Abstract
Objective
Maternal body mass index (BMI) and gestational weight gain (GWG) are modifiable risk factors that influence pregnancy outcomes. We examined the association between the two factors in pregnant women in Qatar with regard to the GWG recommendations by the Institute of Medicine (IOM) in 2009.
Methods
We performed a population-based retrospective cohort analysis of 3547 singleton births, using routinely collected data from a Middle Eastern hospital database.
Results
The mean maternal age was 29.7 ± 5.5 years, prepregnancy BMI was 27.5 ± 5.8 kg/m2, GWG was 9.58 kg ± 6.87 kg and gestational age at birth was 38.5 ± 1.9 weeks. In line with IOM recommendations, we found that higher BMI was correlated with decreased GWG and BMI was significantly associated with GWG even after adjusting for maternal age, parity, and infants’ gestational age at birth. Nonetheless, GWG in more than one-third of women who were overweight or obese exceeded the IOM recommendation.
Significance
Gestational weight gain is an important factor that influences short- and long-term pregnancy outcomes in women and their infants. The present study findings show that while many women achieved optimum weight gain during pregnancy, a significant proportion of who are overweight or obese, exceeded recommended weight gain.
Similar content being viewed by others
Objectives
Excessive gestational weight gain (GWG) has been linked to short- and long-term adverse fetal and maternal outcomes. It is a modifiable risk factor associated with an increase in rates of cesarean deliveries, infants large for gestational age, postpartum weight retention in women, and the development of early childhood obesity (Hernandez, 2012; Li et al., 2018, 2019; Ludwig et al., 2013; Siega-Riz et al., 2009; Sridhar et al., 2014, 2016; Voerman et al., 2019). GWG recommendations and assessment are often based on a woman’s prepregnancy body mass index (BMI). Obesity is currently a global health problem among men and women; with more than 1.9 billion people reported to be overweight, and 650 million living with obesity (WHO, 2017). With this global trend, increasing numbers of women are likely to begin pregnancy classified with either overweight or obesity.
Qatar is a high-income country with a large number of people having overweight or living with obesity. According to the 2006 Qatar World Health Survey, which included Qatari citizens and residents, 39% of the population was classified as overweight, 28.8% as obese, and 3.3% as morbidly obese (National Health Authority (Qatar), 2006). Of the Qatari citizens alone, 75% were classified as overweight or obese, and more than 66% of expatriates as either overweight or obese. Moreover, according to the 2012 STEPwise survey of only Qatari citizens, the mean BMI in the Qatari population aged 18 to 64 years were 28.8 kg/m2 in men and 29.5 kg/m2 in women (Haj Bakri and Al-Thani, 2013). In that survey, 70.1% of participants had a BMI of ≥ 25 kg/m2, the average BMI of nonpregnant women aged 18–44 years was 28.4 kg/m2, and of those women, 25.4% were classfied as overweight and 36.4% as having obesity. These proportions were similar in a Qatar Biobank annual report (Qatar Biobank, 2017). Obesity, metabolic syndromes, and lifestyle-related disorders are nationally prioritized issues in Qatar, and efforts have been ongoing to mitigate these health burdens. Although pregnant women receive dietary and lifestyle education, not all may receive adequate education about BMI and expected GWG unless it is particularly indicated. In several studies, conducted in different parts of the world such as the United States, Sweden, Asian nations, and other countries, GWG decreased with a higher BMI, and a significant proportion of women gained more weight than recommended (Arora & Tamber Aeri, 2019; Johansson et al., 2016; Cheney et al., 2017; Power et al., 2018). The Institute of Medicine (IOM) recommend the following GWG for various groups according to BMI: 12.5–18.0 kg (underweight), 11.5–16.0 kg (normal weight), 7.0–11.5 kg (overweight), and 5.0–9.0 (obese).
We did not find reports of any large study on GWG in Qatar, therefore we examined the pattern of GWG among pregnant women in Qatar. Evidence generated could inform policy and practice in the characterization and prediction of GWG in Qatar. The objective of this study was to examine the association between prepregnancy BMI and GWG among women with singleton pregnancies with regard to the 2009 recommendations of the IOM (Rasmussen & Yaktine, 2009).
