Regulation of Nrf2 by mitochondrial reactive oxygen species in physiology and pathology. Biomolecules. https://doi.org/10.3390/biom10020320
Habtemariam S (2019) The Nrf2/HO-1 axis as targets for flavanones: neuroprotection by pinocembrin, naringenin, and eriodictyol. Oxid Med Cell Longev 2019:4724920. https://doi.org/10.1155/2019/4724920
Wei X, Wang H, Sun X, Huang X, Xu W, Liang Y et al (2020) 4-hydroxy-2(3H)-benzoxazolone alleviates acetaminophen-induced hepatic injury by inhibiting NF-κB and activating Nrf2/HO-1 signaling pathways. Am J Transl Res 12:2169–2180
Du K, Ramachandran A, Jaeschke H (2016) Oxidative stress during acetaminophen hepatotoxicity: Sources, pathophysiological role and therapeutic potential. Redox Biol 10:148–156. https://doi.org/10.1016/j.redox.2016.10.001
Lei XG, Zhu JH, Cheng WH, Bao Y, Ho YS, Reddi AR et al (2016) Paradoxical roles of antioxidant enzymes: basic mechanisms and health implications. Physiol Rev 96:307–364. https://doi.org/10.1152/physrev.00010.2014
Gaweł S, Wardas M, Niedworok E, Wardas P (2004) Malondialdehyde (MDA) as a lipid peroxidation marker. Wiad Lek 57:453–455
Zorov DB, Juhaszova M, Sollott SJ (2006) Mitochondrial ROS-induced ROS release: an update and review. Biochim Biophys Acta 1757:509–517. https://doi.org/10.1016/j.bbabio.2006.04.029
Murphy MP (2009) How mitochondria produce reactive oxygen species. Biochem J 417:1–13. https://doi.org/10.1042/bj20081386
Guo H, Sun J, Li D, Hu Y, Yu X, Hua H et al (2019) Shikonin attenuates acetaminophen-induced acute liver injury via inhibition of oxidative stress and inflammation. Biomed Pharmacother 112:108704. https://doi.org/10.1016/j.biopha.2019.108704
Jiang W, Zhang X, Hao J, Shen J, Fang J, Dong W et al (2014) SIRT1 protects against apoptosis by promoting autophagy in degenerative human disc nucleus pulposus cells. Sci Rep 4:7456. https://doi.org/10.1038/srep07456
Li Y, Xu W, McBurney MW, Longo VD (2008) SirT1 inhibition reduces IGF-I/IRS-2/Ras/ERK1/2 signaling and protects neurons. Cell Metab 8:38–48. https://doi.org/10.1016/j.cmet.2008.05.004
Yang H, Zhang W, Pan H, Feldser HG, Lainez E, Miller C et al (2012) SIRT1 activators suppress inflammatory responses through promotion of p65 deacetylation and inhibition of NF-κB activity. PLoS ONE 7:e46364. https://doi.org/10.1371/journal.pone.0046364
Moles A, Torres S, Baulies A, Garcia-Ruiz C, Fernandez-Checa JC (2018) Mitochondrial-lysosomal axis in acetaminophen hepatotoxicity. Front Pharmacol 9:453. https://doi.org/10.3389/fphar.2018.00453
Silambarasan T, Manivannan J, Priya MK, Suganya N, Chatterjee S, Raja B (2015) Sinapic acid protects heart against ischemia/reperfusion injury and H9c2 cardiomyoblast cells against oxidative stress. Biochem Biophys Res Commun 456:853–859. https://doi.org/10.1016/j.bbrc.2014.12.022
Hu J, Kholmukhamedov A, Lindsey CC, Beeson CC, Jaeschke H, Lemasters JJ (2016) Translocation of iron from lysosomes to mitochondria during acetaminophen-induced hepatocellular injury: Protection by starch-desferal and minocycline. Free Radical Biol Med 97:418–426. https://doi.org/10.1016/j.freeradbiomed.2016.06.024
Acknowledgements
This research project was financially supported in 2019 by National Institute for Medical Research Development (NIMAD) of Iran (Grant number 987706).
Funding
This article was funded by National Institute for Medical Research Development (987706).
Author information
Authors and Affiliations
Contributions
AR performed the experiments of the study. MR analyzed the data, supervised the study, and write the manuscript. TB helped in performing experiments and assisted in statistical analysis and manuscript preparation. All authors read and reviewed the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethical approval
All procedures of this study involving animals were approved by NIMAD Institute (Tehran, Iran) (IR.NIMAD.REC.1399.007) which were in compliance with NIH recommended guidelines.
Consent to participate
No such consent was required for this experimental study.
Consent to publish
All mentioned authors agreed on publication of this manuscript and gave explicit consent to submit. In addition, explicit consent from the responsible authorities at the institute/organization where the work has been carried out has been obtained before submission.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Rostami, A., Baluchnejadmojarad, T. & Roghani, M. Sinapic acid ameliorates paracetamol-induced acute liver injury through targeting oxidative stress and inflammation. Mol Biol Rep 49, 4179–4191 (2022). https://doi.org/10.1007/s11033-022-07251-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11033-022-07251-1