Abstract
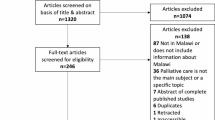
The paper aims to identify and describe the European evidence on opportunities and barriers to access and utilization of palliative care among non- western migrants. A systematic review in accordance with PRISMA guidelines was conducted in June 2020, searching Medline, CINAHL, PsychINFO and EMBASE databases. PROSPERO# CRD42020193651. Studies included empirical research published between 2011 and 2020. Search words were, for example, ethnic groups and palliative care. Thematic analysis was used to analyze data. Twenty nine qualitative and six quantitative studies were included. Four main themes were identified: communication and language; knowledge and awareness; patient preferences, cultural and religious issues; and lack of resources at different levels of palliative care service provision. Migrants’ access to palliative care is impeded at system, community and individual levels, yet, recommendations are mostly at the individual level. Closer attention is required to these different levels when designing future palliative interventions for migrants.

Similar content being viewed by others
References
McAuliffe M, Khadria B, Céline Bauloz MN. World migration report 2020. Geneva: International Organisation for Migration; 2020.
Migration in Europe—Statistics and Facts: Statista Research Department; [updated 05.03.2020. https://www.statista.com/topics/4046/migration-in-europe/.
Migration and migrant population statistics: Eurostat; [updated 15.07. 2020]. https://ec.europa.eu/eurostat/statistics-explained/index.php/Migration_and_migrant_population_statistics.
How health systems can address health inequities linked to migration and ethnicity. 2010.
Palliative care: World Health Organization. https://www.euro.who.int/en/health-topics/noncommunicable-diseases/cancer/policy/palliative-care.
Expert Panel on effective ways of investing in Health (EXPH), Report on Access to Health Services in the European Union. 3 May 2016.
Davies E, Higginson IJ. Better palliative care for older people. Copenhagen: World Health Organization (WHO) Regional Office for Europe; 2004.
Mladovsky P. Migration and health in the EU. Research Note produced for the European Commission as part of the Health and Living Conditions Network of the European Observatory on the Social Situation and Demography. 2007.
Cuadra CB. Right of access to health care for undocumented migrants in EU: a comparative study of national policies. Eur J Public Health. 2012;22(2):267–71.
Jansky M, Owusu-Boakye S, Nauck F. An odyssey without receiving proper care": experts’ views on palliative care provision for patients with migration background in Germany. BMC Palliat Care. 2019;18(1):1–10.
What are the 7 continents of the world?: world population review. https://worldpopulationreview.com/continents/7-continents-of-the-world.
Pavli A, Maltezou H. Health problems of newly arrived migrants and refugees in Europe. J Travel Med. 2017. https://doi.org/10.1093/jtm/tax016.
Ikram UZ, Kunst AE, Lamkaddem M, Stronks K. The disease burden across different ethnic groups in Amsterdam, the Netherlands, 2011–2030. Eur J Public Health. 2014;24(4):600–5.
Calanzani N, Koffman J, Higginson I. Palliative and end of life care for Black, Asian and Minority Ethnic Groups in the UK: demographic profile and the current state of palliative and end of life care provision. London: Public Health England, King’s College London and Marie Curie Cancer Care; 2013.
Nair M, Prabhakaran D. Why do South Asians have high risk for CAD? Glob Heart. 2012;7(4):307–14.
Worth A, Irshad T, Bhopal R, Brown D, Lawton J, Grant E, et al. Vulnerability and access to care for South Asian Sikh and Muslim patients with life limiting illness in Scotland: prospective longitudinal qualitative study. BMJ. 2009;338:b183.
Evans N, Meñaca A, Andrew EV, Koffman J, Harding R, Higginson IJ, et al. Appraisal of literature reviews on end-of-life care for minority ethnic groups in the UK and a critical comparison with policy recommendations from the UK end-of-life care strategy. BMC Health Serv Res. 2011;11(1):1–11.
Calanzani N, Moens K, Cohen J, Higginson IJ, Harding R, Deliens L, et al. Choosing care homes as the least preferred place to die: a cross-national survey of public preferences in seven European countries. BMC Palliat Care. 2014;13:48.
Evans N, Menaca A, Andrew EV, Koffman J, Harding R, Higginson IJ, et al. Systematic review of the primary research on minority ethnic groups and end-of-life care from the United Kingdom. J Pain Symptom Manage. 2012;43(2):261–86.
