Abstract
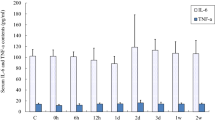
Eccentric exercise has been extensively used as a model to study the contraction-induced muscle damage and its consequent processes. This study aimed at examining molecular responses associated with tissue remodelling, inflammation and angiogenesis in skeletal muscle during the recovery period after eccentric exercise in humans. Ten healthy men performed 50 maximal eccentric muscle actions with the knee extensors and muscle biopsies were collected from the vastus lateralis before and 6 h, 48 h and 120 h post eccentric exercise. Real Time-PCR was utilized to investigate alterations in gene expression of various tissue remodelling-, inflammation- and angiogenesis-related factors: uPA, uPA-R, TGF-β1, MMP-9, TNF-α, IL-6, IL-8, VEGF, VEGFR-2, HIF-1a, Ang-1, Ang-2 and Tie-2. The uPA/uPA-R system exhibited a similar time-expression pattern increasing 6 h post exercise (p < 0.05), while the other tissue remodelling factors TGF-β1 and MMP-9 did not change significantly over time. Transcriptional responses of inflammatory factors TNF-α and IL-8 increased significantly and peaked 6 h post eccentric exercise (p < 0.05), while IL-6 exhibited a similar, though not statistically significant, expression profile (p > 0.05). Similarly, the expression of angiopoietin receptor Tie-2 showed an early increase only at 6 h after the completion of exercise (p < 0.05), while the other angiogenic factors failed to reach statistical significance due a high interindividual variability in the gene expression responses. The early transcriptional upregulation of tissue remodelling, inflammation- and angiogenesis-related factors post eccentric exercise may indicate the acute intramuscular activation of these processes functionally related to muscle damage-induced adaptation.




Similar content being viewed by others
References
Philippou A, Papageorgiou E, Bogdanis G, Halapas A, Sourla A, Maridaki M, Pissimissis N, Koutsilieris M (2009) Expression of IGF-1 isoforms after exercise-induced muscle damage in humans: characterization of the MGF E peptide actions in vitro. Vivo 23:567–575
Peake JM, Neubauer O, Della Gatta PA (1985) Nosaka K (2017) Muscle damage and inflammation during recovery from exercise. J Appl Physiol 122:559–570
Proske U, Morgan DL (2001) Muscle damage from eccentric exercise: mechanism, mechanical signs, adaptation and clinical applications. J Physiol 537:333–345
Jones DA, Newham DJ, Round JM, Tolfree SE (1986) Experimental human muscle damage: morphological changes in relation to other indices of damage. J Physiol 375:435–448
Philippou A, Bogdanis G, Maridaki M, Halapas A, Sourla A, Koutsilieris M (2009) Systemic cytokine response following exercise-induced muscle damage in humans. Clin Chem Lab Med 47:777–782
Hyldahl RD, Hubal MJ (2014) Lengthening our perspective: morphological, cellular, and molecular responses to eccentric exercise. Muscle Nerve 49:155–170
Philippou A, Bogdanis GC, Maridaki M (2010) Neuromuscular dysfunction with the experimental arm acting as its own reference following eccentric and isometric exercise. Somatosens Mot Res 27:45–54
Philippou A, Maridaki M, Bogdanis GC (2003) Angle-specific impairment of elbow flexors strength after isometric exercise at long muscle length. J Sports Sci 21:859–865
Philippou A, Bogdanis GC, Nevill AM, Maridaki M (2004) Changes in the angle-force curve of human elbow flexors following eccentric and isometric exercise. Eur J Appl Physiol 93:237–244
Philippou A, Bogdanis GC, Maridaki M (2007) Isotonic muscle function is selectively reduced after muscle damage induced by isometric exercise at a long muscle length. Isokinet Exerc Sci 15:69–75
