Abstract
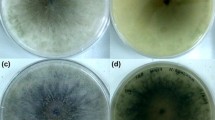
Luliconazole is an imidazole antifungal agent used in topical form for the treatment of onychomycosis and dermatophytosis. In vitro activity of luliconazole against dermatophytes, Candida, black fungi, Fusarium and Aspergillus species have been investigated. Rhodotorula spp. are environmental yeasts and emerged as opportunistic pathogens among immunocompromised patients. Rhodotorula’s human infections are usually resistant to treatment with antifungal drugs especially triazoles and echinocandins. The present study aimed at the molecular detection of environmental isolates of Rhodotorula spp. Then, antifungal efficacy of luliconazole was evaluated against isolates and compared to other routine systemic antifungals including; caspofungin, posaconazole, fluconazole, itraconazole, amphotericin B, and voriconazole. The biofilm production of Rhodotorula isolates was also evaluated. In this study, 39 isolates of Rhodotorula spp. were isolated from the environment, detected using molecular methods, and tested against luliconazole. Then, the anti-fungal activity of luliconazole compared with several routine antifungals. Also, biofilm formation by using a crystal violet staining assay was performed. Our finding showed that luliconazole has a very high minimum inhibitory concentration (MIC) value (1–8 µg/ml) against Rhodotorula spp. Besides, 100% of Rhodotorula strains were resistant to caspofungin, followed by fluconazole 94.7% and voriconazole 74.4%. Amphotericin B was demonstrated excellent in vitro activity against this genus. Our result indicated that 59% of Rhodotorula spp. were in the mid-range of biofilm production. Our results indicated that luliconazole does not effective against the genus Rhodotorula. Furthermore, amphotericin B is the best drug against this genus in comparison to caspofungin and other azole drugs.

Similar content being viewed by others
References
Scorzetti G, Fell JW, Fonseca A, Statzell-Tallman A (2002) Systematics of basidiomycetous yeasts: a comparison of large subunit D1/D2 and internal transcribed spacer rDNA regions. FEMS Yeast Res 2(4):495–517. https://doi.org/10.1111/j.1567-1364.2002.tb00117.x
Lo Re V III, Fishman N, Nachamkin I (2003) Recurrent catheter-related Rhodotorula rubra infection. Clin Microbiol Infect 9(8):897–900. https://doi.org/10.1046/j.1469-0691.2003.00641.x
Vazquez JA. Rhodotorula, saccharomyces, malassezia, trichosporon, blastoschizomyces, and sporobolomyces. Essentials of Clinical Mycology: Springer; 2011. p. 227–239
Wirth F, Goldani LZ (2012) Epidemiology of Rhodotorula: an emerging pathogen. Interdiscip Perspect Infect Dis 2012:465717. https://doi.org/10.1155/2012/465717
Menon S, Gupta HR, Sequeira R, Chavan S, Gholape D, Amandeep S et al (2014) Rhodotorula glutinis meningitis: a case report and review of literature. Mycoses 57(7):447–451. https://doi.org/10.1111/myc.12180
Ruiz-Aragón J, García-Agudo L, García-Martos P, Marín P, García-Tapia A, Moya P (2005) Enzymatic activity of Rhodotorula glutinis strains isolated from clinical and environmental sources. Mikologia Lekarska 12(1):11–13
Seifi Z, Mahmoudabadi AZ, Hydrinia S (2013) Isolation, identification and susceptibility profile of Rhodotorula species isolated from two educational hospitals in Ahvaz. Jundishapur J Microbiol 6(6):e8935. https://doi.org/10.5812/jjm.8935
Guidara R, Trabelsi H, Neji S, Cheikhrouhou F, Sellami H, Makni F et al (2016) Rhodotorula fungemia: Report of two cases in Sfax (Tunisia). J Mycol Med 26(2):178–181. https://doi.org/10.1016/j.mycmed.2016.02.020
Al-Obaid I, Khan Z, Ahmad S, Emara M, Burhama M, Purohit P et al (2011) Persistent catheter-related Rhodotorula mucilaginosa fungemia in a leukemic child. J Mycol Med 21(2):134–137. https://doi.org/10.1016/j.mycmed.2011.02.001
Tiamiyu AB, Dayyab FM, Edwin CP, Iliyasu G, Dalhat MM, Habib AG (2014) Rhodotorula spp. infection presenting as meningitis and fungaemia in human immunodeficiency virus infected patient. Ann Nigerian Med 8(1):48–50. https://doi.org/10.4103/0331-3131.141031
Simon MS, Somersan S, Singh HK, Hartman B, Wickes BL, Jenkins SG et al (2014) Endocarditis caused by Rhodotorula infection. J Clin Microbiol 52(1):374–378. https://doi.org/10.1128/JCM.01950-13
