Abstract
Ascending inflammation from the vagina is a major cause of preterm birth. Currently, this condition—especially when uncontrolled—has no effective treatment. Human amniotic fluid stem cells (hAFSCs) are mesenchymal stem cells known to exert potent anti-inflammatory effects in animal models of perinatal diseases, such as periventricular leukomalacia, myelomeningocele, and neonatal sepsis. However, hAFSC therapy for inflammation-induced preterm birth has not been tested. In order to determine the therapeutic effect of hAFSC transplantation, we employed a preterm mouse model of ascending infection; this model was constructed by administering lipopolysaccharide to pregnant mice. We investigated the preterm birth rate and evaluated the inflammation of tissues, which is related to progressive infections, such as those involving the cervix, placenta, and lavage cells, using real-time qPCR. Further, we tracked the fluorescence of fluorescently labeled hAFSCs using an in vivo imaging system, and hAFSC aggregation was evaluated using immunohistochemistry analysis. We also investigated the presence of multiple types of peritoneal macrophages via flow cytometry analysis. Finally, we performed sphere culturing and co-culturing to determine the therapeutic effects of hAFSCs, such as their anti-inflammatory effects and their potential to alter macrophage polarization. We found that hAFSC administration to the peritoneal cavity significantly reduced inflammation-induced preterm birth in the mouse model. The treatment also significantly suppressed inflammation of the placenta and cervix. Transplanted hAFSCs may have aggregated with peritoneal macrophages, switching them from an inflammatory to an anti-inflammatory type. This property has been reported in vivo previously, but here, we examined the effect in vitro. Our findings support the hypothesis that hAFSCs suppress inflammation and reduce preterm birth by switching macrophage polarity. This study is the first to demonstrate that hAFSCs are effective in the treatment and prevention of inflammation-induced preterm birth.





Similar content being viewed by others
Data availability
Not applicable
Abbreviations
- FBS:
-
Fetal bovine serum
- hAFSCs:
-
Human amniotic fluid stem cells
- LPS:
-
Lipopolysaccharide
- MSCs:
-
Mesenchymal stem cells
- α-MEM:
-
Alpha-modified Eagle minimum essential medium
References
Liu L, Johnson HL, Cousens S, Perin J, Scott S, Lawn JE et al (2012) Global, regional, and national causes of child mortality: An updated systematic analysis for 2010 with time trends since 2000. Lancet 379:2151–2161. https://doi.org/10.1016/S0140-6736(12)60560-1
Goldenberg RL, Hauth JC, Andrews WW (2000) Intrauterine infection and preterm delivery. N Engl J Med 342:1500–1507. https://doi.org/10.1056/NEJM200005183422007
Gibbs RS, Eschenbach DA (1997) Use of antibiotics to prevent preterm birth. Am J Obstet Gynecol 177:375–380. https://doi.org/10.1016/s0002-9378(97)70201-1
Le Blanc K, Tammik L, Sundberg B, Haynesworth SE, Ringdén O (2003) Mesenchymal stem cells inhibit and stimulate mixed lymphocyte cultures and mitogenic responses independently of the major histocompatibility complex. Scand J Immunol 57:11–20. https://doi.org/10.1046/j.1365-3083.2003.01176.x
Németh K, Leelahavanichkul A, Yuen PST, Mayer B, Parmelee A, Doi K et al (2009) Bone marrow stromal cells attenuate sepsis via prostaglandin E(2)-dependent reprogramming of host macrophages to increase their interleukin-10 production. Nat Med 15:42–49. https://doi.org/10.1038/nm.1905
Zhao Q, Ren H, Han Z (2016) Mesenchymal stem cells: Immunomodulatory capability and clinical potential in immune diseases. J Cell Immunother 2:3–20. https://doi.org/10.1016/j.jocit.2014.12.001
Laube M, Stolzing A, Thome UH, Fabian C (2016) Therapeutic potential of mesenchymal stem cells for pulmonary complications associated with preterm birth. Int J Biochem Cell Biol 74:18–32. https://doi.org/10.1016/j.biocel.2016.02.023
Otani T, Ochiai D, Masuda H, Abe Y, Fukutake M, Matsumoto T et al (2019) The neurorestorative effect of human amniotic fluid stem cells on the chronic phase of neonatal hypoxic–ischemic encephalopathy in mice. Pediatr Res 85:97–104. https://doi.org/10.1038/s41390-018-0131-8
