Abstract
Transforming growth factor beta (TGF-β) is a ubiquitously distributed cytokine known to contribute to the pathogenesis of numerous pathological processes. The aim of this study was to measure serum concentrations of TGF-β1 in severely ill COVID-19 patients and to analyze its relationship with selected hematological and biochemical parameters and with the disease outcome. The study population included 53 COVID-19 patients with severe clinical expression of the disease and 15 control subjects. TGF-β1 was determined in serum samples and supernatants from PHA-stimulated whole blood cultures using ELISA assay. Biochemical and hematological parameters were analyzed using standard accepted methods. Our results showed that serum levels of TGF-β1 in COVID-19 patients and controls correlate with the platelet counts. Also, positive correlations of TGF-β1 with white blood cell and lymphocyte counts, platelet-to-lymphocyte (PLR) ratio, and fibrinogen level were shown, while negative correlations of this cytokine with platelet distribution width (PDW), D-dimer and activated partial thromboplastin time (a-PTT) values in COVID-19 patients were observed. The lower serum values of TGF-β1 were associated with the unfavorable outcome of COVID-19. In conclusion, TGF-β1 levels were strongly associated with platelet counts and unfavorable disease outcome of severely ill COVID-19 patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Coronavirus disease 2019 (COVID-19) caused by severe acquired respiratory syndrome coronavirus 2 (SARS-CoV-2) is an ongoing global health crisis. Even though most COVID-19 patients have mild respiratory illness, approximately 15%–20% patients become seriously ill and require hospitalization due to pneumonia and/or systemic complications [1]. The pathophysiology of severe COVID-19 disease involves excessive release of inflammatory mediators leading to acute respiratory distress syndrome (ARDS) and systemic inflammation, which appears to be potentially life-threatening [2]. The plasma cytokine levels analyzed in the majority of studies show higher amounts of proinflammatory cytokines: interleukin 1 (IL-1), interleukin 6 (IL-6), interleukin 12 (IL-12), interleukin 17 (IL-17), interferon gamma (IFN-γ), and tumor necrosis factor alpha (TNF-α) [3,4,5]. The increased concentrations of interleukin 4 (IL-4) and interleukin 10 (IL-10) that suppress inflammation were also observed [6].
The transforming growth factor beta (TGF-β) is known to influence the immune cells’ development, differentiation, tolerance induction and homeostasis. Accordingly, the balance of pleiotropic effects of TGF-β in different immune cells could contribute to the establishment of either immunity or tolerance. It was shown earlier that TGF-β could contribute to the pathogenesis of numerous pathological processes. The role of TGF-β1 in disease course and outcome in COVID-19 patients is still insufficiently examined. In patients with ARDS it was shown that TGF-β1 accumulates in lungs and plasma during the early phase of the infection [7,8,9]; later, it induces a shift to IgA2 production and TGF-β-dominated chronic immune response and fibrosis [10]. In our previous publication we observed correlation of serum TGF-β1 levels with platelet counts in patients with differentiated thyroid cancers and control subjects [11]. The aim of this study was to investigate serum concentrations of TGF-β1 in severely ill COVID-19 patients, as well as its relationship with selected hematological and biochemical parameters and with the intrahospital disease outcome. Since previously published data indicate association of thrombocytopenia with severe COVID-19 infection and/or the unfavorable outcome [12,13,14], and bearing in mind the relation of TGF-β1 levels with platelet counts shown in our previous study [11] , we hypothesized that the concentration of anti-inflammatory cytokine TGF-β1 might be associated with the platelet count and could possibly influence the outcome in severely ill COVID-19 patients. Also, serum level of TGF-β1 was analyzed in relation to its concentration in supernatants obtained from whole blood cultures after unspecific in vitro stimulation.
Materials and methods
Study population
The study was planned according to ethical guidelines following the Declaration of Helsinki. The institutional review committee approved our study protocol (number 01/21-138) according to local biomedical research regulations. All patients and control subjects gave informed consent prior to enrollment in the investigation.
The study population included 53 COVID-19 patients (33 males and 20 females) mean age 67.9 ± 12.5 years; recruited from the University Clinical Center Kragujevac during February and March 2021. Inclusion criteria were: SARS-CoV-2 infection confirmed by real-time polymerase chain reaction (RT-PCR), hospitalization and severe clinical expression of the disease, radiographically proven pneumonia needing supplemental oxygen provided by oxygen mask, High Flow oxygen therapy or Non-Invasive ventilation, but not too advanced to require intubation and invasive mechanical ventilation at the time of blood collection. Besides oxygen therapy, all patients received methylprednisolone, low-molecular weight heparin (LMWH), antibiotics and other supportive therapy. None of the patients had coagulation disorders, chronic inflammatory, autoimmune and malignant diseases, or other conditions that could affect the tested parameters.
Fifteen healthy subjects with a negative antigenic test for coronavirus (10 males and 5 females) of mean age 62.8 ± 11.4 years were included in the investigation as a control group. The control subjects had no coagulation disorders, chronic inflammatory, autoimmune and malignant diseases. Controls subjects were not vaccinated against SARS-CoV-2 before enrolment (February 2021).
After venipuncture, three 5 mL blood samples (one without added anticoagulants) were taken from each patient and each control subject. Approximately 30 min after venipuncture, serum was separated by centrifugation of the sample without anticoagulants at 2000 rpm for 15 min, a part was used for biochemical analyzes, and a part is immediately frozen and stored at − 20 °C until TGF-β measurement. The samples containing anticoagulant sodium citrate were used for hematological analyses, while samples containing heparin were used for whole blood cultures in vitro.