Lanzafame M, De Checchi G, Parinello A, Trevenzoli M, Cattelan AM (2001) Rhodotorula glutinis-related meningitis. J Clin Microbiol 39(1):410. https://doi.org/10.1128/jcm.39.1.410.2001
Giovannini J, Lee R, Zhang SX, Jun AS, Bower KS (2014) Rhodotorula keratitis: a rarely encountered ocular pathogen. Case Rep Ophthalmol 5(3):302–310. https://doi.org/10.1159/000365986
Saha S, Sengupta J, Chatterjee D, Banerjee D (2014) Rhodotorula mucilaginosa Keratitis: a rare fungus from Eastern India. Indian J Ophthalmol 62(3):341–344. https://doi.org/10.4103/0301-4738.111133
Rajmane VS, Rajmane ST, Ghatole MP (2011) Rhodotorula species infection in traumatic keratitis—a case report. Diagn Microbiol Infect Dis 71(4):428–429. https://doi.org/10.1016/j.diagmicrobio.2011.08.009
Maeder M, Vogt PR, Schaer G, von Graevenitz A, Gunthard HF (2003) Aortic homograft endocarditis caused by Rhodotorula mucilaginosa. Infection 31(3):181–183. https://doi.org/10.1007/s15010-002-3155-1
Maurya V, Khatri P, Meena S, Bora A, Seervi K, Rathore L et al (2015) Onychomycosis caused by Rhodotorula glutinis: A case report. Int J Curr Microbiol App Sci 4(11):331–335
Bhattacharyya S, Shivaprakash M, Chakrabarti A, Sharma N (2012) Foot bleb infection due to Rhodotorula mucilaginosa in a diabetic patient: Case report and review of the literature. Biomed Res 23(4):577–579
Savini V, Sozio F, Catavitello C, Talia M, Manna A, Febbo F et al (2008) Femoral prosthesis infection by Rhodotorula mucilaginosa. J Clin Microbiol 46(10):3544–3545. https://doi.org/10.1128/JCM.00873-08
Anica Buzejić SG, Ivana Radojević A, Ostojić L, Čomić S Vasić (2016) Pb and Hg heavy metal tolerance of single and mixed-species biofilm (Rhodotorula mucilaginosa and Escherichia coli). Kragujevac J Sci 38:115–124
Rodrigues ME, Gomes F, Rodrigues CF (2019) Candida spp Bacteria Mixed Biofilms. J Fungi (Basel). https://doi.org/10.3390/jof6010005
Nunes JM, Bizerra FC, Ferreira RC, Colombo AL (2013) Molecular identification, antifungal susceptibility profile, and biofilm formation of clinical and environmental Rhodotorula species isolates. Antimicrob Agents Chemother 57(1):382–389. https://doi.org/10.1128/AAC.01647-12
Scher RK, Nakamura N, Tavakkol A (2014) Luliconazole: a review of a new antifungal agent for the topical treatment of onychomycosis. Mycoses 57(7):389–393. https://doi.org/10.1111/myc.12168
Jarratt M, Jones T, Kempers S, Rich P, Morton K, Nakamura N et al (2013) Luliconazole for the treatment of interdigital tinea pedis: A double-blind, vehicle-controlled study. Cutis 91(4):203–210
Uchida K, Nishiyama Y, Yamaguchi H (2004) In vitro antifungal activity of luliconazole (NND-502), a novel imidazole antifungal agent. J Infect Chemother 10(4):216–219. https://doi.org/10.1007/s10156-004-0327-1
Abastabar M, Rahimi N, Meis JF, Aslani N, Khodavaisy S, Nabili M et al (2016) Potent Activities of Novel Imidazoles Lanoconazole and Luliconazole against a Collection of Azole-Resistant and -Susceptible Aspergillus fumigatus Strains. Antimicrob Agents Chemother 60(11):6916–6919. https://doi.org/10.1128/AAC.01193-16
Shokoohi GR, Badali H, Mirhendi H, Ansari S, Rezaei-Matehkolaei A, Ahmadi B et al (2017) In Vitro Activities of Luliconazole, Lanoconazole, and Efinaconazole Compared with Those of Five Antifungal Drugs against Melanized Fungi and Relatives. Antimicrob Agents Chemother. https://doi.org/10.1128/AAC.00635-17
Koga H, Tsuji Y, Inoue K, Kanai K, Majima T, Kasai T et al (2006) In vitro antifungal activity of luliconazole against clinical isolates from patients with dermatomycoses. J Infect Chemother 12(3):163–165. https://doi.org/10.1007/s10156-006-0440-4
Taghipour S, Kiasat N, Shafiei S, Halvaeezadeh M, Rezaei-Matehkolaei A, Zarei Mahmoudabadi A (2018) Luliconazole, a new antifungal against Candida species isolated from different sources. J Mycol Med 28(2):374–378. https://doi.org/10.1016/j.mycmed.2017.11.004
Zargaran M, Taghipour S, Kiasat N, Aboualigalehdari E, Rezaei-Matehkolaei A, Zarei Mahmoudabadi A et al (2017) Luliconazole, an alternative antifungal agent against Aspergillus terreus. J Mycol Med 27(3):351–356. https://doi.org/10.1016/j.mycmed.2017.04.011
