Abstract
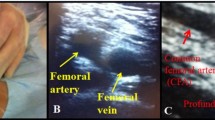
Ultrasound-guided vascular access is a technique that can increase safety as well as technical and procedural success when performing invasive cardiovascular procedures. The aim of this study was to evaluate the effects of two cannulation techniques and vascular morphological properties on the success of femoral artery catheterisation in neonatal patients. We recruited 65 consecutive patients requiring femoral artery catheterisation and randomly divided them into two groups: Group 1, in-plane technique (n = 31) and Group 2, out-of-plane technique (n = 34). We compared the preparation duration, puncture duration, number of punctures, number of arterial punctures, number of unsuccessful interventions, hematoma incidence and vascular morphological characteristics between the groups. The mean age of Group 1 was 17.16 ± 7.04 days, and the mean age of Group 2 was 17.20 ± 7.40 days, with no difference observed between the groups (p > 0.05). Four patients in Group 1 and nine patients in Group 2 developed hematoma (p = 0.172). Hematoma was strongly correlated with the number of venous punctures (r = 0.632; p = 0.001) and the number of needle advancements (r = 0.415; p = 0.001). In terms of artery–vein position, patients whose artery overlapped the vein by > 50% required clearly longer artery cannulation durations than the other patients (p < 0.001). Although the in-plane technique has a steep learning curve, it was found superior in terms of procedure-related factors such as the number of trials, the incidence of hematoma and arterial puncture counts, as it offers advantages such as the ability to evaluate the lumen and a better control of the needle advancement direction.


Similar content being viewed by others
References
Ang H, Veldman A, Lewis A, Carse E, Wong FY. Procedural training opportunities for basic pediatric trainees during a 6-month rotation in a level III perinatal centre in Australia. J Matern Fetal Neonatal Med. 2012;25(11):2428–31.
Bhatia N, Sivaprakasam J, Allford M, Guruswamy V. The relative position of femoral artery and vein in children under general anesthesia–an ultrasound-guided observational study. Paediatr Anaesth. 2014;24(11):1164–8.
National Institute for Clinical Excellence. Acutely ill patients in hospital overview. www.nice.org.uk. Accessed May, 2019
Troianos CA, Hartman GS, Glas KE, Skubas NJ, Eberhardt RT, Walker JD, Reeves ST, Councils on Intraoperative Echocardiography, and Vascular Ultrasound of the American Society of Echocardiography; Society of Cardiovascular Anesthesiologists. Special articles: guidelines for performing ultrasound guided vascular cannulation: recommendations of the American Society of Echocardiography and the Society of Cardiovascular Anesthesiologists. Anesth Analg. 2012;114(1):46–72.
American Institute of Ultrasound in Medicine. AIUM practice guideline for the use of ultrasound to guide vascular access, procedures. J Ultrasound Med. 2013;32(1):191–21515.
Berk D, Gurkan Y, Kus A, Ulugol H, Solak M, Toker K. Ultrasound-guided radial arterial cannulation: long axis/in-plane versus short axis/out-of-plane approaches? J Clin Monit Comput. 2013;27(3):319–24.
Warkentine FH, Clyde Pierce M, Lorenz D, Kim IK. The anatomic relationship of femoral vein to femoral artery in euvolemic pediatric patients by ultrasonography: implications for pediatric femoral central venous access. Acad Emerg Med. 2008;15(5):426–30.
Hopkins JW, Warkentine F, Gracely E, Kim IK. The anatomic relationship between the common femoral artery and common femoral vein in frog leg position versus straight leg position in pediatric patients. Acad Emerg Med. 2009;16(7):579–84.
Bruzoni M, Slater BJ, Wall J, St Peter SD, Dutta S. A prospective randomized trial of ultrasound-vs landmark-guided central venous access in the pediatric population. J Am Coll Surg. 2013;216(5):939–43.
Suk EH, Lee KY, Kweon TD, Jang YH, Bai SJ. Ultrasonographic evaluation of the femoral vein in anaesthetised infants and young children. Anesthesia. 2010;65(9):895–8.
Sethi S, Maitra S, Saini V, Samra T, Malhotra SK. Comparison of short-axis out-of-plane versus long-axis in-plane ultrasound-guided radial arterial cannulation in adult patients: a randomized controlled trial. J Anesth. 2017;31(1):89–94.
Kayashima K, Ueki M, Kinoshita Y. Ultrasonic analysis of the anatomical relationships between vertebral arteries and internal jugular veins in children. Paediatr Anaesth. 2012;22(9):854–8.
Kanter RK, Gorton JM, Palmieri K, Tompkins JM, Smith F. Anatomy of femoral vessels in infants and guidelines forvenous catheterization. Pediatrics. 1989;83(6):1020–2.
Aouad MT, Kanazi GE, Abdallah FW, Moukaddem FH, Turbay MJ, Obeid MY, Siddik-Sayyid SM. Femoral vein cannulation performed by residents: a comparison between ultrasound guided and landmark technique in infants and children undergoing cardiac surgery. Anesth Analg. 2010;111(3):724–8.
Song IK, Choi JY, Lee JH, Kim EH, Kim HJ, Kim HS, Kim JT. Short-axis/out-of-plane or long-axis/in-plane ultrasound-guided arterial cannulation in children: a randomised controlled trial. Eur J Anaesthesiol. 2016;33(1):522–7.
Lv Y, Liu H, Yu P, Wang G, Liu M, Li Y, Wang H, Yu K, Wang C. Evaluating the long-, short-, and oblique-axis approaches for ultrasound-guided vascular access cannulation. J Ultrasound Med. 2019;38(2):347–55.
Gao YB, Yan JH, Ma JM, Liu XN, Dong JY, Sun F, Tang LW, Li J. Effects of long axis in-plane vs short axis out-of-plane techniques during ultrasound-guided vascular access. Am J Emerg Med. 2016;34(5):778–83.
French JLH, Raine-Fenning NJ, Hardman JG, Bedforth NM. Pitfalls of ultrasound guided vascular access: the use of three/four-dimensional ultrasound. Anaesthesia. 2008;63(8):806–13.
Blaivas M, Brannam L, Fernandez E. Short-axis versus long-axis approaches for teaching ultrasound-guided vascular access on a new inanimate model. Acad Emerg Med. 2003;10(12):1307–11.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare have no conflict of interests or financial ties to disclose.
Research involving human participants
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Boran, O.F., Urfalıoglu, A., Arslan, M. et al. Effects of vascular morphological features and ultrasound-guided vascular cannulation techniques on the success of femoral artery catheterisation in newborns. J Clin Monit Comput 34, 607–614 (2020). https://doi.org/10.1007/s10877-020-00490-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-020-00490-2