Abstract
Purpose
In order to assess the occurrence of blood congestion in the liver during liver resection, we aimed to evaluate the influence of a positive-end-expiratory-pressure (PEEP) and positioning of patients on central venous pressure (CVP) and venous hepatic blood flow parameters. We further analyzed correlations between CVP and venous hepatic blood flow parameters.
Methods
In 20 patients scheduled for elective liver resection we measured CVP and quantified venous hepatic hemodynamics by ultrasound assessment of flow-velocity and diameter of the right hepatic vein and the portal vein after equilibration following these maneuvers: M1: 0° supine position, PEEP 0 cmH2O; M2: 0° supine position, PEEP 10 cmH2O; M3: 20° reverse-trendelenburg position; PEEP 10 cmH2O; M4: 20° reverse-trendelenburg position, PEEP 0cmH2O.
Results
Changing from supine to reverse-trendelenburg position led to a significant decrease in CVP (M3 5.95 ± 2.06 vs. M1 7.35 ± 2.18 mmHg and M2 8.55 ± 1.79 mmHg). A PEEP of 10 cmH2O and reverse-trendelenburg position led to significant reduction of systolic (VsHV) and diastolic (VdHV) flow-velocities of the right hepatic vein (VsHV M3 19.96 ± 6.47 vs. M1 27.81 ± 11.03 cm s−1;VdHV M3 14.94 ± 6.22 vs. M1 20.15 ± 10.34 cm s−1 and M2 20.19 ± 13.19 cm s−1) whereas no significant changes of flow-velocity occurred in the portal vein. No correlations between CVP and diameters or flow-velocities of the right hepatic and the portal vein were found.
Conclusions
Changes of central venous pressure due to changes of PEEP and positioning were not correlated with changes of venous hepatic blood flow parameters as measured after equilibration. Strategies aiming for low central venous pressure cannot be supported by these results. However, before ruling out low-CVP-strategies during liver resections these results should be confirmed by further studies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Mainly due to surgical improvements over the past years blood loss during hepatic surgery could be reduced [1]. Minimizing blood loss during liver resection is of special interest since reduced blood loss and fewer requirements for blood transfusions are associated with improved postoperative outcome and reduced long-term morbidity and mortality [1–5].
One generally used approach for minimization of blood loss is to decrease central venous pressure (CVP) [6–10]. The rationale for this concept is that high CVP is supposed to impede hepatic venous outflow [11]. If not accompanied by a reduction of portal venous inflow high CVP would induce hepatic blood congestion leading to increased transmural pressure and thereby vessel distension and could promote blood loss during parenchymal resection [9]. In this context lowering CVP by lowering positive-end-expiratory-pressure (PEEP) and bringing the patient in reverse-trendelenburg position frequently are believed to be associated with reduced CVP and improved venous hepatic blood drainage [6, 10, 12, 13]. However, so far the effects of these maneuvers on the resulting venous hepatic blood flow and blood congestion has not conclusively been validated.
Therefore, in this study we aimed to evaluate the influence of PEEP and patient positioning on CVP and venous hepatic blood flow. We quantified venous hepatic blood flow parameters by ultrasonic based assessment of hepatic venous and portal venous diameter and flow-velocities. Further, we correlated CVP to venous hepatic blood flow parameters in order to assess the association of CVP and changes of CVP to hepatic venous blood flow and hepatic venous dilatation.
2 Methods
2.1 IRB/consent
This prospective observational study was approved by the Ethics Committee of the Medical Board of Hamburg (PV4617). All patients gave written informed consent for participation in this study.
2.2 Patient enrollment
We included patients scheduled for elective hepatic surgery (hemihepatectomy, atypical liver resection or explorative laparotomy for evaluation of liver tumors). Exclusion criteria were former liver resection, liver cirrhosis, portal vein embolization and former liver transplantation. Further, patients with atrial fibrillation during measurements, moderate to severe tricuspid valve regurgitation [14], heart failure ≥NYHA III [15], renal failure ≥stage III according to the KDIGO classification [16], dislocation of the central venous catheters—as verified by chest X-Ray—or refusal of consent were excluded.
