Abstract
Central hypovolemia is accompanied by hemodynamic compensatory responses. Understanding the complex systemic compensatory responses to altered hemodynamic patterns during conditions of central hypovolemia—as induced by standing up and/or lower body negative pressure (LBNP)—in humans are important. LBNP has been widely used to understand the integrated physiological responses, which occur during sit to stand tests (orthostasis), different levels of hemorrhages (different levels of LBNP simulate different amount of blood loss) as well as a countermeasure against the cephalad fluid shifts which are seen during spaceflight. Additionally, LBNP application (used singly or together with head up tilt, HUT) is useful in understanding the physiology of orthostatic intolerance. The role seasonal variations in hormonal, autonomic and circulatory state play in LBNP-induced hemodynamic responses and LBNP tolerance as well as sex-based differences during central hypovolemia and the adaptations to exercise training have been investigated using LBNP. The data generated from LBNP studies have been useful in developing better models for prediction of orthostatic tolerance and/or for developing countermeasures. This review examines how LBNP application influences coagulatory parameters and outlines the effects of temperature changes on LBNP responses. Finally, the review outlines how LBNP can be used as innovative teaching tool and for developing research capacities and interests of medical students and students from other disciplines such as mathematics and computational biology.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
We subject our body to orthostatic challenge every time we stand up (Blaber et al. 2011; Goswami et al. 2015). During active standing, however, the exact potential of the compensatory responses of cardiovascular system may not be revealed. During intensive stress situations (e.g. exercise, diving, disease states or microgravity), the cardiovascular system shows its full potential and reveals cardiovascular regulatory features of physiological systems that otherwise might not be observable. Under certain occasions, there could be a decrease in cerebral perfusion to critical levels thus leading to syncope (Gao et al. 2008; Goswami et al. 2012). Intensive central hypovolemia can be experimentally induced via passive head up Tilt (HUT) and/or lower body negative pressure (LBNP) or a combination of both HUT + LBNP (Arbeille and Herault 1998; Cvirn et al. 2012). Negative suction pressure application on the lower body via a seal at anterior superior iliac spine causes caudal shifts in the blood and leads to a decreased venous return, and consequently, central hypovolemia (Baisch 1993; Balldin et al. 1996; Goswami et al. 2009a, b, c). During central hypovolemia, inhibitory effects of arterial and cardiopulmonary receptors on the central sympathetic system are removed leading to increased sympathetic activity (Barcroft et al. 1944), which ensure adequate cerebral perfusion and maintenance of blood pressure.
Some of the uses of LBNP include draining blood away from diseased organs, as a cardiovascular deconditioning prevention countermeasure (Batzel et al. 2009), for the study of hemorrhage induced responses (Cvirn et al. 2019). It is used in orthopedic rehabilitation, as it creates footward loading (detailed in Goswami et al. 2008, 2019a, b). In spaceflight, LBNP has been used to counter the headward shift of body fluids and to load the musculoskeletal system in spaceflight as it occurs on Earth. LBNP has been used for evaluation of responses to different therapeutic agents as well as to varying perturbations (e.g. across seasons and/or varying skin temperatures) and to investigate how the LBNP-induced responses vary across the sexes. For detailed effects of the LBNP on cardiovascular reflexes, please see (Bevegard et al. 1977; Bennett 1987; Balldin et al. 1996; Beske et al. 2001; Goswami et al. 2008, 2019a, b).
Systemic effects of LBNP
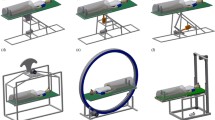
LBNP is usually, though not always, applied to persons in the supine position, without skeletal muscle activity to minimize motion artifacts (Bennett 1987; Baisch 1993; Balldin et al. 1996). It can also be applied in exercising subjects (Hargens et al. 1991). Moreover, as this procedure does not require body position changes, it isolates the reflexes associated with change in the posture from supine to upright standing and also removes movement artifacts from the hemodynamic recordings.