Methods
Study Design
We performed a retrospective analysis of data retrieved from the population-based Perinatal Neonatal Outcomes Research Study in the Arabian Gulf (PEARL)–Peristat Registry in Qatar. This observational research registry was funded by the Qatar National Research Fund and sponsored by the Medical Research Centre of Hamad Medical Corporation. The primary aim of the registry was to study fetal and maternal outcomes in the perinatal–neonatal period in Qatar, and it contained routinely collected data extracted from hospital records for women and newborns. The research complied with all the relevant regulations and institutional policies, was conducted in accordance with the tenets of the Helsinki Declaration, and was approved by the Medical Research Centre, Hamad Medical Corporation. The requirement for consent was waived because of the retrospective nature of the study.
Setting and Participants
Data retrieved from the registry for this analysis included data from public hospitals, which account for approximately 86% of all deliveries in Qatar (Haj Bakri and Al-Thani, 2013). In addition, health care quality in private hospitals is comparable with that in public hospitals.
Data collection for the registry started in January 2017 in the largest maternity hospital (Women’s Wellness Research Centre) and in March 2017 in three other hospitals, Al-Wakra, Al-Khor, and Cuban hospitals. Information on participants with completed data entry from January to June 2017 was retrieved for this analysis. All 9249 participants who gave birth to singletons at 24 weeks of gestation and above were eligible. The inclusion criterion was data for GWG; no exclusion criteria were used. Data from 3547 (37.6%) of the women were available for computing GWG and were included in the analysis. According to Johansson and colleagues, data for GWG is often lacking in many birth registers; such data were available for only one third of women in the Swedish Medical Birth Register (Johansson et al., 2016). In evaluating our sample for selection bias, we observed that the proportions of demographic variables did not differ significantly between the women with and without GWG data; differences ranged from 0.4 to 2.8%, although the proportion of women with diabetes during pregnancy was 11% higher among the women with GWG data than among those without. Our sample was therefore representative of the population of women who delivered singleton infants within the study period.
Primary Outcome Variable
GWG (in kilograms) was defined as the difference between measured weight at delivery and measured or self-reported prepregnancy weight (International Association of Diabetes in Pregnancy Study Group (IADPSG) Working Group on Outcome Definitions et al., 2015). Maternal prepregnancy weight and weights at each antenatal care visit were routinely documented in the electronic medical records of every pregnant woman. Prepregnancy weight in this study was defined as documented weight before confirmation of pregnancy or weight at early antenatal booking (< 13 weeks’ gestation). According to a review by the Working Group on Outcome Definitions of the International Association of Diabetes in Pregnancy Study Group (IADPSG), whose aim is to establish consensus definitions for maternal and fetal outcomes, GWG had various definitions in the literature. The definition finally adopted by the working group was “Weight from preconception (preferable) (measured or self-reported) or within 3 months of conception, or if not available, at first pregnancy visit within first trimester, until the last measured weight during pregnancy (within 4 weeks of delivery)” (International Association of Diabetes in Pregnancy Study Group (IADPSG) Working Group on Outcome Definitions et al., 2015). Data for weight at delivery were available for approximately 99.5% of the study population, but prepregnancy weights and weights at early antenatal booking (< 13 weeks’ gestation) were available for only 21% (1939/9249) and 24.8% (2298/9249) of the sample, respectively. To conform with the IADPSG definition, we used the booking weight at < 13 weeks’ gestation as the prepregnancy weight for cases in which the prepregnancy weight was unavailable (Online Resource 1). The same approach was used in computing BMI.
Secondary Outcome Variables
The proportions of women who gained less than, within, or more than the GWGs recommended by the IOM for each BMI category served as the secondary outcome variables.