Whole blood culture
Whole blood culture was performed as described earlier [15]. Heparinized whole blood (0.5 ml per subject) was added to 2 ml RPMI based complete medium containing fetal bovine serum, L-glutamine and phytohemagglutinin (PHA) (GIBCO TMPB-MAX™ karyotyping medium, Invitrogen, California, USA) and incubated at 37 °C for 48 h. The supernatant was harvested by centrifugation (2000 rpm for 12 min) and then stored at − 20 °C until required.
Determination of biochemical parameters
The biochemical parameters were analyzed using standard accepted methods in Laboratory diagnostic service of University Clinical Center Kragujevac. Serum concentrations of C-reactive protein (CRP), procalcitonin, interleukin 6 (IL-6) and ferritin, were measured using commercially available enzymatic reagents adapted to an autoanalyser Oly AU 680 (Beckman Coulter Inc. Brea, USA) for CRP and ferritin, and Cobas e 411 chemical analyzer (Roche diagnostics GmbH, Mannheim, Germany) for procalcitonin and IL-6. The reference ranges were as follows: CRP < 5 mg/L; procalcitonin 0.5‒2.0 ng/mL; IL-6 < 7 pg/mL and ferritin 20‒300 μg/L.
Determination of hematological parameters
The automated DxH 800 Hematology Analyzer (Beckman Coulter, Inc. Brea, USA) was used for the assessment of hematological parameters: white blood cell (WBC) count (3.70‒10.0 × 109/L), neutrophil granulocytes (2.10‒6.50 × 109/L), lymphocytes (1.2‒3.4 × 109/L) and platelets (135‒450 × 109/L), mean platelet volume, MPV (6.8‒10.4 fL) and platelet distribution width, PDW (12.0–16.5). Blood coagulation parameters: a-PTT, thrombin time (TT), D-dimer and fibrinogen were determined by ACL TOP 350CTS (Beckman Coulter Inc. Brea, USA). The reference ranges were as follows: a-PTT 25‒35 s; TT 9.1‒12.1 s, D-dimer < 0.50 μg/mL; and fibrinogen 2‒5 g/L. Absolute platelet count (× 109 cells/L) divided by absolute lymphocyte count (× 109 cells/L) gives PLR.
TGF-β1 measurement
TGF-β1 was determined in serum samples and supernatants from PHA-stimulated whole blood cultures using the Human/Mouse TGF beta 1 uncoated ELISA (Thermo Fisher Scientific) ELISA kit, Catalog No. 88-8350-88 according to the manufacturer’s instructions. To activate latent TGF-β1 to the immunoreactive form, we used solutions for acid activation and neutralization. The background level of TGF-β1 in control medium was determined and subtracted from the results for samples of PHA-stimulated whole blood culture supernatants.
Statistical analysis
Statistical analysis was carried out using the commercial SPSS version 18.0 for Windows. The Kolmogorov–Smirnov test was performed to verify the distribution of certain variables. Differences between two independent groups were evaluated by Student’s t-test (for variables with normal distribution), or the Mann–Whitney test (for variables without normal distribution). The linear correlation test and determination of the Pearson/Spearman coefficient were applied to estimate association between tested variables. The impact of the analyzed variables on disease outcome was tested by Binary logistic regression test. A probability (p) value less than 0.05 was considered the threshold for statistical significance.
Results
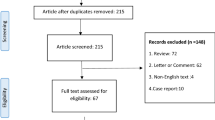
We analyzed the concentration of total (inactive + active) TGF-β1 in COVID-19 patients and in control subjects. Also, we studied a relation of TGF-β1 values with platelet counts as well as with hematological and biochemical parameters in COVID-19 patients. Finally, we tested if TGF-β1 values could be a prognostic factor in COVID-19 patients. The results are presented in Tables 1 and 2 and Figs. 1, 2, 3, 4 and 5.
Correlation analysis between selected hematological and biochemical parameters in COVID-19 patients; TGF-β1 transforming growth factor beta 1, PLT platelets, WBC white blood cells, Ne neutrophils, Ly lymphocytes, CRP C-reactive protein, IL-6 interleukin 6, PCT procalcitonin, D-dim D-dimer, aPTT activated partial thromboplastin time, Fibr fibrinogen, Fer Ferritin
Although the sample size was relatively small, we divided COVID-19 patients into two groups: males (n = 32) and females (n = 21). There were no significant differences between males and females in platelet counts (262.91 ± 208.12 × 109/L vs. 216.43 ± 184.88 × 109/L, p = 0.300). But, the age of COVID-19 patients correlated negatively with the platelet counts (r = − 0.322, p = 0.019).
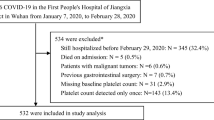
On the basis of platelet counts COVID-19 patients were divided into three groups, group 1 with decreased platelet count, group 2 with normal platelet count and group 3 with the increased platelet count. Table 1 shows the selected hematological and biochemical characteristics of our COVID-19 patients.
The hematological parameters and CRP values in the control group (15 subjects) were within the reference ranges, as follows: platelet counts (242.3 ± 45.6 × 109/L, range 177.0–306.0 × 109/L), WBC counts (6.9 ± 1.2 × 109/L, range 5.3–9.2 × 109/L), neutrophil granulocyte counts (3.8 ± 0.9 × 109/L, range 2.4–4.7 × 109/L), lymphocyte counts (2.2 ± 0.5 × 109/L, range 1.4–3.1 × 109/L) and CRP values (< 5 mg/L).