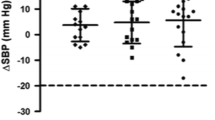
Understanding cardiovascular responses to orthostatic challenge is largely based on the measurement of cardiac output, heart rate and lower limb venous compliance responses. LBNP elicits reproducible reflexive hemodynamic responses which maintain adequate heart and cerebral perfusion (Blaber et al. 2013) during the caudal fluid shifts. In comparing LBNP with centrifuge exposure for selecting pilot candidates, it was reported that the latter was more stressful than LBNP and that LBNP could be used as a convenient screening test to assess tolerance to central hypovolemia (Blaber et al. 2013).
Additional effects of the LBNP on different systems include on cerebral, autonomic, coagulation, pulmonary systems and hormones (Bevegard et al. 1977; Bennett 1987; Bertinieri et al. 1988; Berdeaux et al. 1992; Baisch 1993; Balldin et al. 1996; Beske et al. 2001). For instance, forearm muscle sympathetic activity doubles at − 60 mmHg LBNP (Haditsch et al. 2015; Roessler et al. 2011; Verma et al. 2017; Patel et al. 2016). Specific neurohormonal responses during LBNP are as follows (Blomqvist and Stone 1983): Adrenomedullin, adrenocorticotropic hormone (ACTH), prolactin and multifunctional neuropeptides such as galanin and atrial natriuretic peptide (ANP) rise as the central hypovolemia increases. Hypothalamic-pituitary components, such as vasopressin, are subsequently elevated with some delay, followed by several fold increases at presyncope (Hinghofer-Szalkay et al. 2011).
LBNP and its potential effects on coagulation
LBNP application leads to hemoconcentration and elevations in blood viscosity and plasma proteins. That is, LBNP shifts the blood towards a more prothrombotic state (Zaar et al. 2009, 2014; van Helmond et al. 2015). Applying − 30 mmHg LBNP to healthy participants for about 10 min was shown to increase thrombin anti-thrombin (TAT) complex levels to those that occur during deep venous thrombosis (Zaar et al. 2009). Another study compared the effects of − 45 mmHg LBNP with blood loss of up to 1000 ml and concluded that coagulation changes are similar in both cases (van Helmond et al. 2015). The authors speculated that perhaps it was the accompanying elevations in sympathetic output—seen both in LBNP and bleeding—which could increase the tendency towards clot formation (372). This is not surprising, since it is known that trauma/ rupture to a vessel is accompanied by an increase in thrombosis, which, consequently, reduces exsanguination risk (van Helmond et al. 2015).
Even an increase in coagulation has been seen in healthy participants as they develop presyncopal signs and symptoms during LBNP (Cvirn et al. 2012). Cvirn et al. reported that the LBNP induced changes in hemoconcentration, blood viscosity and the plasma volume losses, and the increase in vasopressin at presyncope, could potentially contribute towards increases in endothelial activation markers (tissue factor, TF, and tissue plasminogen activator, TPA) as well as in thrombin generation parameters (thrombin-antithrombin complexes and prothrombin fragments 1 and 2). As vasopressin levels have been shown to be associated with increases in platelet aggregation and agglutination (Zaar et al. 2014), it could contribute significantly towards the increased coagulation seen at presyncope (Filep and Rosenkranz 1987).
Aspects to consider when using LBNP
In addition to the types of LBNP protocol used (e.g. step vs ramp protocol), following aspects must be considered when applying LBNP:
Magnitude and duration of LBNP suction application
Depending on the magnitude of suction, LBNP induced vascular pooling in the legs leads to decreases in venous return, central venous pressure, and stroke volume (Baisch 1993; Balldin et al. 1996). The onset and the degree of hypotension during central hypovolemia induced by LBNP also varies between participants’ (Bennett 1987; Baisch 1993; Balldin et al. 1996). It has been reported that − 20 mmHg LBNP application for 5 min leads to 500–1000 ml fluid displacement towards the peripheral vascular compartments (Baisch 1993; Balldin et al. 1996).
