Abstract
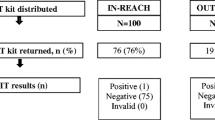
Latinas’ high colorectal cancer (CRC) mortality makes them a priority population for CRC screening. CRC screening knowledge, perceived barriers, and feasibility of using the Fecal Immunochemical Test (FIT) was assessed among Latinas in Utah. Participants aged ≥50 (n = 95) were surveyed about knowledge and barriers to CRC screening. 27 participants completed a FIT and evaluation survey. Fisher’s exact tests assessed sociodemographic correlates of CRC screening outcomes. Most participants were overdue for CRC screening (n = 81, 85%). Age, acculturation, education, and employment were significantly associated with CRC screening status and/or reasons for being overdue (e.g., not knowing about the test, cost). All participants who received a FIT completed it, felt it was easy to use, and reported they would use it again. Latinas had limited awareness of CRC, CRC screenings, and experienced barriers to CRC screening (e.g., limited access, cost), but were willing to utilize a low-cost home-based FIT.

Similar content being viewed by others
References
Escarce J, Morales L, Rumbaut R. The health status and health behaviors of hispanics. In: Tienda M, Mitchell F, editors. National Research Council (US) Panel on Hispanics in the United States. Washington (DC): National Academies of Press; 2006.
Cancer Facts & Figures for Hispanics/Latinos 2012–2014. Atlanta, GA: American Cancer Society; 2012.
Healthy People 2020 Topics & Objectives: Cancer. 2012; https://www.healthypeople.gov/2020/topics-objectives/topic/cancer/objectives. Accessed 04/05/2017.
Colby S, Ortman J. Projections of the size and composition of the U.S. population: 2014–2060. Washington, DC: U.S. Census Bureau; 2014.
QuickFacts United States 2015; https://www.census.gov/quickfacts/table/PST045216/00. Accessed 04 Jun 2017.
Salt Lake City, Utah QuickFacts 2010. Available from: http://www.census.gov/quickfacts/table/PST045215/4967000.
Hispanic Demographics: Utah Hispanice Chamber of COmmerce; 2016. Available from: http://www.utahhcc.com/hispanic-res/demographics.
Brown A. U.S. Hispanic and Asian populations growing, but for different reasons. PewResearchCenter; 2014. Available from: http://www.pewresearch.org/fact-tank/2014/06/26/u-s-hispanic-and-asian-populations-growing-but-for-different-reasons/.
L D. Census: Utah’s Latino population grows to more than 400,000. 2016; http://archive.sltrib.com/story.php?ref=/home/4035282-155. Accessed 04 May 2017.
Public Health Indicator Based Information System (IBIS): Complete Health Indicator Report of Birth Rates. 2017; https://ibis.health.utah.gov/indicator/complete_profile/BrthRat.html. Accessed 05 Oct 2017.
Hamilton BE, Martin JA, Osterman MJK, Curtin SC, Mathews TJ. Births: final Data for 2014. Nat Vital Stat Rep. 2015;64(12):1–72.
Stepler R, Brown A. Statistical portrait of Hispanics in the United States: Pew Research Center Hispanic Trends; 2016. Available from: http://www.pewhispanic.org/2016/04/19/statistical-portrait-of-hispanics-in-the-united-states-key-charts/#hispanic-pop.
Office of Health Disparities: Hispanic & Latino Health: Utah: Department of Health; 2016. Available from: http://www.health.utah.gov/disparities/utah-minority-communities/hispanic-latino.html.
Shih YC, Elting LS, Levin B. Disparities in colorectal screening between US-born and foreign-born populations: evidence from the 2000 National Health Interview Survey. J Cancer Edu. 2008;23(1):18–25.
Health Indicator Report of Colorectal Cancer Deaths 2015. Available from: http://ibis.health.utah.gov/indicator/view/ColCADth.Eth.html.
Health Indicator Report of Colorectal Cancer Screening 2015. Available from: http://ibis.health.utah.gov/indicator/view/ColCAScr.UT_US.html.
Jones RM, Devers KJ, Kuzel AJ, Woolf SH. Patient-reported barriers to colorectal cancer screening: a mixed-methods analysis. Am J Prev Med. 2010;38(5):508–16.
van Ballegooijen M, Habbema JDF, Boer R, Zauber AG, Brown ML. AHRQ technology assessments. A comparison of the cost-effectiveness of fecal occult blood tests with different test characteristics in the context of annual screening in the medicare population. Rockville (MD): Agency for Healthcare Research and Quality; 2003.
Smith RA, Andrews K, Brooks D, et al. Cancer screening in the United States, 2016: a review of current American Cancer Society guidelines and current issues in cancer screening. CA Cancer J Clin. 2016;66(2):96–114.
Short MW, Layton MC, Teer BN, Domagalski JE. Colorectal cancer screening and surveillance. Am Fam Physician. 2015;91(2):93–100.
Natale-Pereira A, Marks J, Vega M, Mouzon D, Hudson SV, Salas-Lopez D. Barriers and facilitators for colorectal cancer screening practices in the Latino community: perspectives from community leaders. Cancer Control. 2008;15(2):157–65.
Walsh JME, Salazar R, Kaplan C, Nguyen L, Hwang J, Pasick RJ. Healthy colon, healthy life (Colon Sano, Vida Sana): colorectal cancer screening among Latinos in Santa Clara, California. J Cancer Educ. 2010;25(1):36–42.
Hillyer GC, Schmitt KM, Freedberg DE, et al. Fecal-based colorectal cancer screening among the Uninsured in Northern Manhattan. Am J Prev Med. 2014;47(2):182–7.
