Abstract
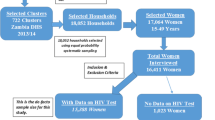
HIV counseling and voluntary testing during antenatal care have been proven to reduce the risk of HIV transmission from mother to child, through increasing knowledge about safe behaviors, ascertaining HIV status and increasing coverage of effective antiretroviral regimens. However, it remains that, in developing countries where 95 % of mother-to-child HIV transmissions (MTCT) take place, such interventions are not widely accessible or available. Using a nationally representative cross-sectional household survey, the present study aimed to examine individual- and contextual-level influences on the receipt of HIV pre-test counseling and uptake of HIV testing during the antenatal care period in Swaziland, a country highly burdened by HIV/AIDS. The study sample was restricted to women aged 15–49 years with a live birth in the past five years preceding the survey and who received antenatal care for the most recent birth. The findings of this study indicated that only 62 % of women received pre-test counseling for the prevention of MTCT and no more than 56 % of women consented to be tested for HIV during antenatal care. The multilevel regression analysis revealed that the likelihood of receiving HIV pre-test counseling increases significantly with higher parity, education level, household wealth and antenatal visits while it is lower in areas where poverty is pervasive (OR = 0.474) and in rural regions (OR = 0.598) as well. Beyond all the significant predictors, undergoing pre-test counseling has emerged as an important determinant of HIV testing. Receiving pre-test counseling increases the odds of accepting an HIV test by 77 %. Evidence from this analysis underscores bottlenecks and challenges that persist in increasing the need for and uptake of HIV preventive and treatment services to stop new HIV infections among children.
Similar content being viewed by others
References
UNAIDS. (2001b). Counselling and voluntary HIV testing for pregnant women in high HIV prevalence countries: Elements and issues. Retrieved October 2, 2012, from data.unaids.org/Publications/IRC-pub01/jc245-couns_test_en.pdf.
WHO, UNAIDS, UNICEF. (2011). Global HIV/AIDS response-Epidemic update and health sector progress towards universal access. Retrieved October 2, 2012, from http://www.unaids.org/en/media/unaids/contentassets/documents/unaidspublication/2011/20111130_UA_Report_en.pdf.
UNICEF. (2012). Countdown to zero: Elimination of new HIV infections among children by 2015 and keeping their mothers alive. Retrieved October 2, 2012, from http://www.unicef.org/aids/files/hiv_pmtctfactsheetSwaziland.pdf.
UNAIDS. (2010). Globla report: UNAIDS report on the global AIDS epidemic 2010. Retrieved October 2, 2012, from http://www.unaids.org/documents/20101123_globalreport_em.pdf.
UNAIDS. (2012a). Swaziland country report on monitoring the political declaration on HIV and AIDS. Retrieved October 2, 2012, from http://www.unaids.org/en/dataanalysis/knowyourresponse/countryprogressreports/2012countries/ce_SZ_Narrative_Report%5B1%5D.pdf.
Dabis, F., & Ekpini, E. R. (2002). HIV-1/AIDS and maternal and child health in Africa. The Lancet, 359, 2097–2104.
Bassett, M. T. (2001). Keeping the M in MTCT: Women, mothers, and HIV prevention. American Journal of Public Health, 91, 701–703.
UNAIDS. (2001a). The impact of voluntary counseling and testing: The global review of the benefits and challenges. Retrieved October 2, 2012, from http://data.unaids.org/Publications/IRC-pub02/jc580-vct_en.pdf.
Karamagi, C. A. S., Tumwine, J. K., Thorkild, T., & Heggenhougen, K. (2006). Antenatal HIV testing in rural eastern Uganda in 2003: Incomplete rollout of the prevention of mother-to-child transmission of HIV programme? Retrieved October 2, 2012 from http://www.biomedcentral.com/1472-698X/6/6.
Temmerman, M., Quaghebeur, A., Mwanyumba, F., & Mandaliya, K. (2003). Mother-to-child HIV transmission in resource poor settings: How to improve coverage? Aids, 17, 1239–1242.
Hardon, A., Vernooij, E., Bongololo-Mbera, G., Cherutich, P., Desclaux, A., Kyaddondo, D., et al. (2012). Women’s views on consent, counseling and confidentiality in PMTCT: a mixed-methods study in four African countries. BMC Public Health, 2012, 26.
Fanta, W., & Worku, A. (2012). Determinants for refusal of HIV testing among women attending for antenatal care in Gambella Region, Ethiopia. Retrieved October 2, 2012 from http://www.reproductive-health-journal.com/content/9/1/8.
Pool, R., Nyanzi, S., & Whitworth, J. G. (2001). Attitudes to voluntary counselling and testing for HIV among pregnant women in rural south-west Uganda. AIDS Care, 13, 605–615.
Holmes, C., Preko, P., Bolds, R., Baidoo, J., & Jolly, P. (2008). Acceptance of voluntary counselling, testing and treatment for HIV among Pregnant Women in Kumasi Ghana. Ghana Medical Journal, 42, 8–15.
Bassett, M. T. (2002). Ensuring a public health impact of programs to reduce HIV transmission from mothers to infants: The place of voluntary counseling and testing. American Journal of Public Health, 92, 347–351.