LBNP also causes an increase in total peripheral resistance; this is dependent on the magnitude of LBNP applied. Low levels of LBNP cause increases in sympathetic tone leading to vasoconstriction in the forearm and in the splanchnic area (Blaber et al. 2013). High LBNP levels (e.g. − 60 mmHg) lead primarily to renal vasoconstriction, decreases in glomerular filtration rate, renal plasma flow and urine production (see Baisch 1993; Balldin et al. 1996).
LBNP magnitude and its influence on regional blood flows
It has been reported that LBNP above − 20 mmHg leads to differential blood distribution across the body compartments (detailed in Baisch 1993; Balldin et al. 1996)). Additionally, changing the LBNP from − 20 to − 40 mmHg causes leg volume to more than double; this leg pooling occurs exclusively in the venous vasculature. It has also been reported that at − 50 mmHg LBNP, women show larger pelvic blood pooling as compared to men (Bronzwaer et al. 2017).
The splanchnic vascular bed, which constitutes a major blood reserve, provides majority of regional vascular conductance, which helps in blood pressure maintenance central hypovolemia (Blaber et al. 2013; Hinghofer-Szalkay et al. 2008). LBNP of − 50 mmHg leads to a up to 1/3rd reduction in blood flow in the splanchnic area. In addition, due to the accompanying increased sympathetic activity, splanchnic blood flow continues to reduce as suction pressure is elevated (Brown et al. 1966).
LBNP sealing location
LBNP induced responses depend also the position of the seal application. The LBNP sealing on its own modulates distribution of blood volume and perfusion of the liver even before commencement of the suction (Goswami et al. 2009a, b, c). During application of LBNP, different effects are seen when the LBNP seal is applied at different locations. For instance, when LBNP is applied at the upper abdomen—which includes the splanchnic region in the suction area—in contrast to the default LBNP seal at Iliac crest, larger drops in central blood volume and splanchnic blood flow occur. Upper sealing position also leads to greater compensatory elevations in heart rate (Goswami et al. 2009a, b, c).
Influence of confounding variables
When carrying out LBNP studies, aspects related to subject selection criteria (e.g. sex, height, age, fitness levels), environmental conditions (e.g. seasons, temperature of the skin, time of the day, fasting or non-fasting state), and in-laboratory conditions (room temperature, humidity, noise) should be considered.
Influence of temperature changes on LBNP responses
As changes in environmental temperature lead to changes in the generalized systemic responses, it is not surprising that LBNP tolerance is influenced by changes in temperature. Just as greater incidence of collapse and syncope during the hot seasons is reported (Goswami et al. 2017), exposure to heat decreases the LBNP tolerance while cold stress has been reported to increase it (Crandall 2000). LBNP tolerance, however, varies considerably between persons exposed to heat (Lee et al. 2013). Several factors such as skin temperature and/or venous compliance changes could contribute towards differences in LBNP tolerance during different temperature changes. These are now discussed in detail:
Skin temperature could influence both reflex vasoactive state of the skin and the direct local control in the skin (Wolthuis et al. 1974). Local changes in temperature on the skin could also influence the tolerance times (Charkoudian et al. 2002). For instance, heat application activates the cutaneous vasodilator system in resting humans and reduces LBNP tolerance while skin cooling improves LBNP tolerance (Wolthuis et al. 1974; Shibasaki et al. 2006). Skin cooling has been reported to be associated with increased sympathetic activity (Durand et al. 2004) and central venous pressure (Cui et al. 2005) as well as peripheral vasoconstriction.
Venous compliance changes during alterations in temperature, and the potential reductions in cerebral perfusion, have been postulated as contributing factors to reduced LBNP tolerance (Tripathi et al. 1984; Tripathi and Nadel 1986; Wilson et al. 2006). A study assessed Frank-Starling relationship with temperature changes and it was observed that heating leads to a downward shift of the operating point to a steeper portion of a Frank-Starling curve while cooling was associated with an upward shift to a flatter portion of the curve (Crandall 2000; Wilson et al. 2009). The Frank-Starling relationship during LBNP could also be influenced by heart rate, venous return, peripheral resistance and compliance (Wilson et al. 2009). The effects of whole-body heating and cooling on cardiovascular responses are presented in greater details in the elegant review of Wilson and Crandall (2011).