2.3 Anesthesia and instrumentation
All patients enrolled into study received premedication with midazolam (between 3.75 and 7.5 mg orally) approximately 1 h before transfer into the operating room. We monitored patients with a 5-lead ECG, non-invasive oscillometric blood-pressure measurement and pulse oxymetry prior to induction of anesthesia. In patients without contraindications for epidural anesthesia we inserted a thoracic epidural catheter at Th 6/7 or Th 7/8 and administered bupivacaine and sufentanil according to our clinical standard. We induced general anesthesia with sufentanil 0.7 µg kg−1 and propofol 1–2 mg kg−1. We used rocuronium 0.6 mg kg−1 for muscle relaxation to facilitate orotracheal intubation and maintained anesthesia with inhalative sevoflurane with concentrations of 2% expiratory. We administered additional doses of rocuronium for proper muscle relaxation during measurements. We placed an arterial line in the radial artery and a central venous catheter either in the right or left internal or external jugular vein respectively. Correct localization of central venous catheters was assessed by chest X-ray after surgery defining catheter tip position at approximately tracheal bifurcation level as correct.
2.4 Study protocol
We assessed cardiac index (CI) and stroke volume variation (SVV) with pulse-contour analysis (ProAQT, Pulsion Medical Systems® or Vigileo Monitor, Edward Lifesciences®). Before measurements and after every change of position we zeroed central venous and arterial catheters to ambient pressure at right atrium level. We performed ventilation using pressure controlled ventilation (volume auto flow mode, Primus, Dräger Medical®) with tidal volumes of 7 ml kg−1 body weight. We adjusted respiratory rates to keep end tidal carbon dioxide between 35 and 45 mmHg and kept the I:E ratio between 1:1.5 and 1:2. We monitored heart rate, mean arterial blood pressure, cardiac index, stroke volume variation, respiratory rate, tidal volume, airway pressure and pulmonary compliance for every measurement point. We optimized hemodynamics on the basis of current concepts [17, 18]. We performed fluid administration with crystalloids (Sterofundin, Braun®) to achieve a SVV ≤ 10%. We administered norepinephrine to maintain a mean arterial pressure above 65 mmHg. We used dobutamine if necessary to keep cardiac index ≥2 l min−1 (m2 bsa)−1. We controlled positioning with a digital water level. All measurements with an equilibration time of 5 min in between were done before skin incision as follows: M1: 0° supine position, PEEP 0 cmH2O; M2: 0° supine position, PEEP 10 cmH2O; M3: 20° reverse-trendelenburg position, PEEP 10 cmH2O; M4: 20° reverse-trendelenburg position, PEEP 0 cmH2O.
2.5 Central venous pressure measurements
We measured central venous pressure using a central venous line inserted as described above. We connected a pressure transducer to the central venous line and zeroed the pressure transducers at all measurement steps to the right atrial level using a fluid filled pressure line fixed at the ventral 2/5 part of the patients’ chest diameter at level of the fifth rib. The pressure transducer was connected to the Dräger Infinity Delta® patient monitor system. This monitor system analyses the CVP online and displays the mean CVP value for a time interval of 16 s. The CVP values were recorded after an equilibration time of 5 min parallel to the ultrasonic measurements.
2.6 Ultrasonic measurements
We performed all ultrasonic measurements using a standardized protocol. The same experienced investigator performed all measurements to exclude interobserver variability and maximize test–retest reliability. The investigator was aware of the protocol. We used an ultrasound machine with a curved array ultrasonic probe (Logiq 7 Ultrasound machine, GE Healthcare®; Logiq 7 4C ultrasound transducer, GE Healthcare®). Doppler angle correction [19] was used whenever the axis of the ultrasound beam was not in line with the longitudinal axis of the vessel or direction of flow. All ultrasonic measurements were performed after an equilibration time of 5 min. Flow-velocity was measured instead of directly measured blood flow according to its non-invasiveness. We measured flow-velocity of the right hepatic vein and the portal vein for every measurement period using pulsed-wave Doppler-ultrasound. We performed ultrasound evaluation of the portal vein and the right hepatic vein flow-velocities in the center of the vessel. After receiving stable flow-velocities over four to five heart-cycles the picture was freezed and the flow-velocity measured. Right hepatic vein was chosen since it has the biggest diameter and is easy to access with ultrasound without much need for Doppler angle correction. It was measured intra-hepatic at 2 cm proximal to the confluence. Under normal circumstances the right hepatic vein has a triphasic flow profile consisting of two anterograde directed velocities (Vshv and Vdhv) and one retrograde directed velocity (Vahv) or a biphasic flow profile without a retrograde directed flow-velocity (Fig. 1). The portal vein has a monophasic flow profile consisting of an anterograde directed flow-velocity (Vmaxpv). As surrogate for liver blood congestion we collected ultrasonic diameters of the right hepatic vein (diameterhv) and the portal vein (diameterpv).
