Abstract
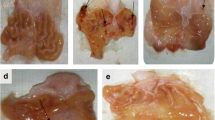
The use of inhibitors of gastric acid secretion (IGAS), especially proton pump inhibitors (PPI), has been associated with increased cardiovascular risk. While the mechanisms involved are not known, there is evidence supporting increased oxidative stress, a major activator of matrix metalloproteinases (MMP), as an important player in such effect. However, there is no study showing whether other IGAS such as histamine H2-receptor blockers (H2RB) cause similar effects. This study aimed at examining whether treatment with the H2RB ranitidine promotes oxidative stress resulting in vascular MMP activation and corresponding functional and structural alterations in the vasculature, as compared with those found with the PPI omeprazole. Male Wistar rats were treated (4 weeks) with vehicle (2% tween 20), omeprazole (10 mg/Kg/day; i.p.) or ranitidine (100 mg/Kg/day; gavage). Then the aorta was collected to perform functional, biochemical, and morphometric analysis. Both ranitidine and omeprazole increased gastric pH and oxidative stress assessed in situ with the fluorescent dye dihydroethidium (DHE) and with lucigenin chemiluminescence assay. Both IGAS augmented vascular activated MMP-2. These findings were associated with aortic remodeling (increased media/lumen ratio and number of cells/μm2). Both IGAS also impaired the endothelium-dependent relaxation induced by acetylcholine (isolated aortic ring preparation). This study provides evidence that the H2RB ranitidine induces vascular dysfunction, redox alterations, and remodeling similar to those found with the PPI omeprazole. These findings strongly suggest that IGAS increase oxidative stress and matrix metalloproteinase-2 activity leading to vascular remodeling, which helps to explain the increased cardiovascular risk associated with the use of those drugs.






Similar content being viewed by others
Data availability
Enquiries about data availability should be directed to the authors.
References
Berner BD, Conner CS, Sawyer DR, Siepler JK (1982) Ranitidine: a new H2-receptor antagonist. Clin Pharm 1:499–509
Sun S, Cui Z, Zhou M et al (2017) Proton pump inhibitor monotherapy and the risk of cardiovascular events in patients with gastro-esophageal reflux disease: a meta-analysis. Neurogastroenterol Motil 29:1–10. https://doi.org/10.1111/nmo.12926
Zhai Y, Ye X, Hu F et al (2022) updated insights on cardiac and vascular risks of proton pump inhibitors: a real-world pharmacovigilance study. Front Cardiovasc Med 9:767987. https://doi.org/10.3389/fcvm.2022.767987
Wu WT, Tsai CT, Chou YC et al (2019) Cardiovascular outcomes associated with clinical use of citalopram and omeprazole: a nationwide population-based cohort study. J Am Heart Assoc 8:1–7. https://doi.org/10.1161/JAHA.118.011607
Yepuri G, Sukhovershin R, Nazari-Shafti TZ et al (2016) Proton pump inhibitors accelerate endothelial senescence. Circ Res 118:e36–e42. https://doi.org/10.1161/CIRCRESAHA.116.308807
Shah NH, LePendu P, Bauer-Mehren A et al (2015) Proton pump inhibitor usage and the risk of myocardial infarction in the general population. PLoS ONE 10(6):e0124653. https://doi.org/10.1371/journal.pone.0124653
Lázaro AMP, Cristóbal C, Franco-Peláez JA et al (2017) Use of proton-pump inhibitors predicts heart failure and death in patients with coronary artery disease. PLoS ONE 12(1):e0169826. https://doi.org/10.1371/journal.pone.0169826