LBNP as a teaching tool
Not only is LBNP a useful tool for demonstrating hemodynamic responses to central hypovolemia to students (Goswami et al. 2011, 2013), the recorded responses can be used for teaching optimization and physiological control loops to students from other disciplines, such as mathematics (Batzel et al. 2012; Etter el al. 2011). However, a big limitation of this measurement technique is that a careful monitoring of the volunteers during LBNP suction application is required. Not only is there a wide variability in the tolerance to LBNP application (Goswami et al. 2009a, b, c) but developmental of presyncopal signs and symptoms—a termination criteria for the study—can occur anytime in any of the volunteers (Goswami et al. 2021).
We have, therefore, recently investigated an innovative teaching approach: the “dry lab” approach (Goswami et al. 2021). In laboratories where there is no LBNP box available or there is lack of medical staff to monitor the study participants, a “dry lab” activity can be employed. This activity involves providing students with a review paper on LBNP, with which students can understand the usage of LBNP, identify issues/ confounding variables when carrying out LBNP experiments, and also how to interpret data from LBNP studies. For the latter activity, students are presented with hemodynamic data that have been collected during LBNP application. For instance, during graded LBNP (Blaber et al. 2013), across the sexes (Cvirn et al. 2019), at presyncope (Grasser et al. 2009a, b), and with interventions (e.g. mental arithmetic: Goswami et al. 2013); heat application (Wilson and Crandall 2011), amongst others.
Overall, it appears that our “dry lab” activity using LBNP to teach physiology exposes students even early in their medical studies and across disciplines to the basics of systems physiology and introduces them to experimental research. For example, providing insight into research includes formulation of a research question, designing (including, consideration of confounding variables), conducting, implementing and interpreting experimental data.
Conclusions and recommendations
LBNP induces responses (cardiovascular and hormonal), which vary widely across persons. When carrying out LBNP studies, confounding variables such as selection criteria, LBNP protocol to be used and the laboratory- and environmental—conditions should be carefully accounted for. The call out box summarizes the potential changes in coagulation that could occur during LBNP as well as how temperature changes during LBNP application influence the physiological responses.
LBNP induced effects on coagulation Hemoconcentration and plasma volume losses Elevations in blood viscosity and plasma proteins which predispose towards a pro-coagulant state Increases in endothelial activation markers (tissue factor, TF, and tissue plasminogen activator, TPA) as well as in thrombin generation parameters (thrombin-antithrombin complexes and prothrombin fragments 1 and 2) Increases in platelet aggregation and agglutination Accompanying elevations in sympathetic output—seen both in LBNP and bleeding—which could increase the tendency towards clot formation in both LBNP and bleeding Effects of temperature changes on LBNP induced responses LBNP tolerance is influenced by changes in temperature Heat decreases the LBNP tolerance while cold stress increases it Local changes in temperature on the skin could also influence the tolerance times Heat application activates the cutaneous vasodilator system and reduces LBNP tolerance while skin cooling improves LBNP tolerance Venous compliance changes during alterations in temperature Decreases in cerebral blood flow during increased temperature |
References
