Abstract
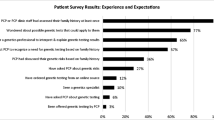
Even at the end of life, testing cancer patients for inherited susceptibility may provide life-saving information to their relatives. Prior research suggests palliative care inpatients have suboptimal understanding of genetic importance, and testing may be underutilized in this clinical setting. These conclusions are based on limited research. This study aimed to estimate genetic testing prevalence among high-risk palliative care patients in a National Cancer Institute-designated comprehensive cancer center. We also aimed to understand these patients’ understanding of, and attitudes toward, hereditary cancer testing and DNA banking. Palliative care in-patients with cancer completed structured interviews, and their medical records were reviewed. Among patients at high risk for hereditary cancer, we assessed history of genetic testing/DNA banking; and related knowledge and attitudes. Among 24 high-risk patients, 14 (58.3%) said they/their relatives had genetic testing or they had been referred for a genetics consultation. Of the remaining 10 patients, seven (70%) said they would “probably” or “definitely” get tested. Patients who had not had testing were least concerned about the impact of future testing on their family relationships; two (20%) said they were “extremely concerned” about privacy related to genetic testing. Of patients without prior testing, five (50%) said they had heard or read “a fair amount” about genetic testing. No high-risk patients had banked DNA. Overall, 23 (95.8%) said they had heard or read “almost nothing” or “relatively little” about DNA banking. Written materials and clinician discussion were most preferred ways to learn about genetic testing and DNA banking. Overall, this study demonstrates underutilization of genetics services at the end of life continues to be problematic, despite high patient interest.

Similar content being viewed by others
References
Berg, A. O., Baird, M. A., Botkin, J. R., Driscoll, D. A., Fishman, P. A., Guarino, P. D., et al. (2009). National institutes of health state-of-the-science conference statement: Family history and improving health. Annals of Internal Medicine, 151(12), 872–877.
Borzekowski, D. L., Guan, Y., Smith, K. C., Erby, L. H., & Roter, D. L. (2014). The Angelina effect: Immediate reach, grasp, and impact of going public. Genetics in Medicine: Official Journal of the American College of Medical Genetics, 16(7), 516–521.
Cohen, P. A., Nichols, C. B., Schofield, L., Van Der Werf, S., & Pachter, N. (2016). Impact of clinical genetics attendance at a gynecologic oncology tumor board on referrals for genetic counseling and BRCA mutation testing. International Journal of Gynecological Cancer: Official Journal of the International Gynecological Cancer Society, 26(5), 892–897.
Delikurt, T., Williamson, G. R., Anastasiadou, V., & Skirton, H. (2015). A systematic review of factors that act as barriers to patient referral to genetic services. European Journal of Human Genetics: EJHG, 23(6), 739–745.
Durfy, S. J., Bowen, D. J., McTiernan, A., Sporleder, J., & Burke, W. (1999). Attitudes and interest in genetic testing for breast and ovarian cancer susceptibility in diverse groups of women in western Washington. Cancer Epidemiology, Biomarkers & Prevention: A Publication of the American Association for Cancer Research, Co-sponsored by the American Society of Preventive Oncology, 8(4 Pt 2), 369–375.
Eichmeyer, J. N., Burnham, C., Sproat, P., Tivis, R., & Beck, T. M. (2014). The value of a genetic counselor: Improving identification of cancer genetic counseling patients with chart review. Journal of Genetic Counseling, 23(3), 323–329.
Evans, D. G., Barwell, J., Eccles, D. M., Collins, A., Izatt, L., Jacobs, C., et al. (2014). The Angelina Jolie effect: How high celebrity profile can have a major impact on provision of cancer related services. Breast Cancer Research: BCR, 16(5), 442-014–40442-6.
Evers, C., Fischer, C., Dikow, N., & Schott, S. (2017). Familial breast cancer: Genetic counseling over time, including patients’ expectations and initiators considering the Angelina Jolie effect. PLoS One, 12(5), e0177893.
Freedman, R., Mountain, H., Karina, D., & Schofield, L. (2017). A retrospective exploration of the impact of the 'Angelina Jolie effect' on the single state-wide familial cancer program in Perth, western Australia. Journal of Genetic Counseling, 26(1), 52–62.
Gammon, A. D., Rothwell, E., Simmons, R., Lowery, J. T., Ballinger, L., Hill, D. A., et al. (2011). Awareness and preferences regarding BRCA1/2 genetic counseling and testing among latinas and non-latina white women at increased risk for hereditary breast and ovarian cancer. Journal of Genetic Counseling, 20(6), 625–638.
Hampel, H., Bennett, R. L., Buchanan, A., Pearlman, R., Wiesner, G. L., & Guideline Development Group, American College of Medical Genetics and Genomics Professional Practice and Guidelines Committee and National Society of Genetic Counselors Practice Guidelines Committee. (2015). A practice guideline from the American College of Medical Genetics and Genomics and the National Society of genetic counselors: Referral indications for cancer predisposition assessment. Genetics in Medicine: Official Journal of the American College of Medical Genetics, 17(1), 70–87.
Health Information National Trends Survey, National Cancer Institute. (2010). HINTS briefs number 16. Retrieved 06/2017, 2017, from https://hints.cancer.gov/docs/Briefs/HINTS_Brief_16.pdf.
Hesse, B. W., Nelson, D. E., Kreps, G. L., Croyle, R. T., Arora, N. K., Rimer, B. K., et al. (2005). Trust and sources of health information: The impact of the internet and its implications for health care providers: Findings from the first health information National Trends Survey. Archives of Internal Medicine, 165(22), 2618–2624.