BMI and Other Covariables
Prepregnancy BMI (in kilograms per square meter) was calculated as the ratio of prepregnancy weight (in kilograms) divided by height (in square meters). It was examined as both a continuous variable and a categorical variable, and BMI categories were defined as underweight (≤ 18.5 kg/m2), normal weight (18.5–24.9 kg/m2), overweight (25.0–29.9 kg/m2), and obese (≥ 30.0 kg/m2) (WHO, 2006).
Women
Maternal age at delivery was assessed in groups: ≤19, 20–24, 25–29, 30–34, and ≥ 35 years. For parity, women were considered nulliparous or uniparous/multiparous. Nationality was classified as Qatari or non-Qatari. The presence of diabetes (overt or gestational) was coded as “yes” (1) or “no” (0).
Newborns
Sex was classified as male or female. Gestational age at delivery was assessed in groups: ≤28, 29–32, 33–36, and ≥ 37 weeks.
Statistical Analysis
Descriptive statistics were calculated as numbers and percentages or as means and standard deviations (SDs) as applicable to show the distribution of variables. Both GWG and BMI had normal distributions. First, we estimated the mean GWG for each covariable and examined the association of each covariable with GWG by using Pearson’s correlation coefficient. Then we performed univariable and multivariable linear regression to examine and test the association between GWG and prepregnancy BMI while adjusting for the effects of significant covariables. We utilized two models for linear regression: BMI was a continuous covariable in the first model and a categorical covariable in the second model. A univariable general linear model, UNIANOVA (univariable analysis of variance) was used to estimate each association of BMI category with GWG. The IBM-SPSS UNIANOVA command provides results for regression analysis and analysis of variance for a dependent variable based on one or more factors. Finally, the mean GWG in each BMI category was compared to the IOM’s recommended ranges. Furthermore, the proportions of women who gained less than, within, and more than the IOM’s recommendation were also estimated in terms of the 25th, 50th, and 75th percentiles. To perform statistical analysis, we used IBM-SPSS 22 statistical software (IBM Corporation, Armonk, NY, USA). Statistical significance was determined in 95% confidence intervals (CI) and indicated by p levels of < 0.05.
Results
Table 1 lists the demographic characteristics and the mean GWG of the 3547 women in this study. The mean maternal age was 29.7 ± 5.5 years, prepregnancy BMI was 27.5 ± 5.8 kg/m2 and around three-fifth of these women; n = 2194 (61.9%) were aged 25–34 years. Majority of the women who gave birth were non-Qatari with term pregnancies (mean gestational age at birth, 38.5 ± 1.9 weeks) who had at least one previous parous experience. Using the WHO BMI cut-off mentioned earlier, 95 (2.7%) were classified as underweight before pregnancy, 1247 (35.2%) as normal weight, 1143 (32.2%) as overweight, and 1061 (29.9%) as living with obesity before pregnancy. Prepregnancy BMI data was missing for one woman.
The overall mean GWG was 9.58 kg (SD = 6.87 kg), with finding showing an inverse correlation between GWG andd BMI. GWG was highest in the underweight group (mean = 13.17 kg, SD = 8.27 kg) and lowest among the women living with obesity (mean = 7.10 kg, SD = 6.85 kg; Table 1). The mean GWG decreased with increased maternal age, parity, and prepregnancy BMI. Mean GWG was also decreased in women with any form of diabetes in pregnancy. In contrast, GWG increased with gestational age of the fetus. The mean GWG with regard to the nationality of the women and sex of the newborns were equivalent.
In the univariable analysis (Table 1), we found a significant correlation between GWG and prepregnancy BMI (r[3544] = − 0.260; p = < 0.001), maternal age (r[3545] = − 0.162; p = < 0.001), parity (r[3545] = − 0.196; p = < 0.001), the gestational age of the newborn (r[3545] = 0.124; p = < 0.001), and the presence of diabetes during pregnancy (r[3545] = − 0.156; p = < 0.001). We found no correlation between nationality, gender of newborn, and GWG.
