Abstract
Objectives
Previously, we reported that an inpatient multimodal occupational rehabilitation program (I-MORE) was more effective than outpatient Acceptance and Commitment Therapy (O-ACT) in reducing sickness absence and was cost-effective over a 24-month period. Here we present 7-years of follow-up on sick leave and the cost of lost production.
Methods
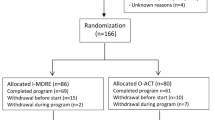
We randomized individuals aged 18–60, sick-listed due to musculoskeletal or mental health disorders to I-MORE (n = 82) or O-ACT (n = 79). I-MORE, lasting 3.5 weeks, integrated ACT, physical training, and work-related problem-solving. In contrast, O-ACT mainly offered six weekly 2.5 h group sessions of ACT. We measured outcomes using registry data for days on medical benefits and calculated costs of lost production. Our analysis included regression analyses to examine differences in sickness absence days, logistic general estimating equations for repeated events, and generalized linear models to assess differences in costs of lost production.
Results
Unadjusted regression analyses showed 80 fewer days of sickness absence in the 7-year follow-up for I-MORE compared to O-ACT (95% CI − 264 to 104), with an adjusted difference of 114 fewer days (95% CI − 298 to 71). The difference in costs of production loss in favour of I-MORE was 27,048 euros per participant (95% CI − 35,009 to 89,104).
Conclusions
I-MORE outperformed O-ACT in reducing sickness absence and production loss costs during seven years of follow-up, but due to a limited sample size the results were unprecise. Considering the potential for substantial societal cost savings from reduced sick leave, there is a need for larger, long-term studies to evaluate return-to-work interventions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sick leave can severely affect an individual’s quality of life, social role, and financial situation [1, 2]. In addition, sick leave has vast impacts on societal productivity [2], and is expected to increase in the future due to demographic changes with an aging population. There has been considerable research on interventions to facilitate return-to-work (RTW), with some reports of positive long-term effects on sick leave and costs [3,4,5]. However, outcomes vary, and there are few studies with long-term follow-up [4, 6].
We have previously reported two-year follow-up data comparing a 3.5-week inpatient multimodal occupational rehabilitation (I-MORE) with a less comprehensive outpatient Acceptance and Commitment Therapy (O-ACT) program for individuals sick-listed due to musculoskeletal or mental health disorders [7,8,9]. We observed fewer days of sickness absence for I-MORE compared to O-ACT [7, 8]. We also found that I-MORE, despite considerably higher interventions costs, was cost-effective compared to O-ACT in a societal perspective due to lower production loss [9]. This paper provides an updated analysis with 7-years follow-up on sick leave and costs of lost production.
Methods
Study Design, Participants, and Interventions
We conducted a randomized controlled trial with parallel groups comparing the effect of I-MORE to O-ACT on sickness absence and production loss over seven years. The primary outcome was sickness absence during 12 months of follow-up, and is reported previously [7].
Eligible participants were 18 to 60 years of age and sick-listed 2 to 12 months with a diagnosis within the musculoskeletal (L), psychological (P) or general and unspecified (A) categories of the ICPC-2 (International Classification of Primary Care, Second edition). I-MORE consisted of physical training, mindfulness, psychoeducation, ACT [10], and work-related problem-solving, conducted both individually and in groups. This program lasted 3.5 weeks, involving 6–7 h daily except on weekends. O-ACT primarily featured group-based ACT-sessions, lasting 2.5 h weekly for six weeks. In addition, there was a group session with psychoeducation on physical activity, two individual sessions with a social worker, and a short individual closing session with a group therapist. Further details about the trial and the interventions have been reported previously [7, 11].
Outcome Measures
Sick leave data were obtained from the Norwegian National Social Security System Registry, where all individuals receiving any form of sickness or disability benefits in Norway are registered by their social security number. To calculate days of sick leave we included the different types of medical benefits: sick leave payments, work assessment allowance and disability pension. Production loss, reflecting the 7-year period, was calculated by multiplying the number of sickness absence days with the average daily wage of 339 euros, as of 2016 data from Statistics Norway [12].
Other Variables
Descriptive variables registered by questionnaires at inclusion were anxiety and depression symptoms, measured using The Hospital Anxiety and Depression scale (HADS) [13], pain assessed by one question from the Brief Pain Inventory (BPI) [14], and educational attainment, categorized as high (college/university) or low. Information about age and sex was obtained from registry data.