The vast majority (47/53, 88.7%) of hospitalized patients with COVID-19 had comorbidities. In relation to diagnoses, most frequent was hypertension (39 patients), diabetes mellitus type II (15 patients), arrhythmia (11 patients), status post myocardial infarction (6 patients), status post cerebrovascular stroke (5 patients), asthma (4 patients) and chronic obstructive pulmonary disease (3 patients).
Figure 1 shows platelet counts (a) and TGF-β1 concentration (b) measured in blood/serum samples of control subjects and three groups of COVID-19 patients. A statistically significant difference in platelet counts between the group of control subjects and group 1 of COVID-19 patients (242.3±45.6 vs 89.8±34.2 x 109/L, p<0.001) as well as between control group and group 3 of patients (242.3±45.6 vs 552.8±86.0 x 109/L, p<0.001) are shown, while the difference between control group and group 2 of COVID-19 patients was not significant (242.3±45.6 vs 293.0±91.5 x 109/L, p=0.091).
Also, statistically significant differences in serum levels of TGF-β1 between the group of control subjects and group 1 (30.4 ± 8.8 vs 13.1 ± 4.7 ng/mL, p < 0.001) as well as between control group and group 3 of COVID-19 patients (30.4 ± 8.8 vs 45.6 ± 14.4 ng/mL, p = 0.002) were shown, while difference between control group and group 2 of COVID-19 patients was not significant (30.4 ± 8.8 vs 29.6 ± 10.9 ng/mL, p = 0.845). There were no significant differences between males and females in TGF-β1 levels (26.03 ± 18.16 ng/mL vs. 23.28 ± 14.76 ng/mL, p = 0.785).
Correlation analysis showed a strong positive association between TGF-β1 concentrations in patients’ serum and platelet counts (r = 0.861, p < 0.001) (Fig. 2). There was significant correlation between platelet counts and TGF-β1 levels in both male (r = 0.878, p < 0.001) and female (r = 0.674, p = 0.001) COVID-19 patients. Besides, a weak positive correlation of serum TGF-β1 values with WBC counts (r = 0.367, p = 0.007), lymphocyte counts (r = 0.290, p = 0.048), PLR ratios (r = 0.387, p = 0.007) and fibrinogen levels (r = 0.339, p = 0.040) were shown. But, a negative correlation with PDW (r = − 0.469, p < 0.001), D-dimer (r = − 0.460, p = 0.004) and a-PTT (r = − 0.338, p = 0.020) values were estimated. When the patients were divided on the basis of D-dimer values, there were significant differences in platelet counts (294.71 ± 192.94 × 109/L vs 98.17 ± 27.44 × 109/L, p = 0.011) and TGF-β1 concentrations (28.77 ± 16.69 ng/mL vs 13 ± 3.74 ng/mL, p < 0.001) between the group of patients with the D-dimer below and above 2 μg/mL.
Also, serum TGF-β1 concentrations were positively correlated with platelet counts in controls (r = 0.591, p = 0.033).
Figure 3 shows the relationship between TGF-β1 values and platelet counts in COVID-19 patients. During the recruitment of COVID-19 patients in this study, we selected a subgroup of 19 patients with the mean value of platelets within the reference range, with no statistically significant differences to control subjects (297.6 ± 131.9 × 109/L vs 242.3 ± 45.6 × 109/L, p = 0.276). In the three COVID-19 patients platelet counts were decreased, in three patients the platelet counts were increased, and in the rest of 13 patients the platelet counts were within the reference range. The TGFβ1 concentrations were measured in supernatants from PHA-stimulated whole blood cultures of selected COVID-19 patients and compared to control subjects. There were significantly higher supernatant levels of TGF-β1 in controls than in COVID-19 patients (963.0 ± 266.0 vs 742.6 ± 327.7 pg/mL, p = 0.037) (Fig. 4a). Besides, there was a strong positive correlation between the platelet counts and TGF-β1 values measured in the supernatant samples of COVID-19 patients (r = 0.837, p < 0.001) as well as between serum and supernatant values of TGF-β1 from the same patients (r = 0.852, p < 0.001) (Fig. 4b).
In our group of 53 patients with severe COVID-19, 32 (60.4%) patients survived and 21 (39.6%) did not survive. Figure 5 shows a mean platelet count (304.75 ± 198.81 vs. 152.67 ± 163.57 × 109/L, p = 0.002) and b TGF-β1 concentration (29.53 ± 17.20 vs. 17.95 ± 13.80 ng/mL, p = 0.006) in COVID-19 survivors and non-survivors.
Using binary logistic regression, we analyzed the possible influence of serum values of TGF-β1, platelet counts and other parameters on the disease outcome (Table 2). We found that TGF-β1 level (β = − 0.52, p = 0.022), platelet counts (β = − 0.005, p = 0.011) and lymphocyte counts (β = − 1.773, p = 0.011) negatively correlated with the death outcome, while PDW (β = 0.936, p = 0.015), IL-6 levels (β = 0.036, p = 0.036), age (β = 0.110, p = 0.003) and comorbidities (β = 0.198, p = 0.029) positively correlated with the death outcome. It means that the lower platelet counts, lower lymphocyte counts and lower total TGF- β1, with the higher PDW, higher IL-6 values, older age and comorbidities were associated with unfavorable outcome of the disease.