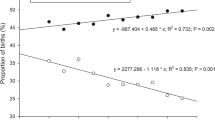
In both regression models examined; with BMI categorized or continuous,, BMI was significantly associated with GWG (Table 2). The association remained significant even after we adjusted for maternal age, parity, and the gestational age of the newborn (adjusted beta = − 0.26 kg; 95% CI − 0.29 kg, − 0.22 kg; p < 0.05). The adjusted regression model showed that for every unit increase in BMI (with an intercept of 12.1), GWG decreased by 0.26 units; where GWG = (− 0.26 × BMI) + 12.1. For all BMI groups, and in comparison with the women living with obesity, GWG increased by a factor of 2.11 kg in women grouped as overweight, 3.14 kg in the normal weight group, and 4.74 kg in the underweight group (Table 2).
GWG and IOM Recommendations
Overall, the mean GWG for the BMI categories were within the IOM’s recommendations (Fig. 1). We found that 41% of all the women women gained less than the IOM’s recommendations, 28% gained within those recommendations, and 31% gained more than those recommendations (Fig. 2). In approximately 83% of women classified as underweight and 82% of women as normal weight, GWG was within or less than IOM values, whereas in 61% of women with overweight and 63% of women living with obesity, GWG was within or less than IOM values (Figs. 1 and 2).
Discussion
In this study, we examined the relationship between prepregnancy BMI and GWG among women with singleton pregnancies with regard to the 2009 recommendations of the Institute of Medicine (IOM) (Rasmussen & Yaktine, 2009). According to our results, 60% of the pregnant women in our study cohort can either be classified as overweight or living with obesity before pregnancy, and more than 33% each of these groups of women gained excessive weight in pregnancy. These findings corroborate those of other national surveys (Li et al., 2018, 2019; Voerman et al., 2019): that high BMI is prevalent among women of reproductive age and remains a national health burden in Qatar. In this study prepregnancy BMI inversely correlated with GWG, among women with singleton pregnancies. Similar to IOM recommendations, women living with overweight and obesity generally gained less weight proportionally than did women classified as having underweight and normal weight. Similar findings were reported by Daemers et al., 2013; de Jersey et al., 2012 and Johansson et al., 2016. In addition, we also observed that higher maternal age, previous parity, and the presence of diabetes during pregnancy were also associated with decreased GWG. We suggest that this relationship may be partly explained by the previous contact that older, multiparous and diabetic women have had with the health system, which may have increased their awareness about weight and healthy lifestyles. In addition, older and multiparous pregnant women were more likely to have better awareness about achieving appropriate weight gain as a result of experiences with weight retention after previous pregnancies. Cheney et al. (Cheney et al., 2017), however, did not find an association between age and adequate GWG.
In our study, the overall proportion of women whose GWG exceeded IOM recommendations was 31%, and the prevalence of exceeding IOM recommendations for GWG was higher among women living with overweight and obesity, in comparison with those with normal or underweight. In several other studies, the proportion of women who gained more than the IOM recommendations ranged from 27% to more than 60% (Cheney et al., 2017; Brawarsky et al., 2005; Chasan-Taber et al., 2008; Daemers et al., 2013; de Jersey et al., 2012; Olson & Strawderman, 2003; Ferraro et al., 2012; Althuizen et al., 2009), and living with overweight or obesity was a significant predictor of excessive weight gain. However some studies showed that, GWG was most excessive among the overweight group in comparison to other BMI categories based on IOM recommendations (Chasan-Taber et al., 2008; Daemers et al., 2013; de Jersey et al., 2012; Althuizen et al., 2009; Stuebe et al., 2009; Restall et al., 2014). To explain the prevalence of excessive weight gain in women who are overweight or obese reported in the literature, Kominiarek and Peaceman suggested that it was possible that these groups of women required a more intensive form of health behavior program which was not obtainable in pregnancy given the: physiological adaptations that occur in pregnancy, reduced physical activity and the short interval between pregnancy and delivery for GWG goals to be achieved (Kominiarek & Peaceman, 2017).