Randomization and Blinding
Potential participants were identified in the National Social Security System and randomized after an outpatient screening. An electronic randomization procedure was provided by the Unit of Applied Clinical Research (third-party) at the Norwegian University of Science and Technology (NTNU). Blinding of participants and caregivers was not possible. Sickness absence data were provided by the Norwegian Welfare and Labour Service, who was unaware of group allocation. The researchers were not blinded.
Statistical Analysis
Sample size was calculated based on the primary outcome, i.e., number of sickness absence days during 12 months of follow-up resulting in 80 persons in each arm [11]. In the current study, to account for the actual follow-up durations, i.e., time until retirement, death, or 7 years of follow-up, we standardized sickness absence days for each participant. This was done by first calculating a ratio of number of sickness absence days over possible sickness absence days for seven years for each participant. The ratio was then multiplied by the possible workdays during follow-up (260 days per year). Calculations were based on a 5-day work week and accounted for part-time positions. All three types of medical benefits (sick leave payments, work assessment allowance and disability pension) were used in the calculations. If a participant received a graded disability at inclusion this was not considered sick leave (as it is a permanent benefit), but any subsequent increase in disability benefits were included.
We used regression analyses to estimate the difference in sickness absence days between the groups. The analyses were performed unadjusted and adjusted for age (continuous), sex, education level (high/low) and diagnosis (musculoskeletal/mental health including general and unspecified) for sick leave. The probability of not receiving any medical benefits each month (i.e., working) during follow-up was analyzed as repeating events with logistic general estimating equations. We used an exchangeable correlation structure and robust standard errors. Between group differences in total costs of lost production was tested using generalized linear models with a log link and a gamma distribution. The analyses were performed unadjusted and adjusted (with the beforementioned variables). All analyses were performed in line with the intention-to-treat principle. Precision was assessed using 95% confidence intervals. STATA 17 was used for all analyses (StataCorp. 2021. Stata Statistical Software: Release 17. College Station, TX: StataCorp LP).
Results
In total 166 participants were randomized to I-MORE (n = 86) and O-ACT (n = 80). Five participants (four in I-MORE, one in O-ACT) declined the 7-year follow-up, leaving 161 participants (82 and 79). The baseline characteristics for participants in the two groups were similar (Table 1).
Over the 7-year follow-up, the median total number of sickness absence days were 689 for I-MORE (IQR 254 to 1156) and 770 for O-ACT (IQR 287 to 1422). The mean number of sickness absence days were 761 (SD 570) and 840 (SD 611), respectively. The unadjusted regression analyses showed that I-MORE resulted in 80 fewer sickness absence days (95% CI − 264 to 104) for I-MORE compared to O-ACT. The adjusted analyses showed 114 fewer days (95% CI − 298 to 71) for I-MORE.
Monthly unadjusted estimates showed that I-MORE participants were more likely to be without medical benefits (i.e., working) in the first year, levelling off over time (Fig. 1a). In adjusted analyses this convergence began around the third year (Fig. 1b).
Monthly estimated probability of no medical benefits for inpatient multimodal occupational rehabilitation (I-MORE) versus outpatient acceptance and commitment therapy (O-ACT), based on logistic general estimating equations analyses. a unadjusted; b adjusted for age, sex, education, and main sick leave diagnosis
Over the 7-year period, 79% of the participants in I-MORE and 68% in O-ACT achieved sustainable RTW, i.e., one month without medical benefits. Many participants transitioned between work and different types of benefits during follow-up (Online Supplementary Table S1). At the 7-year mark, 40% were working in the I-MORE group and 29% in the O-ACT group. Full permanent disability benefits were received by 21% in the I-MORE group and 28% in O-ACT. During follow-up, five participants were retired (I-MORE n = 1; O-ACT n = 4) and four died (2 in each group).
Over seven years, the mean costs of lost production for I-MORE were 257,845 euros (SD 193,287) compared to 284,893 euros (SD 207,044) for O-ACT. This difference favoured I-MORE by 27,048 euros per participant (95% CI − 35,009 to 89,104) in unadjusted analyses, and 46,891 euros (95% CI − 19,190 to 112,972) in adjusted analyses. Cumulative costs over the seven years of follow-up are graphically presented in Online Supplementary Figure S1.