Philippou A, Koutsilieris M, Maridaki M (2012) Changes in kinematic variables at various muscle lengths of human elbow flexors following eccentric exercise. J Muscle Res Cell Motil 33:167–175
Philippou A, Maridaki M, Theos A, Koutsilieris M (2012) Cytokines in muscle damage. Adv Clin Chem 58:49–87
Philippou A, Maridaki M, Psarros C, Koutsilieris M (2018) Systemic Responses of Inflammation-Related Factors Following Eccentric Exercise in Humans. American Journal of Sports Science 6:69–75
Philippou A, Maridaki M, Tenta R, Koutsilieris M (2018) Hormonal responses following eccentric exercise in humans. Hormones (Athens) 16:405–413
Zembron-Lacny A, Naczk M, Gajewski M, Ostapiuk-Karolczuk J, Dziewiecka H, Kasperska A, Szyszka K (2010) Changes of muscle-derived cytokines in relation to thiol redox status and reactive oxygen and nitrogen species. Physiol Res 59:945–951
Chazaud B (2016) Inflammation during skeletal muscle regeneration and tissue remodeling: application to exercise-induced muscle damage management. Immunol Cell Biol 94:140–145
Deng B, Wehling-Henricks M, Villalta SA, Wang Y, Tidball JG (2012) IL-10 triggers changes in macrophage phenotype that promote muscle growth and regeneration. J Immunol 189:3669–3680
Philippou A, Maridaki M, Koutsilieris M (2008) The role of urokinase-type plasminogen activator (uPA) and transforming growth factor beta 1 (TGFbeta1) in muscle regeneration. Vivo 22:735–750
Paulsen G, Mikkelsen UR, Raastad T, Peake JM (2012) Leucocytes, cytokines and satellite cells: what role do they play in muscle damage and regeneration following eccentric exercise? Exerc Immunol Rev 18:42–97
Jarvinen TA, Jarvinen M, Kalimo H (2014) Regeneration of injured skeletal muscle after the injury. Muscles Ligaments Tendons J 3:337–345
Stauber WT, Clarkson PM, Fritz VK (1985) Evans WJ (1990) Extracellular matrix disruption and pain after eccentric muscle action. J Appl Physiol 69:868–874
Brown S, Day S, Donnelly A (1999) Indirect evidence of human skeletal muscle damage and collagen breakdown after eccentric muscle actions. J Sports Sci 17:397–402
Mackey AL (1985) Kjaer M (2016) Connective tissue regeneration in skeletal muscle after eccentric contraction-induced injury. J Appl Physiol 122:533–540
Karalaki M, Fili S, Philippou A, Koutsilieris M (2009) Muscle regeneration: cellular and molecular events. Vivo 23:779–796
Buford TW, MacNeil RG, Clough LG, Dirain M, Sandesara B, Pahor M, Manini TM (1985) Leeuwenburgh C (2014) Active muscle regeneration following eccentric contraction-induced injury is similar between healthy young and older adults. J Appl Physiol 116:1481–1490
Philippou A, Maridaki M, Bogdanis G, Halapas A, Koutsilieris M (2009) Changes in the mechanical properties of human quadriceps muscle after eccentric exercise. Vivo 23:859–865
Tzanis G, Philippou A, Karatzanos E, Dimopoulos S, Kaldara E, Nana E, Pitsolis T, Rontogianni D, Koutsilieris M, Nanas S (2016) Effects of high-intensity interval exercise training on skeletal myopathy of chronic heart failure. J Card Fail 23:36–46
Chen TC, Chen HL, Pearce AJ, Nosaka K (2012) Attenuation of eccentric exercise-induced muscle damage by preconditioning exercises. Med Sci Sports Exerc 44:2090–2098
Damas F, Nosaka K, Libardi CA, Chen TC, Ugrinowitsch C (2016) Susceptibility to exercise-induced muscle damage: a cluster analysis with a large sample. Int J Sports Med 37:633–640
Stavropoulou A, Philippou A, Halapas A, Sourla A, Pissimissis N, Koutsilieris M (2010) uPA, uPAR and TGFbeta(1) expression during early and late post myocardial infarction period in rat myocardium. Vivo 24:647–652
Smith C, Kruger MJ, Smith RM, Myburgh KH (2008) The inflammatory response to skeletal muscle injury: illuminating complexities. Sports Med 38:947–969
Munoz-Canoves P, Scheele C, Pedersen BK, Serrano AL (2013) Interleukin-6 myokine signaling in skeletal muscle: a double-edged sword? FEBS J 280:4131–4148