Policy Implications
Pregnant women in Qatar have access to multidisciplinary care and management involving obstetricians, endocrinologists, diabetes educators, and nutritionists during pregnancy and the immediate postpartum period. Nevertheless, the current efforts to reduce rates of high BMI among women of reproductive age in Qatar must be sustained to reduce the associated health burden on these women and their offspring. Women living with overweight and obesity with excessive GWG could be at risk for postpartum weight retention and other fetal and maternal complications associated with excessive GWG and high BMI. Women living with obesity, both pregnant and nonpregnant, have access to health management in Qatar, but those classified as normal weight or overweight may not garner much attention and more likely to gain excessive weight during pregnancy, to retain more weight after delivery, and to become obese in the future.
In health care, pregnancy is an ideal time for clinicians to intervene in health matters relating to dietary habits, physical activity, and weight gain (WHO, 2017). The sustained interaction between pregnant women and the health sector throughout the antenatal and postpartum periods should therefore be an opportunity for enhanced, personalized, and integrated management for all pregnant women. Various tools such as counseling and dietary and lifestyle modifications can help pregnant women achieve adequate weight gain and minimize postpartum weight retention.
Strengths and Limitations
To our knowledge, this is the first examination of the association between BMI and GWG in Qatar in a large and representative sample. Measurement bias cannot be ruled out with regard to the height and weight measurements obtained from hospital records. In addition, the computation of BMI and GWG through self-reported prepregnancy weights is subject to measurement bias, given that women have been reported to underestimate their weights (Kominiarek & Peaceman, 2017). Although it has been shown that the difference is small and it can accurately represent BMI (Brunner Huber, 2007) and is sometimes the only feasible option available (Kominiarek & Peaceman, 2017). Another limitaion is that we did not disaggregate our data based on the various ethnicities of our study population despite questions in the literature on the applicability of BMI and IOM GWG cut-offs which had been derived from Western populations on non-Western populations.
Although the generalised linear model used in this analysis offers more flexibility and is easy to use; it is limited by its sensitivity to outliers and low predictive power. Despite all these limitations, hospital records are an invaluable resource for providing insight into health care practices. These hospital records contain information that inform the day-to-day care and management of patients. Our use of these records was therefore realistic, and according to our examination for selection bias, the findings were generalizable the population of women who gave birth to singleton infants within the study period.
Conclusion for Practice
A higher BMI was found to be significantly correlated with a lower GWG among women with singleton pregnancies in Qatar. Compared to women classifed as underweight or normal weight, more than one-third of women classified as overweight or obese had GWG that exceeded maximum recommendations. More efforts are needed to study and optimize the GWG pattern in the population of pregnant women in Qatar.
Data Availability
Due to institutional regulations, restrictions apply to the availability of data that support the findings of this study.
Code Availability
Not applicable
Abbreviations
- IOM:
-
Institute of Medicine
- GWG:
-
Gestational weight gain
- BMI:
-
Body mass index
- GDM:
-
Gestational diabetes mellitus
- DM:
-
Diabetes mellitus
References
Althuizen, E., van Poppel, M. N. M., Seidell, J. C., & van Mechelen, W. (2009). Correlates of absolute and excessive weight gain during pregnancy. Journal of Women’s Health, 18(10), 1559–1566.
Arora, P., & Tamber Aeri, B. (2019). Gestational weight gain among healthy pregnant women from Asia in comparison with Institute of Medicine (IOM) Guidelines-2009: a systematic review. Journal of Pregnancy, 2019, 3849596.
Brawarsky, P., Stotland, N. E., Jackson, R. A., Fuentes-Afflick, E., Escobar, G. J., Rubashkin, N., et al. (2005). Pre-pregnancy and pregnancy-related factors and the risk of excessive or inadequate gestational weight gain. International Journal of Gynaecology and Obstetrics, 91(2), 125–131.
Brunner Huber, L. R. (2007). Validity of self-reported height and weight in women of reproductive age. Maternal and Child Health Journal, 11(2), 137–144.
Chasan-Taber, L., Schmidt, M. D., Pekow, P., Sternfeld, B., Solomon, C. G., & Markenson, G. (2008). Predictors of excessive and inadequate gestational weight gain in hispanic women. Obesity (Silver Spring, Md.), 16(7), 1657–1666.