There was no significant difference in the death outcome between males and females (12/32 vs. 9/21, χ2 = 0.152, p = 0.697). The negative influence of platelet counts (β = − 0.005, p = 0.046) and TGF-β1 levels (β = − 0.062, p = 0.041) on unfavorable outcome in male patients was shown. But, negative associations of the death outcome with platelet counts (β = − 0.288, p = 0.122) and TGF-β1 levels (β = − 0.035, p = 0.321) in female patients was not significant, possibly due to the small sample size.
Discussion
The aim of this study was to investigate serum concentrations of TGF-β1 in severely ill COVID-19 patients, as well as its relationship with selected hematological and biochemical parameters, and with the disease outcome. Also, serum level of TGF-β1 was analyzed in relation to its concentration in supernatants obtained from whole blood cultures after unspecific in vitro stimulation. Our main results are: (1) serum levels of TGF-β1 in COVID-19 patients strongly correlate with the platelet counts, (2) positive correlations of lower intensity were also shown with WBC and lymphocyte counts, PLR ratio, as well as with fibrinogen level, while negative correlations were observed with PDW ratio, D-dimer and a-PTT values, (3) concentrations of TGF-β1 in supernatants from whole blood culture in vitro correlate with the serum levels of TGF-β1, 4) lower serum values of TGF-β1 are associated with the unfavorable outcome of COVID-19.
TGF-β1 might influence differentiation and/or function of almost all cells of the innate and acquired immunity. The role of TGF-β in the pathogenesis of COVID-19 infection is insufficiently elucidated. It was proposed that SARS CoV-2 infection is associated with the release of TGF-β from immune cells such as neutrophils and injured cells [9]. TGF-β1 accumulates in lungs and plasma during the early phase of the infection leading to ARDS [7,8,9], while, later it induces a shift to IgA2 production and TGF-β-dominated chronic immune response and fibrosis [10]. The serum concentrations of TGF-β1 in COVID-19 patients with pneumonia, as well as its’ relationships with hematological and biochemical parameters are insufficiently analyzed so far. Our results unequivocally showed that TGF-β1 level measured in serum samples of COVID-19 patients depends on platelet counts. This result is not surprising given that platelets are the main source/reservoir of circulating TGF-β1 containing 40–100 times more of this cytokine than other cells [16], and that about 40% of TGF-β in peripheral blood/plasma is secreted by platelets, reviewed in Karolczak and Watala [17]. Besides the storage of TGF-β1 in alpha granules [18], TGF-β1 is also present on the outer surface of the platelet membrane [16, 19]. In our previous publication we observed the correlation of serum levels of TGF-β1 with platelet counts in patients with differentiated thyroid cancers and control subjects [11]. Apart from the fact that platelets are the main source of TGF-β, and consequently can significantly affect TGF-β1 concentration in the blood, there is a reverse possibility that the level of TGF-β affects the number of platelets [20]. Accordingly, an increased TGF-β release during the progression of disease could contribute to a decrease in platelet count, and consequently, a decrease in the amount of TGF-β stored in platelets. Our results are in agreement with the theoretical consideration of Chen, who proposed that concentration of inactive TGF-β1 in COVID-19 patients would be diminished because of its activation in inflamed areas of lungs [8]. But, our results are not consistent with the findings of other authors who showed that TGF-β1 level was lower in mild patients than both moderate and severe groups of COVID-19 patients [10]. In one study it was observed that TGF-β1 levels were similar in subgroups of COVID-19 patients at first presentation with those in the control group [21], which is not necessarily in disagreement with the results of our study. Namely, our group of COVID-19 patients with normal platelet counts had TGF-β1 values comparable to controls.
The platelets are powerful multifunctional cells involved in many processes, beyond their traditional role in haemostasis. For example, in the presence of a foreign pathogenic agent, platelets become activated and release their granule contents, which include several pro-coagulant molecules, cytokines/chemokines, growth factors, adhesion proteins, and microbicidal proteins [22,23,24,25,26]. Platelet alpha granules contain P-selectin which might mediate adhesion of platelets to monocytes, neutrophils and lymphocytes, resulting in the formation of platelet–leukocyte complexes, with the important role in thromboinflammation [27]. Circulating platelets in COVID-19 pneumonia demonstrate a specific phenotypic and functional profile that is consistent with that of procoagulant platelets [27]. In a recently published paper Tafazoli et al. proposed the term “thrombocytopathy” to explain the involvement of platelets in COVID-19, the unpredictable pathologic alterations of the function, morphology and number of platelets, caused by different factors and with a variety of presentations [28].
In this study we analyzed several platelet related parameters: platelet counts, MPV, PDW and PLR. Based on the platelet counts, COVID-19 patients were divided into three groups (with decreased, normal and increased platelet counts). In patients with COVID-19 included in this study more than half of patients had thrombocytopenia. The decrease of platelet counts in COVID-19 patients could be multifactorial: destruction of platelets by the immune system, more platelets get consumed due to accumulation in the lungs and/or infection of bone marrow [29]. Our results are in agreement with literature data showing the decrease in platelet counts in patients with severe and critical COVID-19 [30]. But our study also included subgroups of patients with normal and increased platelet counts. Thrombocytosis observed in this study might be a result of therapy with methylprednisolone. As suggested, corticosteroids are beneficial for COVID-19 patients if they are administrated at an optimal timing, optimal dosage, and according to the right schedule [31]. Hu et al. have evaluated the effects of methylprednisolone in the treatment of COVID-19 patients [32]. They showed that not only the number of lymphocytes but also the platelet count is significantly increased after corticosteroid therapy [32]. Moreover, platelet count remained stable, and the symptoms of pneumonia improved gradually [31,32,33]. Our results indicate that TGF-β1 levels follow the platelet counts and that both are positively correlated with the disease outcome.