Paton MCB, McDonald CA, Allison BJ, Fahey MC, Jenkin G, Miller SL (2017) Perinatal brain injury as a consequence of preterm birth and intrauterine inflammation: Designing targeted stem cell therapies. Front Neurosci 11:200. https://doi.org/10.3389/fnins.2017.00200
Yin L, Wang S, Zhang N, Bai X, Xie J, Wen Q et al (2020) Elevation of stromal cell-derived factor 1 and C-X-C chemokine receptor type 4 in white matter damage treatment with recombinant human erythropoietin and human umbilical cord mesenchymal stem cells in a rat model of preterm birth. Int J Dev Neurosci 80:247–256. https://doi.org/10.1002/jdn.10021
Abe Y, Ochiai D, Sato Y, Kanzaki S, Ikenoue S, Kasuga Y et al (2020) Prophylactic therapy with human amniotic fluid stem cells improves long-term cognitive impairment in rat neonatal sepsis survivors. Int J Mol Sci. https://doi.org/10.3390/ijms21249590
Sato Y, Ochiai D, Abe Y, Masuda H, Fukutake M, Ikenoue S et al (2020) Prophylactic therapy with human amniotic fluid stem cells improved survival in a rat model of lipopolysaccharide-induced neonatal sepsis through immunomodulation via aggregates with peritoneal macrophages. Stem Cell Res Ther 11:300. https://doi.org/10.1186/s13287-020-01809-1
Abe Y, Ochiai D, Masuda H, Sato Y, Otani T, Fukutake M et al (2019) In utero amniotic fluid stem cell therapy protects against myelomeningocele via spinal cord coverage and hepatocyte growth factor secretion. Stem Cells Transl Med 8:1170–1179. https://doi.org/10.1002/sctm.19-0002
De Coppi P, Bartsch G Jr, Siddiqui MM, Xu T, Santos CC, Perin L et al (2007) Isolation of amniotic stem cell lines with potential for therapy. Nat Biotechnol 25:100–106. https://doi.org/10.1038/nbt1274
Loukogeorgakis SP, De Coppi P (2017) Concise review: Amniotic fluid stem cells: the known, the unknown, and potential regenerative medicine applications. Stem Cells 35:1663–1673. https://doi.org/10.1002/stem.2553
Reznikov LL, Fantuzzi G, Selzman CH, Shames BD, Barton HA, Bell H et al (1999) ‘Utilization of endoscopic inoculation in a mouse model of intrauterine infection-induced preterm birth: role of interleukin 1beta. Biol Reprod 60:1231–1238. https://doi.org/10.1095/biolreprod60.5.1231
Gonzalez JM, Franzke CW, Yang F, Romero R, Girardi G (2011) Complement activation triggers metalloproteinases release inducing cervical remodeling and preterm birth in mice. Am J Pathol 179:838–849. https://doi.org/10.1016/j.ajpath.2011.04.024
Elovitz MA, Mrinalini C (2004) Animal models of preterm birth. Trends Endocrinol Metab 15:479–487. https://doi.org/10.1016/j.tem.2004.10.009
Yamashita A, Kawana K, Tomio K, Taguchi A, Isobe Y, Iwamoto R et al (2013) Increased tissue levels of omega-3 polyunsaturated fatty acids prevents pathological preterm birth. Sci Rep. https://doi.org/10.1038/srep03113
Platt N, Suzuki H, Kurihara Y, Kodama T, Gordon S (1996) Role for the class A macrophage scavenger receptor in the phagocytosis of apoptotic thymocytes in vitro. Proc Natl Acad Sci U S A 93:12456–12460. https://doi.org/10.1073/pnas.93.22.12456
Furuya H, Taguchi A, Kawana K, Yamashita A, Inoue E, Yoshida M et al (2015) Resveratrol protects against pathological preterm birth by suppression of macrophage-mediated inflammation. Reprod Sci 22:1561–1568. https://doi.org/10.1177/1933719115589413
Basraon SK, Menon R, Makhlouf M, Longo M, Hankins GD, Saade GR et al (2012) Can statins reduce the inflammatory response associated with preterm birth in an animal model? Am J Obstet Gynecol 207(224):e1-7. https://doi.org/10.1016/j.ajog.2012.06.020
Elovitz MA, Brown AG, Breen K, Anton L, Maubert M, Burd I (2011) Intrauterine inflammation, insufficient to induce parturition, still evokes fetal and neonatal brain injury. Int J Dev Neurosci 29:663–671. https://doi.org/10.1016/j.ijdevneu.2011.02.011
Salminen A, Paananen R, Vuolteenaho R, Metsola J, Ojaniemi M, Autio-Harmainen H et al (2008) Maternal endotoxin-induced preterm birth in mice: Fetal responses in toll-like receptors, collectins, and cytokines. Pediatr Res 63:280–286. https://doi.org/10.1203/PDR.0b013e318163a8b2
