Abstract
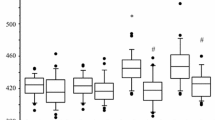
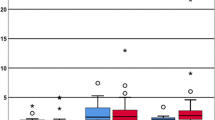
This study was designed to investigate qCON and qNOX variations during outpatient laparoscopic cholecystectomy using remifentanil and desflurane without muscle relaxants and compare these indices with ANI and MAC. Adult patients undergoing outpatient laparoscopic cholecystectomy were included in this prospective observational study. Maintenance of anesthesia was performed using remifentanil targeted to ANI 50–80 and desflurane targeted to MAC 0.8–1.2 without muscle relaxants. The ANI, qCON and qNOX and desflurane MAC values were collected at different time-points and analyzed using repeated measures ANOVA. The relationship between ANI and qNOX and between qCON and MAC were analyzed by linear regression. The ANI was comprised between 50 and 80 during maintenance of anesthesia. Higher values of qNOX and qCON were observed at induction and extubation than during all other time-points where they were comprised between 40 and 60. A poor but significant negative linear relationship (r2 = 0.07, p < 0.001) was observed between ANI and qNOX. There also was a negative linear relationship between qCON and MAC (r2 = 0.48, p < 0.001) and between qNOX and remifentanil infusion rate (r2 = 0.13, p < 0.001). The linear mixed-effect regression correlation (r2) was 0.65 for ANI-qNOX and 0.96 for qCON-MAC. The qCON and qNOX monitoring seems informative during general anesthesia using desflurane and remifentanil without muscle relaxants in patients undergoing ambulatory laparoscopic cholecystectomy. While qCON correlated with MAC, the correlation of overall qCON and ANI was poor but significant. Additionally, the qNOX weakly correlated with the remifentanil infusion rate. This observational study suggests that the proposed ranges of 40–60 for both indexes may correspond to adequate levels of hypnosis and analgesia during general anesthesia, although this should be confirmed by further research.



Similar content being viewed by others
References
Meijer FS, Niesters M, van Velzen M, Martini CH, Olofsen E, Edry R, et al. Does nociception monitor-guided anesthesia affect opioid consumption? A systematic review of randomized controlled trials. J Clin Monit Comput. 2020;34:629–41.
Santonocito C, Noto A, Crimi C, Sanfilippo F. Remifentanil-induced postoperative hyperalgesia: current perspectives on mechanisms and therapeutic strategies. Local Reg Anesth. 2018;11:15–23.
Fletcher D, Martinez V. Opioid-induced hyperalgesia in patients after surgery: a systematic review and a meta-analysis. Br J Anaesth. 2014;112:991–1004.
Jiao Y, He B, Tong X, Xia R, Zhang C, Shi X. Intraoperative monitoring of nociception for opioid administration: a meta-analysis of randomized controlled trials. Minerva Anestesiol. 2019. https://www.minervamedica.it/index2.php?show=R02Y2019N05A0522
Ledowski T. Objective monitoring of nociception: a review of current commercial solutions. Br J Anaesth. 2019;123:e312–21.
Stöckle P-A, Richebé P. Le monitorage de la douleur peropératoire: actualités et perspectives. Anesthésie Réanimation. 2018;4:204–14.
De jonckheere J, Bonhomme V, Jeanne M, Boselli E, Gruenewald M, Logier R, et al. Physiological signal processing for individualized anti-nociception management during general anesthesia: a review. Yearb Med Inform. 2015;24:95–101.
Jeanne M, Clément C, De Jonckheere J, Logier R, Tavernier B. Variations of the analgesia nociception index during general anaesthesia for laparoscopic abdominal surgery. J Clin Monit Comput. 2012;26:289–94.
Jeanne M, Delecroix M, De Jonckheere J, Keribedj A, Logier R, Tavernier B. Variations of the analgesia nociception index during propofol anesthesia for total knee replacement. Clin J Pain. 2014;30:1084–8.
Boselli E, Bouvet L, Bégou G, Torkmani S, Allaouchiche B. Prediction of hemodynamic reactivity during total intravenous anesthesia for suspension laryngoscopy using Analgesia/Nociception Index (ANI): a prospective observational study. Minerva Anestesiol. 2015;81:288–97.