Fowler B, Bodson J, Warner EL, Dyer J, Kepka D. Poor HPV vaccine-related awareness and knowledge among Utah Latinas overdue for recommended cancer screenings. J Community Health. 2016.
Prevention Care Management: National Cancer Institute; 2010. Available from: http://rtips.cancer.gov/rtips/programDetails.do?programId=295722.
Dietrich AJ, Tobin JN, Cassells A, Robinson CM, Greene MA, Sox CH, et al. Telephone care management to improve cancer screening among low-income women: a randomized, controlled trial. Ann Intern Med. 2006;144(8):563–71.
Rapid response TM fecal immunochemical test (FIT) Cassette. 2014; http://www.btnx.com/Product.aspx?id=1735. Accessed 04 May 2017.
American Cancer Society recommendations for colorectal cancer early detection 2016. Available from: http://www.cancer.org/cancer/colonandrectumcancer/moreinformation/colonandrectumcancerearlydetection/colorectal-cancer-early-detection-acs-recommendations.
Colorectal cancer: screening 2008. Available from: http://www.uspreventiveservicestaskforce.org/Page/Document/UpdateSummaryFinal/colorectal-cancer-screening.
Coronado GD, Farias A, Thompson B, Godina R, Oderkirk W. Attitudes and beliefs about colorectal cancer among Mexican Americans in communities along the US-Mexico border. Ethn Dis. 2006;16(2):421–7.
Fernandez ME, Wippold R, Torres-Vigil I, Byrd T, Freeberg D, Bains Y, et al. Colorectal cancer screening among Latinos from U.S. cities along the Texas-Mexico border. Cancer Causes Control. 2008;19(2):195–206.
Gerstel N. Rethinking families and community: the color, class, and centrality of extended kin ties. Sociol Forum. 2011;26(1):1–20.
Sarkisian N, Gerena M, Gerstel N. Extended family ties among Mexicans, Puerto Ricans, and Whites: superintegration or disintegration? Family Relations. 2006;55(3):331–44.
Flowers L, Noel-Miller C, Okrent D. Colonoscopy Screening after the Affordable Care Act: Cost Barriers Persist for Medicare Beneficiaries. 2013.
Mach AL. Individual Mandate Under the ACA. Congressional Research Service, 2015.
Colorectal cancer screening: Insurance coverage: American Cancer Society, 2016. Available from: http://www.cancer.org/cancer/colonandrectumcancer/moreinformation/colonandrectumcancerearlydetection/colorectal-cancer-early-detection-screening-coverage-laws.
Sheinfeld Gorin S, Heck JE. Cancer screening among Latino subgroups in the United States. Prev Med. 2005;40(5):515–26.
van Jaarsveld CH, Miles A, Edwards R, Wardle J. Marriage and cancer prevention: does marital status and inviting both spouses together influence colorectal cancer screening participation? J Med Screen. 2006;13(4):172–6.
Braschi CD, Sly JR, Singh S, Villagra C, Jandorf L. Increasing colonoscopy screening for Latino Americans through a patient navigation model: a randomized clinical trial. J Immigr Health. 2014;16(5):934–40.
Flórez KR, Aguirre AN, Viladrich A, Céspedes A, De La Cruz AA, Abraído-Lanza AF. Fatalism or Destiny? A qualitative study and interpretative framework on dominican women’s breast cancer beliefs. J Immigr Health. 2009;11(4):291–301.
Powe BD. Fatalism among elderly African Americans. Effects on colorectal cancer screening. Cancer Nurs. 1995;18(5):385–92.
Chavez LR, Hubbell FA, Mishra SI, Valdez RB. The influence of fatalism on self-reported use of Papanicolaou smears. Am J Prev Med. 1997;13(6):418–24.
Moralez EA, Rao SP, Livaudais JC, Thompson B. Improving knowledge and screening for colorectal cancer among Hispanics: overcoming barriers through a PROMOTORA-led home-based educational intervention. J Cancer Edu. 2012;27(3):533–9.
Janz NK, Becker MH. The health belief model: a decade later. Health Edu Q. 1984;11(1):1–47.
Rao SK, Schilling TF, Sequist TD. Challenges in the management of positive fecal occult blood tests. J Gen Intern Med. 2009;24(3):356–60.
Yabroff KR, Klabunde CN, Myers R, Brown ML. Physician recommendations for follow-up of positive fecal occult blood tests. Med Care Res Rev. 2005;62(1):79–110.
Marin G, Sabogal F, Vanoss-Marin B, Otero-Sabogal R, Perez-Stable E. Development of a short acculturation scale for hispanics. Hisp J Behav Sci. 1987;9(2):183–205.
Kepka D, Warner EL, Kinney AY, Spigarelli MG, Mooney K. Low human papillomavirus (HPV) vaccine knowledge among Latino parents in Utah. J Immigr Minor Health. 2015;17(1):125–31.
Acknowledgements
We would like to acknowledge and thank the participants for their time and important contributions to this study. We would also like to thank the community organizations, Alliance Community Services and Comunidades Unidas, for their assistance with recruiting participants. Ms. Warner is thankful to be supported by the Jonas Center for Nursing and Veterans Healthcare.
Funding
This study was funded by the Utah Department of Health, the Beaumont Foundation, the University of Utah College of Nursing Research Committee, and the Huntsman Cancer Foundation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare they have no potential conflicts of interest to disclose.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Warner, E.L., Bodson, J., Mooney, R. et al. Latinas’ Colorectal Cancer Screening Knowledge, Barriers to Receipt, and Feasibility of Home-Based Fecal Immunochemical Testing. J Immigrant Minority Health 20, 981–990 (2018). https://doi.org/10.1007/s10903-017-0615-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10903-017-0615-3