Hooker, G. W., Clemens, K. R., Quillin, J., Vogel Postula, K. J., Summerour, P., Nagy, R., et al. (2017). Cancer genetic counseling and testing in an era of rapid change. Journal of Genetic Counseling, 26(6), 1244–1253.
Mai, P. L., Vadaparampil, S. T., Breen, N., McNeel, T. S., Wideroff, L., & Graubard, B. I. (2014). Awareness of cancer susceptibility genetic testing: The 2000, 2005, and 2010 National Health Interview Surveys. American Journal of Preventive Medicine, 46(5), 440–448.
Merdad, L., Aldakhil, L., Gadi, R., Assidi, M., Saddick, S. Y., Abuzenadah, A., et al. (2017). Assessment of knowledge about biobanking among healthcare students and their willingness to donate biospecimens. BMC Medical Ethics, 18(1), 32-017–0195-8.
National Consensus Project for Quality Palliative Care Task Force. (2013). In Dahlin C. (Ed.), Clinical practice guidelines for quality palliative care, 3rd ed. Pittsburgh: National Consensus Project for Quality Care.
Nelson, H. D., Pappas, M., Zakher, B., Mitchell, J. P., Okinaka-Hu, L., & Fu, R. (2014). Risk assessment, genetic counseling, and genetic testing for BRCA-related cancer in women: A systematic review to update the U.S. preventive services task force recommendation. Annals of Internal Medicine, 160(4), 255–266.
Quillin, J. M., Silberg, J., Jones, R. M., Wilson, D. B., Maes, H., Bowen, D., et al. (2008a). Tolerance for ambiguity could influence awareness of breast cancer genetic testing and inform health education. Cancer Causes & Control: CCC, 19(10), 1227–1232.
Quillin, J. M., Bodurtha, J. N., & Smith, T. J. (2008b). Genetics assessment at the end of life: Suggestions for implementation in clinic and future research. Journal of Palliative Medicine, 11(3), 451–458.
Quillin, J. M., Bodurtha, J. N., Siminoff, L. A., & Smith, T. J. (2010). Exploring hereditary cancer among dying cancer patients - a cross-sectional study of hereditary risk and perceived awareness of DNA testing and banking. Journal of Genetic Counseling, 19(5), 497–525.
Quillin, J. M., Bodurtha, J. N., & Smith, T. J. (2011a). Genetic screening and DNA banking at the end of life #206. Journal of Palliative Medicine, 14(5), 656–657.
Quillin, J. M., Bodurtha, J. N., Siminoff, L. A., & Smith, T. J. (2011b). Physicians' current practices and opportunities for DNA banking of dying patients with cancer. Journal of Oncology Practice, 7(3), 183–187.
Raphael, J., Verma, S., Hewitt, P., & Eisen, A. (2016). The impact of Angelina Jolie (AJ)'s story on genetic referral and testing at an academic cancer centre in Canada. Journal of Genetic Counseling, 25(6), 1309–1316.
Riley, B. D., Culver, J. O., Skrzynia, C., Senter, L. A., Peters, J. A., Costalas, J. W., et al. (2012). Essential elements of genetic cancer risk assessment, counseling, and testing: Updated recommendations of the National Society of genetic counselors. Journal of Genetic Counseling, 21(2), 151–161.
Roeland, E. J., Dullea, A. D., Hagmann, C. H., & Madlensky, L. (2017). Addressing hereditary cancer risk at the end of life. Journal of Oncology Practice, 13(10), e851–e856.
Rogith, D., Yusuf, R. A., Hovick, S. R., Peterson, S. K., Burton-Chase, A. M., Li, Y., et al. (2014). Attitudes regarding privacy of genomic information in personalized cancer therapy. Journal of the American Medical Informatics Association: JAMIA, 21(e2), e320–e325.
Staudigl, C., Pfeiler, G., Hrauda, K., Renz, R., Berger, A., Lichtenschopf, R., et al. (2016). Changes of socio-demographic data of clients seeking genetic counseling for hereditary breast and ovarian cancer due to the "Angelina Jolie effect". BMC Cancer, 16, 436-016–42472-1.
Zazove, P., Plegue, M. A., Uhlmann, W. R., & Ruffin 4th, M. T. (2015). Prompting primary care providers about increased patient risk as a result of family history: Does it work? Journal of the American Board of Family Medicine: JABFM, 28(3), 334–342.
Funding
This study was funded by the Maryland Cigarette Fund Restitution, administered by the Sidney Kimmel Comprehensive Cancer Center at Johns Hopkins University.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of Interest
John M. Quillin, Oluwabunmi Emidio, Brittany Ma, Lauryn Bailey, Thomas J. Smith, In Guk Kang, Brandon J. Yu, Oluwafemi Patrick Owodunni, Mohammed Abusamaan, Rab Razzak, and Joann N. Bodurtha declare that they have no conflict of interest.
Human Studies and Informed Consent
All procedures followed were in accordance with the ethical standards for human experimentation of the institutional review board at Johns Hopkins University, with national standards, and with the Helsinki Declaration of 1975, as revised in 2000. Informed consent was obtained from all patients being included in the study.
Animal Studies
No animal studies were carried out by the authors of this article.
Rights and permissions
About this article
Cite this article
Quillin, J.M., Emidio, O., Ma, B. et al. High-Risk Palliative Care Patients’ Knowledge and Attitudes about Hereditary Cancer Testing and DNA Banking. J Genet Counsel 27, 834–843 (2018). https://doi.org/10.1007/s10897-017-0181-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10897-017-0181-9