Also, our results show a significant difference in PLR between COVID-19 patients and controls, as well as between three subgroups of patients. As expected, the highest PLR was observed in COVID-19 patients with thrombocytosis. Even though platelet counts and lymphocyte counts, individually, negatively correlated with the unfavorable outcome, the association of PLR values with the death outcome in our COVID-19 patients was not shown. Also, no association of MPV with disease outcome was observed. Our results are not in agreement with the results of Güçlü et al., who showed an increase in mortality by 1.76 times for every unit increase in mean platelet volume [29, 34]. If the platelet counts decreases, it leads to an increase in platelet production and to variations in the platelet size and consequently to PDW increases [34, 35]. In this study, a positive association of PDW with unfavorable outcome in our COVID-19 patients was observed, which is in agreement with the results of other studies in COVID-19 patients and patients with sepsis [34, 35]. The results of our study support the evidence of PLR as one of the independent factors predicting mortality in COVID-19 patients [36]. Our results indicated that platelet counts positively correlated with WBC counts, neutrophil granulocyte counts and lymphocyte counts, but no correlations with CRP, procalcitonin and IL-6 values were observed. On the other hand, lymphocyte counts negatively correlated with the CRP and procalcitonin values (higher inflammation is associated with lower lymphocyte count). A significant association between disease severity and elevation in blood parameters in majority of published studies is observed. The WBC and neutrophil granulocyte counts were significantly increased, while lymphocyte counts are decreased in the critically ill COVID-19 patients, compared to patients with milder condition [36]. Although WBC and neutrophil counts were increased in our study group, the associations with the unfavorable outcome were not found. Namely, our results indicated that death outcome was associated with the lower platelet and lymphocyte counts, lower TGF-β1 values, but higher PDW and IL-6 values, older age and comorbidities. According to the results of this study, TGF-β1 might be added to the group of biomarkers which are useful in predicting the severity and the outcome of COVID-19.
Lokwani and coworkers suggested that biochemical markers like CRP, LDH and D-dimer could be used to differentiate severe patients from non-severe patients of COVID-19 disease [37]. In our study with the severe COVID-19 patients only the levels of IL-6 were positively associated with the unfavorable outcome. But, when the patients were divided according to the D-dimer levels, there were significant differences in platelet counts and TGF-β1 concentration between the group of patients with the D-dimer below and above the 2 μg/mL. Moreover, correlation analysis showed negative associations of D-dimer values with the platelet counts and TGF-β1 values, indicating the interrelationship of all three markers in severely ill COVID-19 patients.
In this paper, we measured TGF-β1 levels in serum samples of COVID-19 patients, given that the TGF-β1 levels in serum and platelet-poor plasma were shown to be comparable [38, 39]. Besides, in subgroup of COVID-19 patients we also measured the concentrations of TGF-β1 in supernatants obtained from whole blood cultures in vitro. The concentrations of TGF-β1 measured in supernatants of these patients correlated with the serum values. Since strong correlation of TGF-β1 values with platelet counts was shown, we cannot exclude the possibility that at least a part of this cytokine was released during the clotting process [40]. In either case, our results indicate that the blood level of TGF beta in patients with thrombocytopenia is lower, or that their platelets have a lower ability to release this inhibitory cytokine. The low platelet count was associated with unfavorable outcome in patients with sepsis [41, 42], and COVID-19 patients as well [43]. This could be the consequence of disturbances in the coagulation process, but also of the decrease of TGF-β1 level. TGF-β1 is one of the most important anti-inflammatory cytokines, which controls the magnitude and the type of immune response against microbes. It might mean that the decrease of inhibitory influences of TGF-β1 contribute to the predominance of pro-inflammatory activities in severely ill COVID-19 patients. As we know, an enormous release of pro-inflammatory cytokines leads to the cytokine storm, systemic inflammatory response syndrome and multi-organ dysfunction, with an unfavorable outcome of COVID-19 disease [44].
The latent TGF-β complex consists of bioactive free TGF-β non-covalently bound to a major serum protein, α2-macroglobulin [39, 45]. Whereby most of the serum TGF-β exists in a latent form, a small fraction (1.6%) is in a biologically active form [39]. In his theoretical analysis of the possible treatment of COVID-19 with blockade of TGF-β activities Chen proposed that massive activation of latent TGF-β in patients with pneumonia leads to the decrease of circulating level of total TGF-β with a simultaneous increase of active TGF-β in the lungs [8]. However, the measurement of active TGF-β in plasma/serum samples requires a very careful selection of the method and interpretation of the results obtained, given the very short plasma half-life of active TGF-β which lasts about 2–3 min in systemic circulation [46].
To the best of our knowledge, this is the first study in which a very high correlation of platelet counts and serum TGF-β 1 concentrations has been demonstrated in COVID-19 patients. Also, the association of low TGF values with the unfavorable outcome was shown. We believe that these results contribute to the understanding of a very complex role of platelets in inflammatory response in severely ill COVID-19 patients. In clinical practice, blood counts, including platelets are routinely measured. So, low platelet count might indicate the decreased level of anti-inflammatory cytokine TGF- β1 in these patients which the clinicians do not measure routinely. Considering the anti-inflammatory potency of TGF-β1, low platelet counts might indicate the decreased capacity of TGF-β to oppose to proinflammatory cytokines released in systemic inflammatory response. Besides, the association of low serum TGF-β1 levels with the unfavorable outcome recommends it as a serum marker for severe clinical expression of the disease and as an indicator of the unfavorable outcome.