Tidball JG, Villalta SA (2010) Regulatory interactions between muscle and the immune system during muscle regeneration. Am J Physiol Regul Integr Comp Physiol 298:R1173-1187
Petersen AM (1985) Pedersen BK (2005) The anti-inflammatory effect of exercise. J Appl Physiol 98:1154–1162
Pedersen BK, Fischer CP (2007) Beneficial health effects of exercise–the role of IL-6 as a myokine. Trends Pharmacol Sci 28:152–156
Akerstrom T, Steensberg A, Keller P, Keller C, Penkowa M, Pedersen BK (2005) Exercise induces interleukin-8 expression in human skeletal muscle. J Physiol 563:507–516
Pedersen BK, Akerstrom TC, Nielsen AR (1985) Fischer CP (2007) Role of myokines in exercise and metabolism. J Appl Physiol 103:1093–1098
Suzuki K (2018) Cytokine Response to Exercise and Its Modulation. Antioxidants (Basel). https://doi.org/10.3390/antiox7010017
Polesskaya A, Pinna G, Sassi Y, Vandamme M, Bigot A, Mouly V, Morozova N, Harel-Bellan A, Degerny C (2016) Post-transcriptional modulation of interleukin 8 by CNOT6L regulates skeletal muscle differentiation. Biochim Biophys Acta 1863:263–270
Amir Levy Y, Ciaraldi TP, Mudaliar SR, Phillips SA, Henry RR (2015) Excessive secretion of IL-8 by skeletal muscle in type 2 diabetes impairs tube growth: potential role of PI3K and the Tie2 receptor. Am J Physiol Endocrinol Metab 309:E22-34
Novak ML, Bryer SC, Cheng M, Nguyen MH, Conley KL, Cunningham AK, Xue B, Sisson TH, You JS, Hornberger TA, Koh TJ (2011) Macrophage-specific expression of urokinase-type plasminogen activator promotes skeletal muscle regeneration. J Immunol 187:1448–1457
Suelves M, Lopez-Alemany R, Lluis F, Aniorte G, Serrano E, Parra M, Carmeliet P, Munoz-Canoves P (2002) Plasmin activity is required for myogenesis in vitro and skeletal muscle regeneration in vivo. Blood 99:2835–2844
Tidball JG, Dorshkind K, Wehling-Henricks M (2014) Shared signaling systems in myeloid cell-mediated muscle regeneration. Development 141:1184–1196
Rahman FA, Angus SA, Stokes K, Karpowicz P, Krause MP (2020) Impaired ECM remodeling and macrophage activity define necrosis and regeneration following damage in aged skeletal muscle. Int J Mol Sci. https://doi.org/10.3390/ijms21134575
Wang X, Yu YY, Lieu S, Yang F, Lang J, Lu C, Werb Z, Hu D, Miclau T, Marcucio R, Colnot C (2012) MMP9 regulates the cellular response to inflammation after skeletal injury. Bone 52:111–119
Arroyo AG, Iruela-Arispe ML (2010) Extracellular matrix, inflammation, and the angiogenic response. Cardiovasc Res 86:226–235
Olfert IM, Baum O, Hellsten Y, Egginton S (2015) Advances and challenges in skeletal muscle angiogenesis. Am J Physiol Heart Circ Physiol 310:H326-336
Hellsten Y, Hoier B (2014) Capillary growth in human skeletal muscle: physiological factors and the balance between pro-angiogenic and angiostatic factors. Biochem Soc Trans 42:1616–1622
Acknowledgements
The invaluable contribution of the study participants to this research is greatly acknowledged.
Funding
The authors received no financial support for this article.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Ethical approval
The Ethics Committee of the National and Kapodistrian University of Athens approved the present study and all experimental procedures conformed to the Declaration of Helsinki. A written informed consent was obtained from all the participants.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Philippou, A., Tryfonos, A., Theos, A. et al. Expression of tissue remodelling, inflammation- and angiogenesis-related factors after eccentric exercise in humans. Mol Biol Rep 48, 4047–4054 (2021). https://doi.org/10.1007/s11033-021-06412-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11033-021-06412-y