Arbeille P, Herault S (1998) Cardiovascular echographic and Doppler parameters for the assessment of orthostatic intolerance. Eur J Ultrasound 7(1):53–71
Baisch FJ (1993) Body fluid distribution in man in space and effect of lower body negative pressure treatment. Clin Investig 71(9):690–699
Balldin UI, Krock LP, Hopper NL, Squires WG (1996) Cerebral artery blood flow velocity changes following rapid release of lower body negative pressure. Aviat Space Environ Med 67(1):19–22
Barcroft H, Edholm OG, Mcmichael J, Sharpey-Schafer EP (1944) Post haemorrhagic fainting study bz cardiac output and forearm flow. The Lancet 243:489–522
Batzel JJ, Goswami N, Lackner HK, Roessler A, Bachar M, Kappel F, Hinghofer-Szalkay H (2009) Patterns of cardiovascular control during repeated tests of orthostatic loading. Cardiovasc Eng 9(4):134–143
Batzel JJ, Hinghofer-Szalkay H, Kappel F, Schneditz D, Kenner T, Goswami N (2012) Bridging different perspectives of the physiological and mathematical disciplines. Adv Physiol Educ 36(4):265–74
Bennett T (1987) Cardiovascular responses to central hypovolaemia in man: physiology and pathophysiology. Physiologist 30(1 Suppl):S143-146
Berdeaux A, Duranteau J, Pussard E, Edouard A, Giudicelli JF (1992) Baroreflex control of regional vascular resistances during simulated orthostatism. Kidney Int Suppl 37:S29–S33
Bertinieri G, Di Rienzo M, Cavallazzi A, Ferrari AU, Pedotti A, Mancia G (1988) Evaluation of baroreceptor reflex by blood pressure monitoring in unanesthetized cats. Am J Physiol 254:377–383
Beske SD, Alvarez GE, Ballard TP, Davy KP (2001) Gender difference in cardiovagal baroreflex gain in humans. J Appl Physiol 91(5):2088–2092
Bevegard S, Castenfors J, Lindblad LE, Tranesjo J (1977) Blood pressure and heart rate regulating capacity of the carotid sinus during changes in blood volume distribution in man. Acta Physiol Scand 99(3):300–312
Blaber AP, Goswami N, Bondar RL, Kassam MS (2011) Impairment of cerebral blood flow regulation in astronauts with orthostatic intolerance after flight. Stroke 42(7):1844–1850
Blaber A, Hinghofer-Szalkay H, Goswami N (2013) Blood volume redistribution during hypovolemia. Aviat Space Environ Med 84:59–64
Blomqvist CG, Stone HL (1983) Cardiovascular adjustments to gravitational stress. In: Shepherd JT, Abboud FM, Geiger SR (eds) Handbook of physiology. The Cardiovascular system. Peripheral circulation and organ blood flow. American Physiological Society, Bethesda, pp 025–063
Bronzwaer AG, Verbree J, Stok WJ, Daemen MJ, van Buchem MA, van Osch MJ, van Lieshout JJ (2017) The cerebrovascular response to lower-body negative pressure vs. head-up tilt. J Appl Physiol 122(4):877–883
Brown E, Goei JS, Greenfield AD, Plassaras GC (1966) Circulatory responses to simulated gravitational shifts of blood in man induced by exposure of the body below the iliac crests to sub-atmospheric pressure. J Physiol 183(3):607–627
Charkoudian N, Eisenach JH, Atkinson JL, Fealey RD, Joyner MJ (2002) Effects of chronic sympathectomy on locally mediated cutaneous vasodilation in humans. J Appl Physiol 92(2):685–690
Crandall CG (2000) Carotid baroreflex responsiveness in heat-stressed humans. Am J Physiol-Heart Circul Physiol 279(4):H1955–H1962
Cui J, Durand S, Levine BD, Crandall CG (2005) Effect of skin surface cooling on central venous pressure during orthostatic challenge. Am J Physiol Heart Circ Physiol 289(6):H2429-2433
Cvirn G, Schlagenhauf A, Leschnik B, Koestenberger M, Roessler A, Jantscher A, Vrecko K, Juergens G, Hinghofer-Szalkay H, Goswami N (2012) Coagulation changes during presyncope and recovery. PLoS One 7(8):e42221
Cvirn G, Waha JE, Brix B, Rössler A, Jantscher A, Schlagenhauf A, Koestenberger M, Wonisch W, Wagner T, Goswami N (2019) Coagulation changes induced by lower-body negative pressure in men and women. J Appl Physiol 126(5):1214–1222