Discussion
I-MORE outperformed O-ACT in reducing sickness absence days over seven years with 80–114 days, and consequently incurred lower costs of lost production. However, these results should be interpreted with caution due to the limited sample size.
While few studies have assessed long-term RTW intervention outcomes or incorporated economic evaluations [4, 6], some research aligns with our findings. The impact of I-MORE on sickness absence was most pronounced in the initial years after rehabilitation, consistent with prior research showing the most pronounced effects to occur within three years after rehabilitation [3, 15]. Our participants had on average 200 days of sickness absence at study inclusion which underscores the likely complexity of health issues and challenges with work participation in this study population.
The multicomponent nature of I-MORE precludes identifying which elements contribute to its effectiveness. Key distinctions between the programs include I-MORE`s inpatient format, greater intensity, and multimodal approach. Moreover, although the 3.5-week I-MORE intervention might be perceived as expensive, especially by policymakers who favor less resource demanding programs, it is important to consider the overall value it provides. An attempt to create a condensed, less costly 8-day version of I-MORE, revealed that it did not outperform O-ACT in terms of RTW [16]. In contrast, the 3.5-week I-MORE program, despite its higher cost, was cost-effective in a societal perspective compared to O-ACT [9]. A challenge when implementing RTW programs in Norway is that the costs fall on the healthcare system while the savings (reduced sick leave) benefit another sector. The results of this study, and previous publications from this project, highlights the need for policymakers to adopt a societal perspective when planning interventions for sick-listed workers to consider broader economic benefits. This also aligns with recommendations by an expert group on priority setting in Norway [17].
The vast societal impact of sick leave means that even moderate effects of interventions may reduce societal costs substantially. Therefore, the low precision in our effect estimates emphasize the need for larger studies, which could also identify subgroups best suited for comprehensive programs or alternative interventions.
The main strength of this study was the use of long-term registry data for sickness absence, eliminating missing data and recall bias. The main limitation was the limited sample size.
In summary, while I-MORE outperformed O-ACT in reducing sickness absence days and also costs of lost production, the low precision of the estimates, due to a small sample size, remains a concern. Given the societal implications of extended sick leave, future larger-scale RTW intervention studies with long-term follow-up are encouraged for more accurate effect estimations.
Data Availability
Data are not available due to ethical approval.
References
Waddell G, Burton AK. Is work good for your health and well-being? Norwich: TSO; 2006.
Bevan S. Economic impact of musculoskeletal disorders (MSDs) on work in Europe. Best Pract Res Clin Rheumatol. 2015;29(3):356–73. https://doi.org/10.1016/j.berh.2015.08.002.
Busch H, Bodin L, Bergström G, Jensen IB. Patterns of sickness absence a decade after pain-related multidisciplinary rehabilitation. Pain. 2011;152(8):1727–33. https://doi.org/10.1016/j.pain.2011.02.004.
Cullen KL, Irvin E, Collie A, Clay F, Gensby U, Jennings PA, et al. Effectiveness of workplace interventions in return-to-work for musculoskeletal, pain-related and mental health conditions: an update of the evidence and messages for practitioners. J Occup Rehabil. 2018;28(1):1–15. https://doi.org/10.1007/s10926-016-9690-x.
Loisel P, Lemaire J, Poitras S, Durand MJ, Champagne F, Stock S, et al. Cost-benefit and cost-effectiveness analysis of a disability prevention model for back pain management: a six year follow up study. Occup Environ Med. 2002;59(12):807–15.
Vogel N, Schandelmaier S, Zumbrunn T, Ebrahim S, de Boer WE, Busse JW, et al. Return-to-work coordination programmes for improving return to work in workers on sick leave. Cochrane Database Syst Rev. 2017;3(3):Cd011618. https://doi.org/10.1002/14651858.CD011618.pub2.
Gismervik SO, Aasdahl L, Vasseljen O, Fors EA, Rise MB, Johnsen R, et al. Inpatient multimodal occupational rehabilitation reduces sickness absence among individuals with musculoskeletal and common mental health disorders: a randomized clinical trial. Scand J Work Environ Health. 2020. https://doi.org/10.5271/sjweh.3882.