Ghebremariam YT, Lependu P, Lee JC et al (2013) Unexpected effect of proton pump inhibitors: elevation of the cardiovascular risk factor asymmetric dimethylarginine. Circulation 128:845–853. https://doi.org/10.1161/CIRCULATIONAHA.113.003602
Smith CA, Ebrahimpour A, Novikova L et al (1866) (2022) Esomeprazole covalently interacts with the cardiovascular enzyme dimethylarginine dimethylaminohydrolase: insights into the cardiovascular risk of proton pump inhibitors. Biochim Biophys Acta Gen Subj 8:130149. https://doi.org/10.1016/j.bbagen.2022.130149
Pinheiro LC, Montenegro MF, Amaral JH et al (2012) Increase in gastric pH reduces hypotensive effect of oral sodium nitrite in rats. Free Radic Biol Med 53:701–709. https://doi.org/10.1016/j.freeradbiomed.2012.06.001
Pinheiro LC, Oliveira-Paula GH, Portella RL et al (2016) Omeprazole impairs vascular redox biology and causes xanthine oxidoreductase-mediated endothelial dysfunction. Redox Biol 9:134–143. https://doi.org/10.1016/j.redox.2016.08.001
Liu N, Xu H, Sun Q et al (2021) The role of oxidative stress in hyperuricemia and xanthine oxidoreductase (XOR) inhibitors. Oxid Med Cell Longev. https://doi.org/10.1155/2021/1470380
Nogueira RC, Pinheiro LC, Sanches-Lopes JM et al (2021) Omeprazole induces vascular remodeling by mechanisms involving xanthine oxidoreductase and matrix metalloproteinase activation. Biochem Pharmacol 190:114633. https://doi.org/10.1016/j.bcp.2021.114633
Lambeth JD (2007) Nox enzymes, ROS, and chronic disease: an example of antagonistic pleiotropy. Free Radic Biol Med 43(3):332–347. https://doi.org/10.1016/j.freeradbiomed.2007.03.027
García-Redondo AB, Aguado A, Briones AM, Salaices M (2016) NADPH oxidases and vascular remodeling in cardiovascular diseases. Pharmacol Res 114:110–120. https://doi.org/10.1016/j.phrs.2016.10.015
Dries LS, Haefliger R, Seibert BS et al (2022) Cognition, oxidative stress and vitamin B12 levels evaluation on patients under long-term omeprazole use. J Pharm Pharmacol 74:547–555. https://doi.org/10.1093/jpp/rgab001
Marino ML, Fais S, Djavaheri-Mergny M et al (2010) Proton pump inhibition induces autophagy as a survival mechanism following oxidative stress in human melanoma cells. Cell Death Dis 1(10):e87. https://doi.org/10.1038/cddis.2010.67
Fontecha-Barriuso M, Martín-Sanchez D, Martinez-Moreno JM et al (2020) Molecular pathways driving omeprazole nephrotoxicity. Redox Biol 32:101464. https://doi.org/10.1016/j.redox.2020.101464
Mo C, Sun G, Wang YZ et al (2015) PPI versus histamine H2 receptor antagonists for prevention of upper gastrointestinal injury associated with low-dose aspirin: Systematic review and meta-analysis. PLoS ONE 10:1–13. https://doi.org/10.1371/journal.pone.0131558
Sanches-Lopes JM, Ferreira GC, Pinheiro LC et al (2020) Consistent gastric pH-dependent effects of suppressors of gastric acid secretion on the antihypertensive responses to oral nitrite. Biochem Pharmacol 177:113940. https://doi.org/10.1016/j.bcp.2020.113940
Batista RIM, Nogueira RC, Ferreira GC et al (2021) Antiseptic mouthwash inhibits antihypertensive and vascular protective effects of L-arginine. Eur J Pharmacol 907:174314. https://doi.org/10.1016/j.ejphar.2021.174314
Gonzaga NA, Awata doVale WMCGT et al (2018) Perivascular adipose tissue protects against the vascular dysfunction induced by acute ethanol intake: Role of hydrogen peroxide. Vascul Pharmacol 111:44–53. https://doi.org/10.1016/j.vph.2018.08.010