Smith AK, Earle CC, McCarthy EP. Racial and ethnic differences in end-of-life care in fee-for-service Medicare beneficiaries with advanced cancer. J Am Geriatr Soc. 2009;57(1):153–8.
Speck P. Culture and spirituality: essential components of palliative care. Postgrad Med J. 2016;92(1088):341–5.
De Souza J, Gillett K, Froggatt K, Walshe C. Perspectives of elders and their adult children of Black and minority ethnic heritage on end-of-life conversations: a meta-ethnography. Palliat Med. 2020;34(2):195–208.
De Graaff FM, Mistiaen P, Deville WL, Francke AL. Perspectives on care and communication involving incurably ill Turkish and Moroccan patients, relatives and professionals: a systematic literature review. BMC Palliat Care. 2012;11:1–37.
Torres S, Ågård P, Milberg A. The ‘other’in end-of-life care: providers’ understandings of patients with migrant backgrounds. J Intercult Stud. 2016;37(2):103–17.
Milberg A, Torres S, Agard P. Health care professionals’ understandings of cross-cultural interaction in end-of-life care: a focus group study. PLoS ONE. 2016;11(11):e0165452.
Schrank B, Rumpold T, Amering M, Masel EK, Watzke H, Schur S. Pushing boundaries-culture-sensitive care in oncology and palliative care: a qualitative study. Psychooncology. 2017;26(6):763–9.
Hawker S, Payne S, Kerr C, Hardey M, Powell J. Appraising the evidence: reviewing disparate data systematically. Qual Health Res. 2002;12(9):1284–99.
Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101.
Venkatasalu MR. Let him not be alone: perspectives of older British South Asian minority ethnic patients on dying in acute hospitals. Int J Palliat Nurs. 2017;23(9):432–9.
Venkatasalu MR, Arthur A, Seymour J. Talking about end-of-life care: the perspectives of older South Asians living in East London. J Res Nurs. 2013;18(5):394–406.
Venkatasalu MR, Seymour JE, Arthur A. Dying at home: a qualitative study of the perspectives of older South Asians living in the United Kingdom. Palliat Med. 2014;28(3):264–72.
de Graaff FM, Francke AL, van den Muijsenbergh ME, van der Geest S. Understanding and improving communication and decision-making in palliative care for Turkish and Moroccan immigrants: a multiperspective study. Ethn Health. 2012;17(4):363–84.
Graaff FM, Francke AL, Muijsenbergh METC, Geest S. Talking in triads: communication with Turkish and Moroccan immigrants in the palliative phase of cancer. J Clin Nurs. 2012;21(21–22):3143–52.
Wilkinson E, Randhawa G, Brown E, Da Silva GM, Stoves J, Warwick G, et al. Exploring access to end of life care for ethnic minorities with end stage kidney disease through recruitment in action research. BMC Palliat Care. 2016;15:1–9.
Wilkinson E, Randhawa G, Brown E, Da Silva GM, Stoves J, Warwick G, et al. Time, timing, talking and training: findings from an exploratory action research study to improve quality of end of life care for minority ethnic kidney patients. Clin Kidney J. 2017;10(3):419–24.
Wilkinson E, Randhawa G, Brown EA, Da Silva GM, Stoves J, Warwick G, et al. Communication as care at end of life: an emerging issue from an exploratory action research study of renal end-of-life care for ethnic minorities in the UK. J Ren Care. 2014;40(Suppl 1):23–9.
Wilkinson E, Waqar M, Gill B, Hoque P, Jetha C, Bola KK, et al. Exploring end-of-life care for South Asian kidney patients: interviewer reflections. Int J Palliat Nurs. 2017;23(3):120–8.
Van Keer R-L, Deschepper R, Francke AL, Huyghens L, Bilsen J. Conflicts between healthcare professionals and families of a multi-ethnic patient population during critical care: an ethnographic study. Crit Care. 2015;17:1–13.
Van Keer R-L, Deschepper R, Huyghens L, Bilsen J. Challenges in delivering bad news in a multi-ethnic intensive care unit: an ethnographic study. Patient Educ Couns. 2019;102(12):2199–207.
Van Keer RL, Deschepper R, Huyghens L, Bilsen J. Mental well-being of patients from ethnic minority groups during critical care: a qualitative ethnographic study. BMJ Open. 2017;7(9):e014075.