Cheney, K., Berkemeier, S., Sim, K. A., Gordon, A., & Black, K. (2017). Prevalence and predictors of early gestational weight gain associated with obesity risk in a diverse Australian antenatal population: A cross-sectional study. BMC Pregnancy and Childbirth, 17(1), 296.
Daemers, D. O. A., Wijnen, H. A. A., van Limbeek, E. B. M., Budé, L. M., & de Vries, R. G. (2013). Patterns of gestational weight gain in healthy, low-risk pregnant women without co-morbidities. Midwifery, 29(5), 535–541.
de Jersey, S. J., Nicholson, J. M., Callaway, L. K., & Daniels, L. A. (2012). A prospective study of pregnancy weight gain in Australian women. Australian and New Zealand Journal of Obstetrics and Gynaecology, 52(6), 545–551.
Ferraro, Z. M., Barrowman, N., Prud’homme, D., Walker, M., Wen, S. W., Rodger, M., et al. (2012). Excessive gestational weight gain predicts large for gestational age neonates Independent of maternal body mass index. Journal of Maternal-Fetal and Neonatal Medicine, 25(5), 538–542.
Haj Bakri, A., & Al-Thani, A. A. (2013). Chronic disease risk factor surveillance: Qatar STEPS report 2012 https://www.mdps.gov.qa/en/statistics/Surveys/STEPwise_Report.pdf. Accessed 5 May 2019.
Hernandez, D. C. (2012). Gestational weight gain as a predictor of longitudinal body mass index transitions among socioeconomically disadvantaged women. Journal of Women’s Health, 21(10), 1082–1090.
International Association of Diabetes in Pregnancy Study Group (IADPSG) Working Group on Outcome Definitions, Feig, D. S., Corcoy, R., Jensen, D. M., Kautzky-Willer, A., Nolan, C. J., et al. (2015). Diabetes in pregnancy outcomes: A systematic review and proposed codification of definitions. Diabetes/Metabolism Research and Reviews, 31(7), 680–690.
Johansson, K., Hutcheon, J. A., Stephansson, O., & Cnattingius, S. (2016). Pregnancy weight gain by gestational age and BMI in Sweden: A population-based cohort study. American Journal of Clinical Nutrition, 103(5), 1278–1284.
Kominiarek, M. A., & Peaceman, A. M. (2017). Gestational weight gain. American Journal of Obstetrics and Gynecology, 217(6), 642–651.
Li, C., Zhu, N., Zeng, L., Dang, S., Zhou, J., Pei, L., et al. (2018). Effect of maternal pre-pregnancy underweight and average gestational weight gain on physical growth and intellectual development of early school-aged children. Scientific Reports, 8(1), 12014.
Li, C., Zeng, L., Wang, D., Dang, S., Chen, T., Watson, V., et al. (2019). Effect of maternal pre-pregnancy BMI and weekly gestational weight gain on the development of infants. Nutrition Journal, 18(1), 6.
Ludwig, D. S., Rouse, H. L., & Currie, J. (2013). Pregnancy weight gain and childhood body weight: A within-family comparison. PLOS Medicine A Prentice (Ed), 10(10), e1001521.
National Health Authority (Qatar) (May 2018). Qatar Statistics Authority WHO (WHO). Qatar world health survey 2006 (2006). https://static-content.springer.com/esm/art%3A10.1186%2F1478-7954-12-18/MediaObjects/12963_2013_244_MOESM1_ESM.pdf. Accessed 6.
Olson, C. M., & Strawderman, M. S. (2003). Modifiable behavioral factors in a biopsychosocial model predict inadequate and excessive gestational weight gain. Journal of the American Dietetic Association, 103(1), 48–54.
Power, M. L., Lott, M. L., Mackeen, A. D., DiBari, J., & Schulkin, J. (2018). A retrospective study of gestational weight gain in relation to the Institute of Medicine’s recommendations by maternal body mass index in rural Pennsylvania from 2006 to 2015. BMC Pregnancy and Childbirth, 18(1), 239.