Boselli E, Bouvet L, Allaouchiche B. Monitorage de l’analgésie avec l’Analgesia/Nociception Index: résultats des études cliniques chez les patients éveillés et anesthésiés. EM-Consulte. 2015;19:78–86.
Szental JA, Webb A, Weeraratne C, Campbell A, Sivakumar H, Leong S. Postoperative pain after laparoscopic cholecystectomy is not reduced by intraoperative analgesia guided by analgesia nociception index (ANI ® ) monitoring: a randomized clinical trial. Br J Anaesth. 2015;114:640–5.
Boselli E, Jeanne M. Analgesia: effects on response to nociceptive stimulation. In: Gambús PL, Hendrickx JFA, editors. Personalized anaesthesia. 1st ed. Cambridge: Cambridge University Press;2019. p. 117–27.
Jensen EW, Valencia JF, López A, Anglada T, Agustí M, Ramos Y, et al. Monitoring hypnotic effect and nociception with two EEG-derived indices, qCON and qNOX, during general anaesthesia. Acta Anaesthesiol Scand. 2014;58:933–41.
Melia U, Gabarron E, Agustí M, Souto N, Pineda P, Fontanet J, et al. Comparison of the qCON and qNOX indices for the assessment of unconsciousness level and noxious stimulation response during surgery. J Clin Monit Comput. 2017;31:1273–81.
Lewis SR, Pritchard MW, Fawcett LJ, Punjasawadwong Y. Bispectral index for improving intraoperative awareness and early postoperative recovery in adults. Cochrane Anaesthesia Group, editor. Cochrane Database Syst Rev. 2019. https://doi.org/10.1002/14651858.CD003843.pub4
Abbott TEF, Pearse RM. Depth of anesthesia and postoperative delirium. JAMA. 2019;321:459–60.
Myles P, Leslie K, McNeil J, Forbes A, Chan M. Bispectral index monitoring to prevent awareness during anaesthesia: the B-Aware randomised controlled trial. Lancet. 2004;363:1757–63.
Avidan MS, Searleman AC, Bottros M. Anesthesia awareness and the bispectral index. N Engl J Med 2008;12.
El-Radaideh K, Dheeb E, Shbool H, Garaibeh S, Bataineh A, Khraise W, et al. Evaluation of different airway tests to determine difficult intubation in apparently normal adult patients undergoing surgical procedures. Patient Saf Surg. 2020;14:43.
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. 2007;370:1453–7.
Boselli E, Intubation without NMBA: first optimise opioid dose. Comment on Br J Anaesth. 120: 1150–3. Br J Anaesth. 2018;2019(122):e9-10.
Bouvet L, Stoian A, Rimmelé T, Allaouchiche B, Chassard D, Boselli E. Optimal remifentanil dosage for providing excellent intubating conditions when co-administered with a single standard dose of propofol. Anaesthesia. 2009;64:719–26.
Jalota L, Kalira V, George E, Shi Y-Y, Hornuss C, Radke O, et al. Prevention of pain on injection of propofol: systematic review and meta-analysis. BMJ. 2011;342:d1110–d1110.
Roth D, Pace NL, Lee A, Hovhannisyan K, Warenits A-M, Arrich J, et al. Airway physical examination tests for detection of difficult airway management in apparently normal adult patients. Cochrane Anaesthesia Group, editor. Cochrane Database Syst Rev. 2018. https://doi.org/10.1002/14651858.CD008874.pub2
Peng K, Ji F, Liu H, Wu S. Ultrasound-guided transversus abdominis plane block for analgesia in laparoscopic cholecystectomy: a systematic review and meta-analysis. Med Princ Pract. 2016;25:237–46.
Boselli E, Logier R, Bouvet L, Allaouchiche B. Prediction of hemodynamic reactivity using dynamic variations of Analgesia/Nociception Index (∆ANI). J Clin Monit Comput. 2016;30:977–84.
Sridharan K, Sivaramakrishnan G. Drugs for preventing post-operative nausea and vomiting in patients undergoing laparoscopic cholecystectomy: network meta-analysis of randomized clinical trials and trial sequential analysis. Int J Surg. 2019;69:1–12.
Köprülü AŞ, Haspolat A, Gül YG, Tanrikulu N. Can postoperative pain be predicted? New parameter: analgesia nociception index. Turk J Med Sci. 2020;50.