Durand S, Cui J, Williams KD, Crandall CG (2004) Skin surface cooling improves orthostatic tolerance in normothermic individuals. Am J Physiol Regul Integr Comp Physiol 286(1):R199-205
Etter KE, Goswami N, Sharp MK (2011) Modelling of cardiovascular response to graded orthostatic stress: role of capillary filtration. Eur J Clin Invest 41(8):807–819
Filep J, Rosenkranz B (1987) Mechanism of vasopressin-induced platelet aggregation. Thromb Res 45:7–15
Gao Y, Goswami N, Grasser E, Rössler A, Stöger E, Schwaberger G, Hinghofer-Szalkay HG (2008) Radix astragali and orthostatic response: a double-masked crossover study. Aviat Space Environ Med 79(2):94–98
Goswami N, Loeppky JA, Hinghofer-Szalkay HG (2008) LBNP: past protocols and technical considerations for experimental design. Aviat Space Environ Med 79:459–471
Goswami N, Roessler A, Lackner HK, Schneditz D, Grasser E, Hinghofer-Szalkay HG (2009a) Heart rate and stroke volume response patterns to augmented orthostatic stress. Clin Auton Res 19(3):157–165
Goswami N, Grasser E, Roessler A, Schneditz D, Hinghofer-Szalkay HG (2009b) The cardiovascular response to lower body negative pressure in humans depends on seal location. Physiol Res 58:311–318
Goswami N, Lackner HK, Grasser EK, Hinghofer-Szalkay HG (2009c) Individual stability of orthostatic tolerance response. Acta Physiol Hung 96:157–166
Goswami N, Batzel JJ, Loeppky JA, Hinghofer-Szalkay H (2011) Teaching fluid shifts during orthostasis using a classic paper by Foux et al. Adv Physiol Educ. 35(4):330–335
Goswami N, Roessler A, Hinghofer-Szalkay HG, Montani JP, Steptoe A (2012) Delaying orthostatic syncope with mental challenge: a pilot study. Physiol Behav 106:569–573
Goswami N, Batzel JJ, Clément G, Stein TP, Hargens AR, Sharp MK, Blaber AP, Roma PG, Hinghofer-Szalkay HG (2013) Maximizing information from space data resources: a case for expanding integration across research disciplines. Eur J Appl Physiol 113:1645–1654
Goswami N, Evans J, Schneider S, von der Wiesche M, Mulder E, Rössler A, Hinghofer-Szalkay H, Blaber AP (2015) Effects of individualized centrifugation training on orthostatic tolerance in men and women. PLoS One 10:e0125780-e0125780
Goswami N, Blaber AP, Hinghofer-Szalkay H, Montani JP (2017) Orthostatic intolerance in older persons: etiology and countermeasures. Front Physiol 8:803
Goswami N, Blaber AP, Hinghofer-Szalkay HG, Convertino VA (2019a) Lower body negative pressure: physiological effects, applications, and implementation. Physiol Rev 99(1):807–851
Goswami N, Reichmuth J, Di Mise A, Brix B, Roessler A, Centrone M, Ranieri M, Russo A, De Santo NG, Tamma G, Sasso FC, Valenti G (2019b) Comparison between men and women of volume regulating hormones and aquaporin-2 excretion following graded central hypovolemia. Eur J Appl Physiol 119(3):633–643
Goswami N, Singh A, Deepak KK (2021) Developing a “dry lab” activity using lower body negative pressure to teach physiology. Adv Physiol Educ 45(3):445–453
Grasser EK, Goswami N, Hinghofer-Szalkay HG (2009a) Presyncopal cardiac contractility and autonomic activity in young healthy males. Physiol Res 58:817–826
Grasser EK, Goswami N, Roessler A, Vrecko CK, Hinghofer-Szalkay HG (2009b) Hemodynamic and neurohormonal responses to extreme orthostatic stress in physically fit young adults. Acta Astronaut 64:688–696
Haditsch B, Roessler A, Krisper P, Frisch H, Hinghofer-Szalkay HG, Goswami N (2015) Volume regulation and renal function at high altitude across gender. PLoS ONE 10(3):e0118730
Hargens AR, Whalen RT, Watenpaugh DE, Schwandt DF, Krock LP (1991) Lower body negative pressure to provide load bearing in space. Aviat Space Environ Med 62(934–937):1991