Sheller-Miller S, Radnaa E, Yoo JK, Kim E, Choi K, Kim Y et al (2021) Exosomal delivery of NF-κB inhibitor delays LPS-induced preterm birth and modulates fetal immune cell profile in mouse models. Sci Adv. https://doi.org/10.1126/sciadv.abd3865
Arabpour M, Saghazadeh A, Rezaei N (2021) Anti-inflammatory and M2 macrophage polarization-promoting effect of mesenchymal stem cell-derived exosomes. Int Immunopharmacol 97:107823. https://doi.org/10.1016/j.intimp.2021.107823
Corcelli M, Hawkins K, Vlahova F, Hunjan A, Dowding K, De Coppi P et al (2018) Neuroprotection of the hypoxic-ischemic mouse brain by human CD117(+)CD90(+)CD105(+) amniotic fluid stem cells. Sci rep. https://doi.org/10.1038/s41598-018-20710-9
Jiménez J, Lesage F, Richter J, Nagatomo T, Salaets T, Zia S et al (2018) Upregulation of vascular endothelial growth factor in amniotic fluid stem cells enhances their potential to attenuate lung injury in a preterm rabbit model of bronchopulmonary dysplasia. Neonatology 113:275–285. https://doi.org/10.1159/000481794
Stenson WF (2014) Preventing necrotising enterocolitis with amniotic fluid stem cells. Gut 63:218–219. https://doi.org/10.1136/gutjnl-2013-304653
Santana AC, Dellê H, Cavaglieri RC, Lopes MAB, Francisco RPV, Zugaib M et al (2012) Protective effects of human amniotic fluid stem cells in a model of aorta allograft vasculopathy in rats. Transplant Proc 44:2490–2494. https://doi.org/10.1016/j.transproceed.2012.07.022
Zavatti M, Beretti F, Casciaro F, Bertucci E, Maraldi T (2020) Comparison of the therapeutic effect of amniotic fluid stem cells and their exosomes on monoiodoacetate-induced animal model of osteoarthritis. BioFactors 46:106–117. https://doi.org/10.1002/biof.1576
Sala E, Genua M, Petti L, Anselmo A, Arena V, Cibella J et al (2015) Mesenchymal stem cells reduce colitis in mice via release of TSG6, independently of their localization to the intestine. Gastroenterology 149:163-176.e20. https://doi.org/10.1053/j.gastro.2015.03.013
Li Y, Zhang D, Xu L, Dong L, Zheng J, Lin Y et al (2019) Cell-cell contact with proinflammatory macrophages enhances the immunotherapeutic effect of mesenchymal stem cells in two abortion models. Cell Mol Immunol 16:908–920. https://doi.org/10.1038/s41423-019-0204-6
Lee TH, Wisniewski HG, Vilcek J (1992) A novel secretory tumor necrosis factor-inducible protein (TSG-6) is a member of the family of hyaluronate binding proteins, closely related to the adhesion receptor CD44. J Cell Biol 116:545–557. https://doi.org/10.1083/jcb.116.2.545
Day AJ, Milner CM (2019) TSG-6: A multifunctional protein with anti-inflammatory and tissue-protective properties. Matrix Biol 78–79:60–83. https://doi.org/10.1016/j.matbio.2018.01.011
Lee RH, Pulin AA, Seo MJ, Kota DJ, Ylostalo J, Larson BL et al (2009) Intravenous hMSCs improve myocardial infarction in mice because cells embolized in lung are activated to secrete the anti-inflammatory protein TSG-6. Cell Stem Cell 5:54–63. https://doi.org/10.1016/j.stem.2009.05.003
Choi H, Lee RH, Bazhanov N, Oh JY, Prockop DJ (2011) Anti-inflammatory protein TSG-6 secreted by activated MSCs attenuates zymosan-induced mouse peritonitis by decreasing TLR2/NF-κB signaling in resident macrophages. Blood 118:330–338. https://doi.org/10.1182/blood-2010-12-327353
Di G, Du X, Qi X, Zhao X, Duan H, Li S et al (2017) Mesenchymal stem cells promote diabetic corneal epithelial wound healing through TSG-6-dependent stem cell activation and macrophage switch. Invest Ophthalmol Vis Sci 58:4344–4354. https://doi.org/10.1167/iovs.17-21506
Zhang S, Liu Y, Zhang X, Zhu D, Qi X, Cao X et al (2018) Prostaglandin E2 hydrogel improves cutaneous wound healing via M2 macrophages polarization. Theranostics 8:5348–5361. https://doi.org/10.7150/thno.27385
Philipp D, Suhr L, Wahlers T, Choi YH, Paunel-Görgülü A (2018) Preconditioning of bone marrow-derived mesenchymal stem cells highly strengthens their potential to promote IL-6-dependent M2b polarization. Stem Cell Res Ther 9:286. https://doi.org/10.1186/s13287-018-1039-2
Goldenberg RL, Culhane JF, Iams JD, Romero R (2008) Epidemiology and causes of preterm birth. Lancet 371:75–84. https://doi.org/10.1016/S0140-6736(08)60074-4