Gonzalez-Cava JM, Arnay R, León A, Martín M, Reboso JA, Calvo-Rolle JL, et al. Machine learning based method for the evaluation of the Analgesia Nociception Index in the assessment of general anesthesia. Comput Biol Med. 2020;118: 103645.
Anderson TA, Segaran JR, Toda C, Sabouri AS, De Jonckheere J. High-frequency heart rate variability index: a prospective, observational trial assessing utility as a marker for the balance between analgesia and nociception under general anesthesia. Anesth Analg. 2020;130:1045–53.
Christenson C, Martinez-Vazquez P, Breidenstein M, Farhang B, Mathews J, Melia U, et al. Comparison of the Conox (qCON) and Sedline (PSI) depth of anaesthesia indices to predict the hypnotic effect during desflurane general anaesthesia with ketamine. J Clin Monit Comput. 2020. https://doi.org/10.1007/s10877-020-00619-3
Müller JN, Kreuzer M, García PS, Schneider G, Hautmann H. Monitoring depth of sedation: evaluating the agreement between the Bispectral Index, qCON and the Entropy Module’s State Entropy during flexible bronchoscopy. Minerva Anestesiol. 2017;83:563–73.
Tacquard C, Collange O, Gomis P, Malinovsky J-M, Petitpain N, Demoly P, et al. Anaesthetic hypersensitivity reactions in France between 2011 and 2012: the 10th GERAP epidemiologic survey. Acta Anaesthesiol Scand. 2017;61:290–9.
Desai N, Kirkham KR, Albrecht E. Local anaesthetic adjuncts for peripheral regional anaesthesia: a narrative review. Anaesthesia. 2021;76:100–9.
Raval AD, Deshpande S, Koufopoulou M, Rabar S, Neupane B, Iheanacho I, et al. The impact of intra-abdominal pressure on perioperative outcomes in laparoscopic cholecystectomy: a systematic review and network meta-analysis of randomized controlled trials. Surg Endosc. 2020;34:2878–90.
Gurusamy KS, Vaughan J, Davidson BR. Low pressure versus standard pressure pneumoperitoneum in laparoscopic cholecystectomy. Cochrane Hepato-Biliary Group, editor. Cochrane Database Syst Rev. 2014.https://doi.org/10.1002/14651858.CD006930.pub3
Ledowski T. Muscle relaxation in laparoscopic surgery: what is the evidence for improved operating conditions and patient outcome? A brief review of the literature. Surg Laparosc Endosc Percutan Tech. 2015;25:5.
Boon M, Martini CH, Aarts LPHJ, Dahan A. The use of surgical rating scales for the evaluation of surgical working conditions during laparoscopic surgery: a scoping review. Surg Endosc. 2019;33:19–25.
Graça R, Lobo FA. Analgesia Nociception Index (ANI) and ephedrine: a dangerous liasion. J Clin Monit Comput. 2021;35:953–4.
Acknowledgements
The authors wish to thank Dr Luca Guizouarn, Dr Quentin Darnajoux, Dr Stefano Pigella, Dr Jennifer Rocher and Dr Sarah Touama for their participation in the study.
Funding
This study was performed with institutional sources. The CONOX© monitor and electrodes were supplied by Fresenius Kabi France during the time of the study.
Author information
Authors and Affiliations
Contributions
TP made substantial contribution to the acquisition and interpretation of data for the work, drafted the work, approved the final version to be published and agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. BA made substantial contribution to the acquisition of data for the work, revised the work critically for important intellectual content, approved the final version to be published and agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. EB made substantial contribution to the design of the work and on the acquisition, analysis and interpretation of data for the work, revised the work critically for important intellectual content, approved the final version to be published and agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Conflict of interest
Bernard Allaouchiche and Emmanuel Boselli have received honoraria from Fresenius Kabi.
Consent to participate
All participants provided written inform consent to participate to this study.
Ethical approval
The study was promoted by the Centre hospitalier Pierre Oudot and approved by the Ethics Committee (Centre de Protection des Personnes Île-de-France XI, Approval No. 20015–62544).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Pantalacci, T., Allaouchiche, B. & Boselli, E. Relationship between ANI and qNOX and between MAC and qCON during outpatient laparoscopic cholecystectomy using remifentanil and desflurane without muscle relaxants: a prospective observational preliminary study. J Clin Monit Comput 37, 83–91 (2023). https://doi.org/10.1007/s10877-022-00861-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-022-00861-x