In conclusion, we could say that TGF-β1 levels in COVID-19 patients are strongly associated with the platelet counts. The low levels of TGF-β1 indicate disease severity and the unfavorable outcome.
Data availability
Enquiries about data availability should be directed to the authors.
References
Wu Z, McGoogan JM (2020) Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese center for disease control and prevention. JAMA 323:1239–1242. https://doi.org/10.1001/jama.2020.2648. (PMID: 32091533)
Yuki K, Fujiogi M, Koutsogiannaki S (2020) COVID-19 pathophysiology: A review. Clin immunol (Orlando, Fla.) 215:108427. https://doi.org/10.1016/j.clim.2020.108427
Costela-Ruiz VJ, Illescas-Montes R, Puerta-Puerta JM, Ruiz C, Melguizo-Rodríguez L (2020) SARS-CoV-2 infection: the role of cytokines in COVID-19 disease. Cytokine Growth Factor Rev 54:62–75. https://doi.org/10.1016/j.cytogfr.2020.06.001
Pat Y, Alkan Ş (2020) How does sars-cov-2 manipulates the immune system? Critical role of Th1, Th2, Th17 responses. Turk J Immunol. https://doi.org/10.25002/tji.2020.1270
De Biasi S, Meschiari M, Gibellini L, Bellinazzi C, Borella R, Fidanza L, Gozzi L, Iannone A, Lo Tartaro D, Mattioli M, Paolini A, Menozzi M, Milić J, Franceschi G, Fantini R, Tonelli R, Sita M, Sarti M, Trenti T, Brugioni L, Cicchetti L, Facchinetti F, Pietrangelo A, Clini E, Girardis M, Guaraldi G, Mussini C, Cossarizza A (2020) Marked T cell activation, senescence, exhaustion and skewing towards TH17 in patients with COVID-19 pneumonia. Nat Commun 11:3434. https://doi.org/10.1038/s41467-020-17292-4. (PMID:32632085;PMCID:PMC7338513)
Hirawat R, Saifi MA, Godugu C (2021) Targeting inflammatory cytokine storm to fight against COVID-19 associated severe complications. Life Sci 267:118923. https://doi.org/10.1016/j.lfs.2020.118923
Frank JA, Matthay MA (2014) TGF-β and lung fluid balance in ARDS. Proc Natl Acad Sci U S A 111:885–886. https://doi.org/10.1073/pnas.1322478111. (PMID: 24449829; PMCID: PMC3903208)
Chen W (2020) A potential treatment of COVID-19 with TGF-β blockade. Int J Biol Sci 16:1954–1955. https://doi.org/10.7150/ijbs.46891. (PMID:32398962;PMCID:PMC7211163)
Hamidi SH, Kadamboor Veethil S, Hamidi SH (2021) Role of pirfenidone in TGF-β pathways and other inflammatory pathways in acute respiratory syndrome coronavirus 2 (SARS-Cov-2) infection: a theoretical perspective. Pharmacol Rep 73:712–727. https://doi.org/10.1007/s43440-021-00255-x. (PMID: 33880743; PMCID: PMC8057922)
Wang EY, Chen H, Sun BQ, Wang H, Qu HQ, Liu Y, Sun XZ, Qu J, Fang ZF, Tian L, Zeng YF, Huang SK, Hakonarson H, Liu ZG (2021) Serum levels of the IgA isotype switch factor TGF-β1 are elevated in patients with COVID-19. FEBS Lett 595(13):1819–1824. https://doi.org/10.1002/1873-3468.14104. (PMID: 33961290; PMCID: PMC8209884)
Zivancevic-Simonovic S, Mihaljevic O, Mihajlovic D, Milosevic-Djordjevic O, Jovanovic Z, Mijatovic-Teodorovic L, Colic M (2016) Transforming growth factor beta 1 (TGF-β1) in thyroid cancer patients: a view from the peripheral blood. Ann Clin Lab Sci 46:401–406 (PMID: 27466300)
Lippi G, Plebani M, Henry BM (2020) Thrombocytopenia is associated with severe coronavirus disease 2019 (COVID-19) infections: a meta-analysis. Clin Chim Acta 506:145–148. https://doi.org/10.1016/j.cca.2020.03.022. (PMID: 32178975; PMCID: PMC7102663)
Wool GD, Miller JL (2021) The impact of COVID-19 disease on platelets and coagulation. Pathobiology 88(1):15–27. https://doi.org/10.1159/000512007. (PMID: 33049751; PMCID: PMC7649697)
Hanif M, Sumalani KK, Shaikh Z, Mandhan V, Haider S (2022) Frequency of thrombocytopenia in severe COVID-19 pneumonia and its effects on clinical outcomes. Pak J Pharm Sci 35(5):1385–1390. https://doi.org/10.36721/PJPS.2022.35.5.REG.1385-1390.1)
Zivancevic-Simonovic S, Jovanovic D, Cupurdija V, Milosevic-Djordjevic O, Stanojevic M, Marinkovic M, Igrutinovic N, Stanojevic I, Vojvodic D, Mihaljevic O (2022) Cytokine producing ability of peripheral blood cells from COVID-19 patients after unspecific in vitro stimulation. Inflamm Res 71(3):331–341. https://doi.org/10.1007/s00011-022-01543-9. (PMID: 35157090; PMCID: PMC8853300)
Assoian RK, Komoriya A, Meyers CA, Miller DM, Sporn MB (1983) Transforming growth factor-beta in human platelets. Identification of a major storage site, purification, and characterization. J Biol Chem 258:7155–7160 (PMID: 6602130)