Eide, M., Myhre, M., Lindbaek, M., Sundby, J., Arimi, P., & Thior, I. (2006). Social consequences of HIV-positive women’s participation in prevention of mother-to-child transmission programmes. Patient Education and Counseling, 60, 146–151.
Kilewo, C., Massawe, A., Lyamuya, E., Semali, I., Kalokola, F., Urassa, E., et al. (2001). HIV counseling and testing of pregnant women in sub-Saharan Africa—Experiences from a study on prevention of mother-to-child HIV-1 transmission in Dar es Salaam, Tanzania. Journal of Acquired Immune Deficiency Syndromes, 28, 458–462.
Rutenberg, N., Baek, C., Kalibala, S., & Rosen, J. (2003). Evaluation of United Nations-supported pilot projects for the prevention of mother-to-child transmission of HIV: Overview of findings. Retrieved October 2, 2012, from http://www.unicef.org/evaldatabase/files/Global_2003_UN_Supported_PMTCT_Projects.pdf.
Baiden, F., Remes, P., Baiden, R., Williams, J., Hodgson, A., Boelaert, M., et al. (2005). Voluntary counseling and HIV testing for pregnant women in the Kassena–Nankana district of northern Ghana: Is couple counseling the way forward? AIDS Care, 17, 648–657.
Fylkesnes, K., Haworth, A., Rosensvard, C., & Kwapa, P. M. (1999). HIV counseling and testing: Over- emphasizing high acceptance rates as a threat to confidentiality and the right not to know. Aids, 13, 2469–2474.
Fabiani, M., Cawthorne, A., Nattabi, B., Ayella, E. O., Ogwang, M., & Declich, S. (2007). Investigating factors associated with uptake of HIV voluntary counselling and testing among pregnant women living in North Uganda. Aids Care-Psychological and Socio-Medical Aspects of Aids/Hiv, 19, 733–739.
de Paoli, M. M., Manongi, R., & Klepp, K. I. (2004). Factors influencing acceptability of voluntary counselling and HIV-testing among pregnant women in Northern Tanzania. Aids Care-Psychological and Socio-Medical Aspects of Aids/Hiv, 16, 411–425.
Painter, T. M. (2001). Voluntary counseling and testing for couples: A high-leverage intervention for HIV/AIDS prevention in sub-Saharan Africa. Social Science and Medicine, 53, 1397–1411.
Turan, J. M., Bukusi, E. A., Onono, M., Holzemer, W. L., Miller, S., & Cohen, C. R. (2011). HIV/AIDS stigma and refusal of HIV testing among pregnant women in rural Kenya: Results from the MAMAS Study. AIDS Behavior, 15, 1111–1120.
Kroeger, A. (1983). Anthropological and socio-medical health care research in developing countries. Social Science and Medicine, 17, 147–161.
Andersen, R. M. (1995). Revisiting the behavioral model and access to medical care: Does it matter? Journal of Health and Social Behavior, 36, 1–10.
Central Statistical Office. (CSO) [Swaziland] (2008). Macro International Inc. Swaziland Demographic and Health Survey 2006–2007. In: Mbabane, Swaziland. Calverton, MD: Central Statistical Office and Macro International Inc.
Donabedian, A. (1980). Exploration in quality assessment and monitoring: The definition of quality and approaches to its management (vol. 1). Ann Arbor, MA: Health Administration Press.
Donabedian, A. (1986). Criteria and standards for quality assessment and monitoring. Quality Review Bulletin, 3, 99–108.
Rosenstock, I. M., Strecher, V. J., & Becker, M. (1994). The health belief model and HIV risk behavior change. In R. J. DiClemente, & J. L. Peterson E. (Eds.), Preventing AIDS: Theories and methods of behavioral interventions (pp. 5–24). New York: Plenum Press.
Strecher, V. J., & Rosenstock, I. M. (1997). The health belief model. In K. L. F. Glanz, & B. K. Rimer (Eds.), Health behavior and health education: Theory, research and practice (pp. 41–59). San Francisco: Jossey-Bass.
Stephenson, R., Elfstrom, K. M., & Winter, A. (2013). Community influences on married men’s uptake of HIV testing in eight African Countries. AIDS Behavior, 17, 2352–2366.
Goldstein, H. (2003). Multilevel Statistical Models. London: Edward Arnold.
StataCorp. (2011). Stata statistical software: Release 12. College Station, TX: StataCorp LP.
UNAIDS. (2012b). Together we will end AIDS. Retrieved December 21, 2012, from http://www.unaids.org/en/media/unaids/contentassets/documents/epidemiology/2012/jc2296_unaids_togetherreport_2012_en.pdf.
Homsy, J., King, R., Malamba, S. S., Opio, C., Okallany, A., Kalamya, J. N., et al. (2007). The need for partner consent is a main reason for opting out of routine HIV testing for prevention of mother-to-child transmission in a rural Ugandan Hospital. Journal of Acquired Immune Deficiency Syndromes, 44, 366–369.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sagna, M.L., Schopflocher, D. HIV Counseling and Testing for the Prevention of Mother-to-Child Transmission of HIV in Swaziland: A Multilevel Analysis. Matern Child Health J 19, 170–179 (2015). https://doi.org/10.1007/s10995-014-1507-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10995-014-1507-y