Moutquin JM (2003) Classification and heterogeneity of preterm birth. BJOG 110(Suppl 20):30–33. https://doi.org/10.1016/s1470-0328(03)00021-1
Kasuga Y, Ikenoue S, Tanaka M, Ochiai D (2021) Management of pregnancy after radical trachelectomy. Gynecol Oncol 162:220–225. https://doi.org/10.1016/j.ygyno.2021.04.023
Romero R, Miranda J, Chaiworapongsa T, Korzeniewski SJ, Chaemsaithong P, Gotsch F et al (2014) Prevalence and clinical significance of sterile intra-amniotic inflammation in patients with preterm labor and intact membranes. Am J Reprod Immunol 72:458–474. https://doi.org/10.1111/aji.12296
Jain VG, Willis KA, Jobe A, Ambalavanan N (2021) Chorioamnionitis and neonatal outcomes. Pediatr Res. https://doi.org/10.1038/s41390-021-01633-0
Caughey AB, Robinson JN, Norwitz ER (2008) Contemporary diagnosis and management of preterm premature rupture of membranes. Rev Obstet Gynecol 1:11–22
Dagklis T, Petousis S, Margioula-Siarkou C, Mavromatidis G, Kalogiannidis I, Prapas N et al (2013) Parameters affecting latency period in PPROM cases: a 10-year experience of a single institution. J Matern Fetal Neonatal Med 26:1455–1458. https://doi.org/10.3109/14767058.2013.784257
Test G, Levy A, Wiznitzer A, Mazor M, Holcberg G, Zlotnik A et al (2011) Factors affecting the latency period in patients with preterm premature rupture of membranes. Arch Gynecol Obstet 283:707–710. https://doi.org/10.1007/s00404-010-1448-7
McCarthy R, Martin-Fairey C, Sojka DK, Herzog ED, Jungheim ES, Stout MJ et al (2018) Mouse models of preterm birth: suggested assessment and reporting guidelines. Biol Reprod 99:922–937. https://doi.org/10.1093/biolre/ioy109
Bazhanov N, Ylostalo JH, Bartosh TJ, Tiblow A, Mohammadipoor A, Foskett A et al (2016) Intraperitoneally infused human mesenchymal stem cells form aggregates with mouse immune cells and attach to peritoneal organs. Stem Cell Res Ther 7:27. https://doi.org/10.1186/s13287-016-0284-5
Acknowledgements
Not applicable.
Funding
This work was supported by JSPS Grant-in-Aid for Scientific Research (B) (grant number 20K08215) and (C) (grant number 21H03080).
Author information
Authors and Affiliations
Contributions
YA and DO were involved in study conception and design, provision of study material or patients, collection and/or assembly of data, data analysis and interpretation, and manuscript writing. DO also provided administrative support. SK was involved in data collection and/or assembly, as well as data analysis and interpretation. YS and TO provided study material or patients, collected and/or assembled data, as well as analyzed and interpreted data. SI and YK provided administrative support and helped with data analysis and interpretation. MT was involved in study conception and design; administrative support; data collection, assembly, analysis, and interpretation; and manuscript writing. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
SK is an employee of StemCell Institute Inc. Other authors have no conflict of interest to declare.
Ethical approval
All experimental protocols were approved by the Institutional Review Board of Keio University School of Medicine (no. 20140285), and informed consent was obtained from all the volunteer donors. All animal experiments were approved by the Animal Committee of Keio University (no. 18025).
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
11010_2022_4512_MOESM1_ESM.pptx
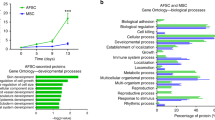
Supplementary file1 (PPTX 5301 kb) Figure 1. Characteristics of hAFSCs. (a) Culture, (b) surface marker expression, and (c) differentiation potential of human amniotic fluid stem cells (hAFSCs), Supplementary Figure 2. Transvaginal administration of LPS.
Rights and permissions
About this article
Cite this article
Abe, Y., Ochiai, D., Kanzaki, S. et al. Prophylactic administration of human amniotic fluid stem cells suppresses inflammation-induced preterm birth via macrophage polarization. Mol Cell Biochem 478, 363–374 (2023). https://doi.org/10.1007/s11010-022-04512-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11010-022-04512-2