Mattos BR, Bonacio GF, Vitorino TR et al (2020) TNF-α inhibition decreases MMP-2 activity, reactive oxygen species formation and improves hypertensive vascular hypertrophy independent of its effects on blood pressure. Biochem Pharmacol 180:114121. https://doi.org/10.1016/j.bcp.2020.114121
Ceron CS, Castro MM, Rizzi E et al (2010) Spironolactone and hydrochlorothiazide exert antioxidant effects and reduce vascular matrix metalloproteinase-2 activity and expression in a model of renovascular hypertension. Br J Pharmacol 160:77–87. https://doi.org/10.1111/j.1476-5381.2010.00678.x
Rizzi E, Amaral JH, Guimarães DA et al (2019) Nitrite treatment downregulates vascular MMP-2 activity and inhibits vascular remodeling in hypertension independently of its antihypertensive effects. Free Radic Biol Med 130:234–243. https://doi.org/10.1016/j.freeradbiomed.2018.11.002
Khawaja M, Thakker J, Kherallah R et al (2022) Antacid therapy in coronary artery disease and heart failure: proton pump inhibitors vs H2 receptor blockers. Cardiovasc Drugs Ther. https://doi.org/10.1007/s10557-022-07358-4
Tseng HJ, Cheng CM, Tsai SJ et al (2021) Proton pump inhibitor exposure and acute myocardial infarction risk: a nested cohort study. Cardiovasc Toxicol 21:444–450. https://doi.org/10.1007/s12012-021-09637-2
Lo CH, Ni P, Yan Y et al (2022) Association of proton pump inhibitor use with all-cause and cause-specific mortality. Gastroenterology 163(4):852-861.e2. https://doi.org/10.1053/j.gastro.2022.06.067
Vial T, Goubier C, Bergeret A et al (1991) Side effects of ranitidine. Drug Saf 6(2):94–117. https://doi.org/10.2165/00002018-199106020-00002
Leary PJ, Tedford RJ, Bluemke DA et al (2016) Histamine H 2 receptor antagonists, left ventricular morphology, and heart failure risk the MESA study. J Am Coll Cardiol 67(13):1544–1552. https://doi.org/10.1016/j.jacc.2016.01.045
Zhang J, Cai WK, Zhang Z et al (2018) Cardioprotective effect of histamine H2 antagonists in congestive heart failure. Medicine (United States) 97(15):e0409. https://doi.org/10.1097/MD.0000000000010409
Corsonello A, Lattanzio F (2019) Cardiovascular and non-cardiovascular concerns with proton pump inhibitors: Are they safe? Trends Cardiovasc Med 29(6):353–360. https://doi.org/10.1016/j.tcm.2018.10.008
Kieboom BCT, Kiefte-De Jong JC, Eijgelsheim M et al (2015) Proton pump inhibitors and hypomagnesemia in the general population: a population-based cohort study. Am J Kidney Dis 66:775–782. https://doi.org/10.1053/j.ajkd.2015.05.012
Kamiya C, Odagiri K, Hakamata A et al (2021) Omeprazole suppresses endothelial calcium response and eNOS Ser1177 phosphorylation in porcine aortic endothelial cells. Mol Biol Rep 48:5503–5511. https://doi.org/10.1007/s11033-021-06561-0
Costarelli L, Giacconi R, Malavolta M et al (2017) Different transcriptional profiling between senescent and non-senescent human coronary artery endothelial cells (HCAECs) by Omeprazole and Lansoprazole treatment. Biogerontology 18:217–236. https://doi.org/10.1007/s10522-016-9675-3
Luo T, Chen B, Zhao Z et al (2013) Histamine H2 receptor activation exacerbates myocardial ischemia/reperfusion injury by disturbing mitochondrial and endothelial function. Basic Res Cardiol 108(3):342. https://doi.org/10.1007/s00395-013-0342-4
Hekimian G, Cijte S, Van Sande J et al (1992) Hz receptor-mediated responses of aortic endothelial cells to histamine. Am J Physiol 262(1):H220–H224. https://doi.org/10.1152/ajpheart.1992.262.1.H220