Gunaratnam Y. Cultural vulnerability: a narrative approach to intercultural care. Qual Soc Work. 2013;12(2):104–18.
Kai J, Beavan J, Faull C. Challenges of mediated communication, disclosure and patient autonomy in cross-cultural cancer care. Br J Cancer. 2011;105(7):918–24.
Henke A, Thuss-Patience P, Behzadi A, Henke O. End-of-life care for immigrants in Germany. An epidemiological appraisal of Berlin. PLoS ONE. 2017;12(8):e0182033.
Finnvold JE. How social and geographical backgrounds affect hospital admission with a serious condition: a comparison of 11 immigrant groups with native-born Norwegians. BMC Health Serv Res. 2018;18(1):1–11.
Fang ML, Malcoe LH, Sixsmith J, Wong LY, Callender M. Exploring traditional end-of-life beliefs, values, expectations, and practices among Chinese women living in England: informing culturally safe care. Palliat Support Care. 2015;13(5):1261–74.
Debesay J, Harslof I, Rechel B, Vike H. Facing diversity under institutional constraints: challenging situations for community nurses when providing care to ethnic minority patients. J Adv Nurs. 2014;70(9):2107–16.
Islam Z, Markham S, Faull C. Raising the profile of palliative care services for BAME groups within Leicester city: challenges with recruiting and training volunteers. Divers Equal Health Care. 2015;12(3):116–23.
Raunkiar M. Conceptions about the death of elderly with ethnic minority background in own homes and in nursing homes. Klin Sygepleje. 2012;26(3):61–73.
Markham S, Islam Z, Faull C. (2014) I never knew that! Why do people from Black and Asian Minority Ethnic groups in Leicester access hospice services less than other groups? A discussion with community groups. Divers Equal Health Care. 2014;11:23–745.
Cowan MM. The lived experiences of the Sikh population of south east England when caring for a dying relative at home. Int J Palliat Nurs. 2014;20(4):179–86.
Paal P, Bükki J. “If I had stayed back home, I would not be alive any more…”: exploring end-of-life preferences in patients with migration background. PLoS ONE. 2017;12(4):e0175314.
Samanta J, Samanta A, Madhloom O. A rights-based proposal for managing faith-based values and expectations of migrants at end-of-life illustrated by an empirical study involving South Asians in the UK. Bioethics. 2018;32(6):368–77.
Coupland VH, Madden P, Jack RH, Moller H, Davies EA. Does place of death from cancer vary between ethnic groups in South East England? Palliat Med. 2011;25(4):314–22.
Koffman J, Ho YK, Davies J, Gao W, Higginson IJ. Does ethnicity affect where people with cancer die? A population-based 10 year study. PLoS ONE. 2014;9(4):e95052.
Torensma M, Suurmond JL, van der Heide A, Onwuteaka-Philipsen BD. Care and decision-making at the end of life for patients with a non-western migration background living in the Netherlands: a nationwide mortality follow-back study. J Pain Symptom Manage. 2020;59(5):990-1000.e5.
Sharpe KH, Cezard G, Bansal N, Bhopal RS, Brewster DH. Policy for home or hospice as the preferred place of death from cancer: Scottish Health and Ethnicity Linkage Study population cohort shows challenges across all ethnic groups in Scotland. BMJ Support Palliat Care. 2015;5(4):443–51.
Kristiansen M, Irshad T, Worth A, Bhopal R, Lawton J, Sheikh A. The practice of hope: a longitudinal, multi-perspective qualitative study among South Asian Sikhs and Muslims with life-limiting illness in Scotland. Ethn Health. 2014;19(1):1–19.
Torensma M, Onwuteaka-Philipsen BD, Strackee KL, Oosterveld-Vlug MG, de Voogd X, Willems DL, et al. How to help researchers in palliative care improve responsiveness to migrants and other underrepresented populations: developing and testing a self-assessment instrument. BMC Palliat Care. 2019;18(1):1–11.
Samanta J, Samanta A. Exploring cultural values that underpin the ethical and legal framework of end-of-life care: a focus group study of South Asians. J Med Law Ethics. 2013;1(1):63–74.
Shabnam J, Timm H, Nielsen DS, Raunkiaer M. Palliative care for older South Asian migrants: a systematic review. Palliat Support Care. 2020;18(3):346–58.