Qatar biobank Report (2016/2017). (2017). Doha, Qatar. http://www.qatarbiobank.org.qa/app/media/1730. Accessed 5 June 2019.
Rasmussen, K. M., & Yaktine, A. L. (Eds.). (2009). Weight gain during pregnancy: Reexamining the guidelines. The National Academies Press.
Restall, A., Taylor, R. S., Thompson, J. M. D., Flower, D., Dekker, G. A., Kenny, L. C., et al. (2014). Risk factors for excessive gestational weight gain in a healthy, nulliparous cohort. Journal of Obesity, 2014, 148391.
Siega-Riz, A. M., Viswanathan, M., Moos, M. K., Deierlein, A., Mumford, S., Knaack, J. (2009). A systematic review of outcomes of maternal weight gain according to the Institute of Medicine recommendations: birthweight, fetal growth, and postpartum weight retention. American Journal of Obstetrics and Gynecology, 201(4), 339.e1–339.14.
Sridhar, S. B., Darbinian, J., Ehrlich, S. F., Markman, M. A., Gunderson, E. P., Ferrara, A., et al. (2014). Maternal gestational weight gain and offspring risk for childhood overweight or obesity. American Journal of Obstetrics and Gynecology, 211(3), 259e1–259e8.
Sridhar, S. B., Xu, F., & Hedderson, M. M. (2016). In Krukowski (Ed.), Trimester-specific gestational weight gain and infant size for gestational age (11 vol.). PLOS ONE R. A. 7e0159500.
Stuebe, A. M., Oken, E., & Gillman, M. W. (2009). Associations of diet and physical activity during pregnancy with risk for excessive gestational weight gain. American Journal of Obstetrics and Gynecology, 201(1), 58.e1–58.e8.
Voerman, E., Santos, S., Patro Golab, B., Amiano, P., Ballester, F., Barros, H. (2019). Maternal body mass index, gestational weight gain, and the risk of overweight and obesity across childhood: An individual participant data meta-analysis. PLOS Medicine, 16(2), e1002744.
World Health Organization (Published 2006). WHO: global database on body mass index. BMI classification Retrieved from http://apps.who.int/bmi/index.jsp?introPage=intro_3.html. Accessed 14 May 2018.
World Health Organization (Published 2017). Obesity. Retrieved from http://www.who.int/features/factfiles/obesity/en/. Geneva: WHO. Accessed 14 May 2018.
Acknowledgements
Not applicable.
Funding
The PEARL-Peristat Registry (Perinatal Neonatal Outcomes Research Study in the Arabian Gulf) was funded by the Qatar National Research Fund, Grant no. NPRP 6-238-3-059. The funding organization played no role in the design, collection, analysis, interpretation of data, in the writing of the manuscript or in the decision to submit this manuscript for publication.
Open Access funding provided by the Qatar National Library.
Author information
Authors and Affiliations
Contributions
TO, HS, and SA designed the study and assisted with data analysis. TO, HS, SA, MA, and HA wrote the paper.
Corresponding author
Ethics declarations
Conflicts of interest
Authors state no conflict of interest.
Ethics Approval
The research complied with all the relevant regulations and institutional policies, was conducted in accordance with the tenets of the Helsinki Declaration, and was approved by the Hamad Medical Corporation Institutional Review Board. The registry study was granted with a waiver of consent for access and analysis of de-identified retrospective patient data.
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
10995_2023_3816_MOESM1_ESM.docx
Online Resource 1. Method used for computing gestational weight gain and prepregnancy body mass index (BMI). ANC, antenatal care; GA, gestational age.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Olukade, T., Salama, H., Al-Obaidly, S. et al. Maternal Body Mass Index and Recommended Gestational Weight Gain in a Middle Eastern Setting. Matern Child Health J 28, 524–531 (2024). https://doi.org/10.1007/s10995-023-03816-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10995-023-03816-z