Kishi F, Nakaya Y, Ito S (1998) Histamine H2-receptor-mediated nitric oxide release from porcine endothelial cells. J Cardiovasc Pharmacol 32:177–182. https://doi.org/10.1097/00005344-199808000-00002
Biswas K, Bandyopadhyay U, Chattopadhyay I et al (2003) A novel antioxidant and antiapoptotic role of omeprazole to block gastric ulcer through scavenging of hydroxyl radical. J Biol Chem 278:10993–11001. https://doi.org/10.1074/jbc.M210328200
Abed MN, Alassaf FA, Jasim MHM et al (2020) Comparison of antioxidant effects of the proton pump-inhibiting drugs omeprazole, esomeprazole, lansoprazole, pantoprazole, and rabeprazole. Pharmacology 105:645–651. https://doi.org/10.1159/000506232
Patil AS, Singh AD, Mahajan UB et al (2019) Protective effect of omeprazole and lansoprazole on β-receptor stimulated myocardial infarction in Wistar rats. Mol Cell Biochem 456:105–113. https://doi.org/10.1007/s11010-019-03494-y
Kohler JE, Blass AL, Liu J et al (2010) Antioxidant pre-treatment prevents omeprazole-induced toxicity in an in vitro model of infectious gastritis. Free Radic Biol Med 49:786–791. https://doi.org/10.1016/j.freeradbiomed.2010.05.034
Patel A, Zhang S, Shrestha AK et al (2016) Omeprazole induces heme oxygenase-1 in fetal human pulmonary microvascular endothelial cells via hydrogen peroxide-independent Nrf2 signaling pathway. Toxicol Appl Pharmacol 311:26–33. https://doi.org/10.1016/j.taap.2016.10.002
Kondru SK, Potnuri AG, Allakonda L, Konduri P (2018) Histamine 2 receptor antagonism elicits protection against doxorubicin-induced cardiotoxicity in rodent model. Mol Cell Biochem 441:77–88. https://doi.org/10.1007/s11010-017-3175-x
Potnuri AG, Allakonda L, Appavoo A et al (2018) Association of histamine with hypertension-induced cardiac remodeling and reduction of hypertrophy with the histamine-2-receptor antagonist famotidine compared with the beta-blocker metoprolol. Hypertens Res 41:1023–1035. https://doi.org/10.1038/s41440-018-0109-2
Potnuri AG, Allakonda L, Saheera S (2021) Involvement of histamine 2 receptor in alpha 1 adrenoceptor mediated cardiac hypertrophy and oxidative stress in H9c2 cardio myoblasts. J Cardiovasc Transl Res 14:184–194. https://doi.org/10.1007/s12265-020-09967-6
Sena CM, Leandro A, Azul L et al (2018) Vascular oxidative stress: impact and therapeutic approaches. Front Physiol 9:1668. https://doi.org/10.3389/fphys.2018.01668
Ceron CS, Rizzi E, Guimarães DA et al (2013) Nebivolol attenuates prooxidant and profibrotic mechanisms involving TGF-β and MMPs, and decreases vascular remodeling in renovascular hypertension. Free Radic Biol Med 65:47–56. https://doi.org/10.1016/j.freeradbiomed.2013.06.033
Castro MM, Rizzi E, Rodrigues GJ et al (2009) Antioxidant treatment reduces matrix metalloproteinase-2-induced vascular changes in renovascular hypertension. Free Radic Biol Med 46:1298–1307. https://doi.org/10.1016/j.freeradbiomed.2009.02.011
Marçal DMO, Rizzi E, Martins-Oliveira A et al (2011) Comparative study on antioxidant effects and vascular matrix metalloproteinase-2 downregulation by dihydropyridines in renovascular hypertension. Naunyn Schmiedebergs Arch Pharmacol 383:35–44. https://doi.org/10.1007/s00210-010-0573-y
Grote K, Flach I, Luchtefeld M et al (2003) Mechanical stretch enhances mRNA expression and proenzyme release of matrix metalloproteinase-2 (MMP-2) via NAD(P)H oxidase-derived reactive oxygen species. Circ Res 92(11):e80–e86. https://doi.org/10.1161/01.res.0000077044.60138.7c