Karolczak K, Watala C (2021) Blood platelets as an important but underrated circulating source of TGFβ. Int J Mol Sci 22:4492. https://doi.org/10.3390/ijms22094492. (PMID:33925804;PMCID:PMC8123509)
Windelov NA, Ostrowski SR, Johansson PI, Wanscher M, Larsen CF, Sorensen AM, Rasmussen LS (2015) Circulating levels of platelet alpha-granule cytokines in trauma patients. Inflamm Res 64(3–4):235–241. https://doi.org/10.1007/s00011-015-0802-4
Tran DQ, Andersson J, Wang R, Ramsey H, Unutmaz D, Shevach EM (2009) GARP (LRRC32) is essential for the surface expression of latent TGF-beta on platelets and activated FOXP3+ regulatory T cells. Proc Natl Acad Sci U S A 106:13445–13450. https://doi.org/10.1073/pnas.0901944106. (PMID: 19651619; PMCID: PMC2726354)
Metcalf Pate KA, Lyons CE, Dorsey JL, Queen SE, Adams RJ, Morrell CN, Mankowski JL (2014) TGFβ-mediated downregulation of thrombopoietin is associated with platelet decline in asymptomatic SIV infection. J Acquir Immune Defic Syndr 65:510–516. https://doi.org/10.1097/QAI.0000000000000048. (PMID:24220290;PMCID:PMC3999250)
Cabalak M, Doğan S, Bal T, Dikmen N (2021) Serum periostin levels in COVID-19: is it useful as a new biomarker? Int J Clin Pract 75:e14728. https://doi.org/10.1111/ijcp.14728. (PMID: 34396648; PMCID: PMC8420097)
Hawrylowicz CM (1993) Viewpoint: a potential role for platelet derived cytokines in the inflammatory response. Platelets 4:1–10. https://doi.org/10.3109/09537109309013189. (PMID: 21043847)
Li C, Li J, Li Y, Lang S, Yougbare I, Zhu G, Chen P, Ni H (2012) Crosstalk between Platelets and the immune system: old systems with new discoveries. Adv Hematol. https://doi.org/10.1155/2012/384685. (PMID: 23008717; PMCID: PMC3447344)
Golebiewska EM, Poole AW (2015) Platelet secretion: from haemostasis to wound healing and beyond. Blood Rev 29:153–162. https://doi.org/10.1016/j.blre.2014.10.003. (PMID: 25468720; PMCID: PMC4452143)
Mussano F, Genova T, Munaron L, Petrillo S, Erovigni F, Carossa S (2016) Cytokine, chemokine, and growth factor profile of platelet-rich plasma. Platelets 27:467–471. https://doi.org/10.3109/09537104.2016.1143922. (Epub 2016 Mar 7 PMID: 26950533)
Smith CW (2021) Release of α-granule contents during platelet activation. Platelets 25:1–12. https://doi.org/10.1080/09537104.2021.1913576. (PMID: 34569425)
Taus F, Salvagno G, Canè S, Fava C, Mazzaferri F, Carrara E, Petrova V, Barouni RM, Dima F, Dalbeni A, Romano S, Poli G, Benati M, De Nitto S, Mansueto G, Iezzi M, Tacconelli E, Lippi G, Bronte V, Minuz P (2020) Platelets promote thromboinflammation in SARS-CoV-2 pneumonia. Arterioscler Thromb Vasc Biol 40:2975–2989. https://doi.org/10.1161/ATVBAHA.120.315175. (Epub 2020 Oct 14. PMID: 33052054; PMCID: PMC7682791)
Tafazoli A, Anil Kumar S, Othman M (2021) Thrombocytopathy vs Platelet hyper-reactivity in COVID-19: diverse pathologies, disease outcomes and therapeutic implications. Platelets 33(1):48–53. https://doi.org/10.1080/09537104.2021.1961718. (Epub 2021 Nov 30 PMID: 34847829)
Güçlü E, Kocayiğit H, Okan HD, Erkorkmaz U, Yürümez Y, Yaylacı S, Koroglu M, Uzun C (1992) Karabay O (2020) effect of COVID-19 on platelet count and its indices. Rev Assoc Med Bras 66:1122–1127. https://doi.org/10.1590/1806-9282.66.8.1122. (PMID: 32935808)
Tjendra Y, Al Mana AF, Espejo AP, Akgun Y, Millan NC, Gomez-Fernandez C, Cray C (2020) Predicting Disease severity and outcome in COVID-19 patients: a review of multiple biomarkers. Arch Pathol Lab Med 144:1465–1474. https://doi.org/10.5858/arpa.2020-0471-SA. (PMID: 32818235)
Yousefifard M, Mohamed Ali K, Aghaei A, Zali A, Madani Neishaboori A, Zarghi A, Safari S, Hashemi B, Forouzanfar MM, Hosseini M (2020) Corticosteroids on the management of coronavirus disease 2019 (COVID-19): a systemic review and meta-analysis. Iran J Public Health 49:1411–1421. https://doi.org/10.18502/ijph.v49i8.3863. (PMID: 33083317; PMCID: PMC7554375)
Hu Z, Chen W, Liang W, Xu C, Sun W, Yi Y (2021) Severe exacerbation of immune thrombocytopenia and COVID-19: the favorable response to corticosteroid-based therapy-a case report. Ann Hematol 100:2135–2137. https://doi.org/10.1007/s00277-020-04070-x. (PMID: 32500224; PMCID: PMC7270513)
Delshad M, Safaroghli-Azar A, Pourbagheri-Sigaroodi A, Poopak B, Shokouhi S, Bashash D (2021) Platelets in the perspective of COVID-19; pathophysiology of thrombocytopenia and its implication as prognostic and therapeutic opportunity. Int Immunopharmacol 99:107995. https://doi.org/10.1016/j.intimp.2021.107995. (Epub 2021 Jul 21. PMID: 34304001; PMCID: PMC8295197)