Relationship of electrocardiogramm, central venous pressure and hepatic vein flow-velocity. ECG electrocardiogramm, CVP central venous pressure, HV hepatic vein, a a-wave, c c-wave, v v-wave, Va HV retrograde directed flow-velocity wave, Vs hv systolic flow-velocity wave, Vd hv diastolic flow-velocity wave
2.7 Statistical analysis
Results are expressed as means ± standard deviation (SD) unless otherwise stated. We performed statistical analysis using SPSS Statistics 22 (IBM®). To test for differences between measurement points we used ANOVA with position/PEEP as independent variable. Furthermore we adjusted for epidural anesthesia by including it as additional independent variable. Variables were log transformed if necessary. A p-value <0.05 was defined as significant. To analyze correlations we calculated the Pearson correlation coefficient.
2.8 Results
2.9 Study group
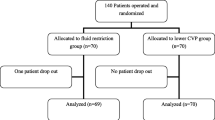
22 patients were enrolled in this study. Two patients had to be excluded due to malpositioned central venous catheters, as verified by chest radiograph. In total data of 20 patients was analyzed (11 male, 9 female). Patients suffered from hepatocellular or cholangiocellular carcinoma, colorectal metastases and hepatocellular adenoma. The mean body weight was 78.5 ± 16.57 and the mean age in years was 59.45 ± 14.47.
2.10 General hemodynamics and ventilation
Results of hemodynamic measurements and ventilatory data are shown in Table 1. There were no significant changes in heart rate, mean arterial pressure, cardiac index and stroke volume variation respectively. No significant changes occurred regarding tidal volume, respiratory rates and pulmonary compliance respectively. Increases of PEEP were accompanied by significant increases of peak-pressure. The combination of reverse-trendelenburg position with PEEP 0 cmH2O resulted in a significant decrease of peak-pressure compared with all other measurement points.
2.11 Vasopressor and inotropic use
In two patients dobutamine was administered additionally at a dose of 3 µg kg−1min−1 to obtain a cardiac index above 2 l min−1 (m2 bsa)−1. All patients received norepinephrine between 0.01 and 0.35 µg kg−1min−1 with a mean dosage of 0.11 ± 0.07 µg kg−1min−1. There were no significant changes in norepinephrine dosage due to PEEP or positioning.
2.12 Central venous pressure and venous hepatic hemodynamics
CVP and venous hepatic hemodynamics are shown in Table 2 and Fig. 2. In supine position increase of PEEP had no significant effect on CVP. Movement of the patient from supine to reverse-trendelenburg position was accompanied by a significant decrease in CVP compared with supine position. Reduction of PEEP from 10 to 0 cmH2O in reverse-trendelenburg position further decreased CVP significantly. Ultrasound analysis of the right hepatic vein and the portal vein showed diameters in physiological range [19]. None of the interventions could evoke significant changes in the diameters of the right hepatic or portal vein. There were no significant changes of flow-velocity of the hepatic vein due to increase of PEEP in supine position. The combination of PEEP 10 cmH2O and reverse-trendelenburg position led to significant decreases of Vshv and Vdhv compared with supine position and PEEP 0 cmH2O. Vdhv was also significantly decreased compared with supine position and PEEP 10 cmH2O. There were no significant changes in Vahv at any time point. No significant changes of flow-velocity of the portal vein occurred due to PEEP and positioning.
Central venous pressure versus flow-velocities of the right hepatic vein and portal vein. CVP central venous pressure; HV right hepatic vein; M measurement point; PV portal vein; RT 20° reverse-trendelenburg position; SP supine position; Va HV a-wave flow-velocity right hepatic vein; Vd HV d-wave flow-velocity right hepatic vein; Vmax PV maximum flow-velocity portal vein; Vs HV s-wave flow-velocity right hepatic vein. M1 0° supine position, PEEP 0 cmH2O; M2 0° supine position, PEEP 10 cmH2O; M3 20° reverse-trendelenburg position, PEEP 10 cmH2O; M4 20° reverse-trendelenburg position, PEEP 0 cmH2O. Error bars present ± standard deviation (SD). *p < 0.05 versus M1, †p < 0.05 versus M2. **p ≤ 0.01 versus M1, ††p ≤ 0.01 versus M2, ‡‡p ≤ 0.01 versus M3
2.13 Correlation analysis
No correlations could be shown between CVP and the flow-velocities of the right hepatic vein and the portal vein. Furthermore, no correlations were found between CVP and the diameters of the right hepatic and the portal vein.
3 Discussion
This prospective study compared changes of central venous pressure with changes in venous hepatic blood flow and hepatic vessel diameters due to different PEEP levels and positioning. No correlation was found between CVP and the diameters and flow-velocities of the right hepatic vein and the portal vein.