Hinghofer-Szalkay HG, Goswami N, Rössler A, Grasser E, Schneditz D (2008) Reactive hyperemia in the human liver. Am J Physiol Gastrointest Liver Physiol 295(2):G332–G337
Hinghofer-Szalkay H, Lackner HK, Rössler A, Narath B, Jantscher A, Goswami N (2011) Hormonal and plasma volume changes after presyncope. Eur J Clin Invest 41:1180–1185
Lee JF, Harrison ML, Brown SR, Brothers RM (2013) The magnitude of heat stress-induced reductions in cerebral perfusion does not predict heat stress-induced reductions in tolerance to a simulated hemorrhage. J Appl Physiol 114:1492
Patel K, Rössler A, Lackner HK, Trozic I, Laing C, Lorr D, Green DA, Hinghofer-Szalkay H, Goswami N (2016) Effect of postural changes on cardiovascular parameters across gender. Medicine 95(28):e4149
Roessler A, Goswami N, Haditsch B, Loeppky JA, Luft FC, Hinghofer-Szalkay HG (2011) Volume regulating hormone responses to repeated head-up tilt and lower body negative pressure. Eur J Clin Invest 41:863–869
Shibasaki M, Davis SL, Cui J, Low DA, Keller DM, Durand S, Crandall CG (2006) Neurally mediated vasoconstriction is capable of decreasing skin blood flow during orthostasis in the heat stressed human. J Physiol 575(3):953–959
Tripathi A, Nadel ER (1986) Forearm skin and muscle vasoconstriction during lower body negative pressure. J Appl Physiol 60(5):1535–1541
Tripathi A, Shi X, Wenger CB, Nadel ER (1984) Effect of temperature and baroreceptor stimulation on reflex venomotor responses. J Appl Physiol 57(5):1384–1392
van Helmond N, Johnson BD, Curry TB, Cap AP, Convertino VA, Joyner MJ (2015) Coagulation changes during lower body negative pressure and blood loss in humans. Am J Physiol Heart Circ Physiol 309(9):H1591-1597
Verma AK, Xu D, Garg A, Cote AT, Goswami N, Blaber AP, Tavakolian K (2017) Non-linear heart rate and blood pressure interaction in response to lower-body negative pressure. Front Physiol 8(20):767–777
Wilson TE, Crandall CG (2011) Effect of thermal stress on cardiac function. Exerc Sport Sci Rev 39:12
Wilson TE, Cui J, Zhang R, Crandall CG (2006) Heat stress reduces cerebral blood velocity and markedly impairs orthostatic tolerance in humans. Am J Physiol Regul Integr Comp Physiol. 291(5):R1443–R1448
Wilson TE, Brothers RM, Tollund C, Dawson EA, Nissen P, Yoshiga CC, Jons C, Secher NH, Crandall CG (2009) Effect of thermal stress on Frank-Starling relations in humans. J Physiol 587:3383–3392
Wolthuis RA, Bergman SA, Nicogossian AE (1974) Physiological-effects of locally applied reduced pressure in man. Physiol Rev 54(3):566–595
Zaar M, Johansson PI, Nielsen LB, Crandall CG, Shibasaki M, Hilsted L, Secher NH (2009) Early activation of the coagulation system during lower body negative pressure. Clin Physiol Funct Imaging 29(6):427–430
Zaar M, Fedyk CG, Pidcoke HF, Scherer MR, Ryan KL, Rickards CA, Hinojosa-Laborde C, Convertino VA, Cap AP (2014) Platelet activation after presyncope by lower body negative pressure in humans. PLoS ONE 9(12):e116174
Acknowledgements
I wish to thank Dr. Bianca Brix, Medical University of Graz, Austria for her essential help in preparing the manuscript.
Funding
Open access funding provided by Medical University of Graz.
Author information
Authors and Affiliations
Contributions
The manuscript was conceptualised, written and edited by NG.
Corresponding author
Ethics declarations
Competing interests
The author declares no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Goswami, N. Compensatory hemodynamic changes in response to central hypovolemia in humans: lower body negative pressure: updates and perspectives. J Muscle Res Cell Motil 44, 89–94 (2023). https://doi.org/10.1007/s10974-022-09635-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10974-022-09635-z