Shin MH, Moon YJ, Seo JE et al (2008) Reactive oxygen species produced by NADPH oxidase, xanthine oxidase, and mitochondrial electron transport system mediate heat shock-induced MMP-1 and MMP-9 expression. Free Radic Biol Med 44:635–645. https://doi.org/10.1016/j.freeradbiomed.2007.10.053
Wei S, Isagawa T, Eguchi M et al (2020) Febuxostat, a xanthine oxidase inhibitor, decreased macrophage matrix metalloproteinase expression in hypoxia. Biomedicines 8:1–13. https://doi.org/10.3390/biomedicines8110470
Rodríguez-Rovira I, Arce C, De Rycke K et al (2022) Allopurinol blocks aortic aneurysm in a mouse model of Marfan syndrome via reducing aortic oxidative stress. Free Radic Biol Med 193:538–550. https://doi.org/10.1016/j.freeradbiomed.2022.11.001
Prado AF, Pernomian L, Azevedo A et al (2018) Matrix metalloproteinase-2-induced epidermal growth factor receptor transactivation impairs redox balance in vascular smooth muscle cells and facilitates vascular contraction. Redox Biol 18:181–190. https://doi.org/10.1016/j.redox.2018.07.005
Brown IAM, Diederich L, Good ME et al (2018) Vascular smooth muscle remodeling in conductive and resistance arteries in hypertension: VSMC in hypertension. Arterioscler Thromb Vasc Biol 38:1969–1985. https://doi.org/10.1161/ATVBAHA
Gao Z, Karfunkle M, Ye W et al (2021) In vitro analysis of N -nitrosodimethylamine (NDMA) formation from ranitidine under simulated gastrointestinal conditions. JAMA Netw Open 4:e2118253. https://doi.org/10.1001/jamanetworkopen.2021.18253
White CM (2021) Ranitidine’s N -nitrosodimethylamine problem may be tip of the iceberg. JAMA Netw Open 4:e2035158. https://doi.org/10.1001/jamanetworkopen.2020.35158
Florian J, Matta MK, DePalma R et al (2021) Effect of oral ranitidine on urinary excretion of N -nitrosodimethylamine (NDMA). JAMA 326:240. https://doi.org/10.1001/jama.2021.9199
Funding
This work was supported by Fundação de Aparo a Pesquisa do Estado de São Paulo (FAPESP Grant number 2014–23946-0), Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq - Grant number 406442/2022-3) and Coordenação de Aperfeiçoamento de Pessoal de Nível Superior—Brasil (CAPES)—Finance Code 001.
Author information
Authors and Affiliations
Contributions
RCN and JMS-L: Contributed equally to this article in Conceptualization, Data curation, Formal analysis, Methodology, Writing. [GHO-P]: Conceptualization, Data curation, Formal analysis, Methodology, Writing. JET-S: Conceptualization, Data curation, Formal analysis, Funding acquisition, Project administration, Resources, Supervision, Writing. All authors read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Ethical approval
The present study and experimental procedures complied with the ARRIVE guidelines and were in accordance with the National Research Council's Guide for the Care and Use of Laboratory Animals. The study was approved by the Animal Care and Use Committee of Ribeirao Preto Medical School—University of Sao Paulo (protocol code 171–2016).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Nogueira, R.C., Sanches-lopes, J.M., Oliveira-Paula, G.H. et al. Inhibitors of gastric acid secretion increase oxidative stress and matrix metalloproteinase-2 activity leading to vascular remodeling. Mol Cell Biochem (2024). https://doi.org/10.1007/s11010-023-04921-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11010-023-04921-x