Todokoro D, Suzuki T, Tamura T, Makimura K, Yamaguchi H, Inagaki K et al (2019) Efficacy of luliconazole against broad-range filamentous fungi including Fusarium solani species complex causing fungal keratitis. Cornea 38(2):238–242. https://doi.org/10.1097/ICO.0000000000001812
Diekema DJ, Petroelje B, Messer SA, Hollis RJ, Pfaller MA (2005) Activities of available and investigational antifungal agents against Rhodotorula species. J Clin Microbiol 43(1):476–478. https://doi.org/10.1128/JCM.43.1.476-478.2005
Millar BC, Jiru X, Moore JE, Earle JA (2000) A simple and sensitive method to extract bacterial, yeast and fungal DNA from blood culture material. J Microbiol Methods 42(2):139–147. https://doi.org/10.1016/s0167-7012(00)00174-3
Clinical and Laboratory Standards Institute (2017) Reference method for broth dilution antifungal susceptibility testing of yeasts; CLSI standard M27, 4th edn. Clinical and Laboratory Standards Institute, Wayne
Gomez-Lopez A, Mellado E, Rodriguez-Tudela JL, Cuenca-Estrella M (2005) Susceptibility profile of 29 clinical isolates of Rhodotorula spp. and literature review. J Antimicrob Chemother 55(3):312–316. https://doi.org/10.1093/jac/dki020
Zaas AK, Boyce M, Schell W, Lodge BA, Miller JL, Perfect JR (2003) Risk of fungemia due to Rhodotorula and antifungal susceptibility testing of Rhodotorula isolates. J Clin Microbiol 41(11):5233–5235.
Krzyściak P, Macura AB (2010) Drug susceptibility of 64 strains of Rhodotorula sp. Wiad Parazytol 56(2):167–170
Clinical and Laboratory Standards institute (2008) Reference method for broth dilution antifungal susceptibility testing of yeasts. Third informational supplement. CLSI document M27-S3: (ISBN: 1-56238-667-0). In: Clinical and Laboratory Standards Institute, 940 West Vally Road, Suite 1400, Wayne. Pennsylvania, 19087 – 1898
Samonis G, Anatoliotaki M, Apostolakou H, Maraki S, Mavroudis D, Georgoulias V (2001) Transient fungemia due to Rhodotorula rubra in a cancer patient: case report and review of the literature. Infection 29(3):173–176. https://doi.org/10.1007/s15010-001-1066-1
Kiehn TE, Gorey E, Brown AE, Edwards FF, Armstrong D (1992) Sepsis due to Rhodotorula related to use of indwelling central venous catheters. Clin Infect Dis 14(4):841–846
Petrocheilou-Paschou V, Prifti H, Kostis E, Papadimitriou C, Dimopoulos MA, Stamatelopoulos S (2001) Rhodotorula septicemia: case report and minireview. Clin Microbiol Infect 7(2):100–102. https://doi.org/10.1046/j.1469-0691.2001.00203.x
Tuon FF, Costa SF (2008) Rhodotorula infection. A systematic review of 128 cases from literature. Rev Iberoam Micol 25(3):135–140. https://doi.org/10.1016/s1130-1406(08)70032-9
Ioannou P, Vamvoukaki R, Samonis G (2019) Rhodotorula species infections in humans: A systematic review. Mycoses 62(2):90–100. https://doi.org/10.1111/myc.12856
Koga H, Nanjoh Y, Makimura K, Tsuboi R (2009) In vitro antifungal activities of luliconazole, a new topical imidazole. Med Mycol 47(6):640–647. https://doi.org/10.1080/13693780802541518
Acknowledgements
We would like to thank the Infectious and Tropical Diseases Research Center, Health Research Institute, Ahvaz Jundishapur University of Medical Sciences for their support (OG: 9722).
Author information
Authors and Affiliations
Contributions
AZM: Study design, supervision, data interpretation, and manuscript editing. MG: Experimentation, Data collection, analysis, literature search, and manuscript writing. ST: Experimentation, Data collection, analysis, literature search, and manuscript writing. All authors read and approved the manuscript in the present state.
Corresponding author
Ethics declarations
Conflict of interest
No conflict of interest declared.
Ethical approval
This research related to micro-organisms and all tests was applied in vitro and no ethical approval was required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Gharaghani, M., Taghipour, S. & Zarei Mahmoudabadi, A. Molecular identification, biofilm formation and antifungal susceptibility of Rhodotorula spp.. Mol Biol Rep 47, 8903–8909 (2020). https://doi.org/10.1007/s11033-020-05942-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11033-020-05942-1