Bommenahalli Gowda S, Gosavi S, Ananda Rao A, Shastry S, Raj SC, Menon S, Suresh A, Sharma A (2021) Prognosis of COVID-19: red cell distribution width, platelet distribution width, and C-reactive protein. Cureus 13:e13078. https://doi.org/10.7759/cureus.13078. (PMID: 33680618; PMCID: PMC7932824)
Gao Y, Li Y, Yu X, Guo S, Ji X, Sun T, Lan C, Lavergne V, Ghannoum M, Li L (2014) The impact of various platelet indices as prognostic markers of septic shock. PLoS ONE 9:e103761. https://doi.org/10.1371/journal.pone.0103761. (PMID: 25118886; PMCID: PMC4131909)
Waris A, Din M, Khalid A, Abbas Lail R, Shaheen A, Khan N, Nawaz M, Baset A, Ahmad I, Ali M (2021) Evaluation of hematological parameters as an indicator of disease severity in Covid-19 patients: Pakistan’s experience. J Clin Lab Anal 35:e23809. https://doi.org/10.1002/jcla.23809. (PMID: 34028884; PMCID: PMC8183923)
Lokwani DP, Yadav BS, Bharti S, Gupta V, Toppo N (2021) Evaluation of hematological, coagulation and inflammatory biomarker’s role in predicting the severity of disease in patients with COVID-19, admitted in designated COVID-19 hospital of central India. Indian J Pathol Microbiol 64:735–740. https://doi.org/10.4103/IJPM.IJPM_1350_20. (PMID: 34673594)
Grainger DJ, Mosedale DE, Metcalfe JC, Weissberg PL, Kemp PR (1995) Active and acid-activatable TGF-beta in human sera, platelets and plasma. Clin Chim Acta 235:11–31. https://doi.org/10.1016/0009-8981(94)05995-4. (PMID: 7634487)
Khan SA, Joyce J, Tsuda T (2012) Quantification of active and total transforming growth factor-β levels in serum and solid organ tissues by bioassay. BMC Res Notes 5:636. https://doi.org/10.1186/1756-0500-5-636. (PMID:23151377;PMCID:PMC3556312)
Kropf J, Schurek JO, Wollner A, Gressner AM (1997) Immunological measurement of transforming growth factor-beta 1 (TGF-beta1) in blood; assay development and comparison. Clin Chem 43:1965–1974 (PMID: 9342020)
Brotfain E, Schwartz A, Boniel A, Koyfman L, Boyko M, Kutz R, Klein M (2016) Clinical outcome of critically ill patients with thrombocytopenia and hypophosphatemia in the early stage of sepsis. Anaesthesiol Intensive Ther 48(5):294–299. https://doi.org/10.5603/AIT.a2016.0053
Al Saleh K, AlQahtani RM (2021) Platelet count patterns and patient outcomes in sepsis at a tertiary care center beyond the APACHE score. Medicine 100(18):e25013. https://doi.org/10.1097/MD.0000000000025013
Zong X, Gu Y, Yu H, Li Z, Wang Y (2021) Thrombocytopenia is associated with COVID-19 severity and outcome: an updated meta-analysis of 5637 patients with multiple outcomes. Lab Med 52(1):10–15. https://doi.org/10.1093/labmed/lmaa067
Ye Q, Wang B, Mao J (2020) The pathogenesis and treatment of the `Cytokine Storm’ in COVID-19. J Infect 80:607–613. https://doi.org/10.1016/j.jinf.2020.03.037. (Epub 2020 PMID: 32283152; PMCID: PMC7194613)
McCaffrey TA, Falcone DJ, Brayton CF, Agarwal LA, Welt FG, Weksler BB (1989) Transforming growth factor-beta activity is potentiated by heparin via dissociation of the transforming growth factor-beta/alpha 2-macroglobulin inactive complex. J Cell Biol 109:441–448. https://doi.org/10.1083/jcb.109.1.441. (PMID:2473082;PMCID:PMC2115487)
Wakefield LM, Winokur TS, Hollands RS, Christopherson K, Levinson AD, Sporn MB (1990) Recombinant latent transforming growth factor beta 1 has a longer plasma half-life in rats than active transforming growth factor beta 1, and a different tissue distribution. J Clin Invest 86:1976–1984. https://doi.org/10.1172/JCI114932. (PMID:2254455;PMCID:PMC329834)
Funding
The study was supported by the Ministry of Education, Science and Technological Development of the Republic of Serbia (Grant No. III41010), and Faculty of Medical Sciences, University of Kragujevac (Grant No. JP 08/17).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by VC, MS-P, OM-D and RM. The first draft of the manuscript was written by SZ-S and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zivancevic-Simonovic, S., Minic, R., Cupurdija, V. et al. Transforming growth factor beta 1 (TGF-β1) in COVID-19 patients: relation to platelets and association with the disease outcome. Mol Cell Biochem 478, 2461–2471 (2023). https://doi.org/10.1007/s11010-023-04674-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11010-023-04674-7