Since increased bleeding is correlated with increased mortality reduction of blood loss is one of the main issues in the perioperative management during liver resections [1–5]. Low central venous pressures are supposed to be associated with less blood loss and a reduction of blood transfusion rates [7, 8]. Reduced central venous pressures are believed to improve venous return from the liver [11]. Although hepatic inflow has to be considered, reduced blood congestion could be the consequence. Since blood loss depends on transmural pressure and vessel diameters facilitated venous return from the liver could be crucial for blood loss limitation [9]. Based on this concept low central venous pressure strategies are frequently used for liver resections [20]. Therefore various interventions such as reduction of positive-end-expiratory-pressure [12] or reversed-trendelenburg positioning of the patient have been implemented [10]. However, several studies failed to show the correlation between high CVP and increased blood loss [21–23]. In line with former studies analyzing the effects of PEEP and body positioning on CVP [10, 13, 24–27] our findings showed that a change from supine to reverse-trendelenburg position was effective for reducing CVP. The combination of reverse-trendelenburg position with a reduction of PEEP further decreased CVP. However, the effect of PEEP in supine position on CVP was not significant.
Even though positioning and PEEP had a significant influence on CVP, vessel diameters of the right hepatic vein and the portal vein remained unchanged assessed by ultrasound evaluation. Since low CVP is known to result in an increase of venous return [11] this might be surprising. Reduced blood congestion might be expected resulting in decreased vessel diameters. However, in our study the diameter of the right hepatic vein and the portal vein were not correlated with CVP. It may be assumed that the changes of CVP in our study were not severe enough to effectively influence the vessel diameters. This could suggest that moderate changes in CVP do not induce congestion of blood in the liver.
Blood flow in the liver cannot directly be assessed by ultrasound. Given constant vessel diameters and a constant heart rate flow-velocity might be used as a surrogate of the hepatic blood flow. The risk of bleeding should be increased by either a decrease of venous return from the liver to the heart or by an increase of blood flow towards the liver. In our study blood flow into the liver was assessed by flow-velocity in the portal vein and venous return from the liver by flow-velocity in the right hepatic vein.
Since flow-velocity in the right hepatic vein was lowest during reverse-trendelenburg and PEEP 10 cmH2O, while flow-velocity in the portal vein was unchanged, it might be assumed, that congestion of blood in the liver was at its peak in this constellation. This is of particular interest since reverse-trendelenburg position is a frequently performed maneuver in clinical practice to reduce CVP in order to reduce blood loss. This is possibly explained by the fact that in reverse-trendelenburg position a major part of the liver is underneath the patients center of gravity reducing venous return and promoting liver congestion while CVP was measured with a central venous line above the center of gravity leading to a reduced measured CVP. Our results suggest two issues: firstly the commonly performed reverse-trendelenburg position does not mandatorily result in reduced congestion of blood in the liver and secondly a lowered CVP is not a proper parameter to predict reduced blood congestion of the liver. This is in line with results from Sand and colleagues [13], who could not find a correlation between CVP and portal or hepatic venous pressure due to changes from supine to reverse-trendelenburg position. When PEEP was reduced in reverse-trendelenburg position the CVP was further reduced, while the flow-velocities where not significantly changed. Since the diameter of the right hepatic vein was also unchanged, it has to be assumed that the gradient between CVP and the right hepatic venous pressure was unchanged as well and therefor might indicate a decrease in right hepatic venous pressure at this constellation.
Looking at the influence of PEEP there was no effect on flow-velocity and vein diameter of the right hepatic vein and the portal vein. This is in line with other studies assessing the influence of PEEP on hepatic vein flow-velocity [25–27]. While experimental studies have shown a reduction of portal venous flow due to PEEP this was considered primarily the consequence of reduced cardiac output [28, 29]. Under cardiac output maintenance in our study PEEP had no effect on portal venous flow-velocity and diameter. Therefore, looking at our results in supine position the application of PEEP should not lead to congestion of blood in the liver. More precisely our study indicates that in supine position the application of PEEP under normalized cardiac output should have no effect on blood loss.
Our study has certain limitations. Major limitation of our study is that all measurements were performed while the abdomen was still closed. The opening of the abdomen may lead to a reduction of the abdominal pressure, which may have influenced liver hemodynamics. The advantages of measuring before surgery were that measurements could be taken almost at the same time after beginning of anesthesia and before any bleeding due to surgical preparation occurred. Moreover liver resections are increasingly performed using laparoscopic techniques [30]. In this context the influence of open surgery vs. laparoscopic surgery on liver hemodynamics and CVP should be focused in further studies. Also it has to be addressed that the investigator was not blinded to the protocol and the number of patients examined was rather small. Nevertheless differences concerning CVP were significant and we also observed significant changes in flow-velocity.