Aasdahl L, Vasseljen O, Gismervik S, Johnsen R, Fimland MS. Two-year follow-up of a randomized clinical trial of inpatient multimodal occupational rehabilitation vs outpatient acceptance and commitment therapy for sick listed workers with musculoskeletal or common mental disorders. J Occup Rehabil. 2021. https://doi.org/10.1007/s10926-021-09969-4.
Aasdahl L, Fimland MS, Bjørnelv GMW, Gismervik S, Johnsen R, Vasseljen O, et al. Economic evaluation of inpatient multimodal occupational rehabilitation vs. outpatient acceptance and commitment therapy for sick-listed workers with musculoskeletal- or common mental disorders. J Occup Rehabil. 2023. https://doi.org/10.1007/s10926-022-10085-0.
Hayes SCSK, Wilson KG. Acceptance and commitment therapy: an experiential approach to behavior change. New York: The Guilford Press; 2003.
Fimland MS, Vasseljen O, Gismervik S, Rise MB, Halsteinli V, Jacobsen HB, et al. Occupational rehabilitation programs for musculoskeletal pain and common mental health disorders: study protocol of a randomized controlled trial. BMC Public Health. 2014;14(1):368. https://doi.org/10.1186/1471-2458-14-368.
Statistics Norway: wages—occupational monthly salary, by sector, sex and working hours 2015–2021. https://www.ssb.no/statbank/table/11418/. Accessed 5 Apr 2022.
Zigmond AS, Snaith RP. The Hospital Anxiety and Depression Scale. Acta Psychiatr Scand. 1983;67(6):361–70.
Cleeland CS, Ryan KM. Pain assessment: global use of the Brief Pain Inventory. Ann Acad Med Singapore. 1994;23(2):129–38.
Suoyrjö H, Hinkka K, Oksanen T, Kivimäki M, Klaukka T, Pentti J, et al. Effects of multidisciplinary inpatient rehabilitation for chronic back or neck pain: a register-linkage study of sickness absences and analgesic purchases in an occupational cohort. Occup Environ Med. 2008;65(3):179–84. https://doi.org/10.1136/oem.2007.033753.
Aasdahl L, Pape K, Vasseljen O, Johnsen R, Gismervik S, Halsteinli V, et al. Effect of inpatient multicomponent occupational rehabilitation versus less comprehensive outpatient rehabilitation on sickness absence in persons with musculoskeletal- or mental health disorders: a randomized clinical trial. J Occup Rehabil. 2017. https://doi.org/10.1007/s10926-017-9708-z.
Helse-og omsorgsdepartementet. Perspectives and priorities—a report from the expert group set by the Ministry of Health and Care services on perspectives in priorities [In Norwegian]. 2024.
Acknowledgements
We thank clinicians and staff at Hysnes Rehabilitation Centre and the Clinic of Rehabilitation at St. Olavs Hospital, and all study participants.
Funding
Open access funding provided by NTNU Norwegian University of Science and Technology (incl St. Olavs Hospital - Trondheim University Hospital). The Liaison Committee between the Central Norway Regional Health Authority and the Norwegian University of Science and Technology; The Research Council of Norway (Grant Nos. 238015 and 295989); and government funding via the Central Norway Regional Health Authority.
Author information
Authors and Affiliations
Contributions
MSF, RJ, OV, SG and LA developed the project. MSF and RJ led the project. SG developed and led the O-ACT comparison intervention. LA led the analyses, assisted by GMWB and JH, and wrote the initial draft. All authors critically reviewed, refined, and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
MSF previously worked at Hysnes Rehabilitation Center, St. Olavs Hospital. MSF and LA were previously affiliated with, and SØG is currently employed, at the Department of Physical Medicine and Rehabilitation, St. Olavs Hospital. Other authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. All participants provided informed written consent. The study was approved by the Regional Committee for Medical and Health Research Ethics in Central Norway (No: 2012/1241) and included approval for linkage to registry data and seven years of follow-up. The study is registered in clinicaltrials.gov (No: NCT01926574).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Aasdahl, L., Gismervik, S.Ø., Johnsen, R. et al. Effects of Inpatient Occupational Rehabilitation vs. Outpatient Acceptance and Commitment Therapy on Sick Leave and Cost of Lost Production: 7-Year Follow-Up of a Randomized Controlled Trial. J Occup Rehabil (2024). https://doi.org/10.1007/s10926-024-10195-x
Accepted:
Published:
DOI: https://doi.org/10.1007/s10926-024-10195-x