Fang ML, Sixsmith J, Sinclair S, Horst G. A knowledge synthesis of culturally- and spiritually-sensitive end-of-life care: findings from a scoping review. BMC Geriatr. 2016;16:107.
Rechel B, Mladovsky P, Ingleby D, Mackenbach JP, McKee M. Migration and health in an increasingly diverse Europe. The Lancet. 2013;381(9873):1235–45.
Lolle H, Torpe L. Growing ethnic diversity and social trust in European societies. Comp Eur Polit. 2011;9(2):191–216.
Rahemi Z, Williams CL. Does ethnicity matter—cultural factors underlying older adults’ end-of-life care preferences: a systematic review. Geriatr Nurs. 2020;41(2):89–97.
Hiam L, Gionakis N, Holmes S, McKee M. Overcoming the barriers migrants face in accessing health care. Public Health. 2019;172:89–92.
Cain C, Cain CL, Surbone A, Elk R, Kagawa-Singer M. Culture and palliative care: preferences, communication, meaning, and mutual decision making. J Pain Symptom Manage. 2018;55(5):1408–19.
Harding R, Simms V, Calanzani N, Higginson I, Hall S, Gysels M, et al. If you had less than a year to live, would you want to know? A seven-country European population survey of public preferences for disclosure of poor prognosis. Psychooncology. 2013;22(10):2298–305.
Clark D, Baur N, Clelland D, Garralda E, López-Fidalgo J, Connor S, et al. Mapping levels of palliative care development in 198 countries: the situation in 2017. J Pain Symptom Manag. 2020;59(4):794–807.
Radbruch L, Payne S. White paper on standards and norms for hospice and palliative care in Europe: part 1. Eur J Palliat Care. 2009;16(6):278–89.
Sørensen K, Van den Broucke S, Fullam J, Doyle G, Pelikan J, Slonska Z, et al. Health literacy and public health: a systematic review and integration of definitions and models. BMC Public Health. 2012;12(1):80.
Murtagh FE, Bausewein C, Verne J, Groeneveld EI, Kaloki YE, Higginson IJ. How many people need palliative care? A study developing and comparing methods for population-based estimates. Palliat Med. 2014;28(1):49–58.
Organization WH. Planning and implementing palliative care services: a guide for programme managers. Report No. 9241565411. Geneva: WHO; 2016.
Booth A, Moore G, Flemming K, Garside R, Rollins N, Tunçalp Ö, et al. Taking account of context in systematic reviews and guidelines considering a complexity perspective. BMJ Glob Health. 2019;4(Suppl 1):e000840.
Matlin SA, Depoux A, Schütte S, Flahault A, Saso L. Migrants’ and refugees’ health: towards an agenda of solutions. Public Health Rev. 2018;39:1–55.
Cain CL, Surbone A, Elk R, Kagawa-Singer M. Culture and palliative care: preferences, communication, meaning, and mutual decision making. J Pain Symptom Manag. 2018;55(5):1408–19.
Kelley AS, Morrison RS. Palliative care for the seriously ill. N Engl J Med. 2015;373(8):747–55.
Statistik D. Indvandrere og efterkommere. Lokaliseret. 2019;18:2019.
Speck P, Ellershaw J, Wilkinson S. Spiritual/religious issues in care of the dying. Care of Dying A pathway to excellence. 2011. p. 106–26.
Acknowledgements
The authors would like to thank Librarian, Anne Faber Hansen for her contribution in the search strategy and Professor David Clark for his help in the English revision of the manuscript.
Funding
The first author received financial support for her PhD study from The Danish Cancer Society, case number—R210-A12932-18-S64. This work is a part of her PhD.
Author information
Authors and Affiliations
Contributions
JS and MR conceptualize and designed the study. JS was responsible for data collection, extraction, analysis and writing initial draft of the manuscript. MR supervised and guided throughout the entire process. HT and DN reviewed and edited the paper in the writing process. All authors approved the final paper.
Corresponding author
Ethics declarations
Conflict of interests
The authors declare that they have no conflict of interests.
Ethical Approval
Approval for this research was obtained from The Danish National Committee on Bioethics, number 61269.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Shabnam, J., Timm, H.U., Nielsen, D.S. et al. Palliative Care Utilization Among Non-Western Migrants in Europe: A Systematic Review. J Immigrant Minority Health 24, 237–255 (2022). https://doi.org/10.1007/s10903-021-01302-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10903-021-01302-8