As we did not measure flow and diameters of the hepatic artery, our study cannot predict total hepatic blood flow and its influence on hepatic blood congestion. However important determining factors of arterial blood flow such as cardiac index, mean arterial pressure and vasopressor use were not significantly changed. In addition, we did not measure portal venous or hepatic venous resistance. Although the hepatic venous pressure was not directly assessed here, our results indicate that the hepatic venous pressure was reduced when PEEP was reduced combined with reversed-trendelenburg positioning. However, this has yet to be proven by direct measurements of hepatic venous pressure. We did measure flow-velocities instead of directly measured flow of the hepatic and portal vein. Moreover, we did not measure the flow-velocity time integral which would have been more stable to resistance-changes. Although factors influencing flow-velocity such as diameters, catecholamine-doses, heart rate or other parameters of global hemodynamics were not significantly changed, measuring flow-velocity instead of flow has to be seen clearly as a limitation of this study. Since we did measure the flow-velocity randomly over the ventilation cycle and did not adjust the measurement to a certain part of ventilation, ventilator induced changes in intrathoracic pressure could have influenced flow-velocity measurements and this has to be considered as limitation. Since all measurements were performed after an equilibration time of 5 min we did not register acute effects after PEEP and position changes. It is most likely that changes in liver hemodynamics did occur soon after PEEP and position changes leading to changes in liver in- and outflow. Thereafter a new steady-state is reached. It is important to take into account that our measurements represent these equilibrated venous hepatic blood flow parameters. The reduced CVP due to this maneuvers is normally maintained for the whole resection time and therefore the equilibrated changes measured here are of clinical interest. Nevertheless, the acute changes are of interest for some clinical situations and are important for further studies and therefor the limitation of measuring venous hepatic blood flow parameters after allowing 5 min of equilibration should be taken into account. Furthermore, to reflect daily clinical practice we used standard clinical methods to assess CVP and avoided to measure CVP directly by pressure tip catheters due to its high invasiveness. Since ventilation influences CVP our results could have been also affected by the respiratory cycle. However, since our CVP values are the mean value of a 16 s interval this influence should have been of low clinical relevance. Although our study gives some hints for possible increases of bleeding risk under certain circumstances, we did not investigate the effect of changes in liver hemodynamics on blood loss directly. Further studies should investigate the relationship between bleeding risk and venous as well as arterial liver hemodynamics. In our study nine patients received epidural anesthesia while the remaining 11 patients were not equipped with an epidural catheter. Epidural anesthesia could have influenced liver hemodynamics and even more CVPs. Therefore we adjusted the statistical models for the effect of epidural anesthesia.
4 Conclusion
Changes of central venous pressure due to changes of PEEP and positioning were not correlated with significant changes of venous hepatic blood flow parameters. Therefore, these data questions the assumption that changes in CVP following those maneuvers can indicate venous unloading within the hepatic veins as measured after an equilibration period. Before ruling out modulation of CVP as a strategy during liver resection, the changes in venous hepatic blood flow parameters using actual flow measurement and measured soon after CVP changes should be taken into consideration. The impact of reverse-trendelenburg positioning and application of different PEEP levels on intraoperative blood loss was not assessed here.
References
Poon RT, Fan ST, Lo CM, Liu CL, Lam CM, Yuen WK, Yeung C, Wong J. Improving perioperative outcome expands the role of hepatectomy in management of benign and malignant hepatobiliary diseases: analysis of 1222 consecutive patients from a prospective database. Ann Surg. 2004;240(4):698–708.
Katz SC, Shia J, Liau KH, Gonen M, Ruo L, Jarnagin WR, Fong Y, D’Angelica MI, Blumgart LH, Dematteo RP. Operative blood loss independently predicts recurrence and survival after resection of hepatocellular carcinoma. Ann Surg. 2009;249(4):617–23.
Yang T, Zhang J, Lu JH, Yang GS, Wu MC, Yu WF. Risk factors influencing postoperative outcomes of major hepatic resection of hepatocellular carcinoma for patients with underlying liver diseases. World J Surg. 2011;35(9):2073–82.
de Boer MT, Molenaar IQ, Porte RJ. Impact of blood loss on outcome after liver resection. Dig Surg. 2007;24(4):259–64.
Kooby DA, Stockman J, Ben-Porat L, Gonen M, Jarnagin WR, Dematteo RP, Tuorto S, Wuest D, Blumgart LH, Fong Y. Influence of transfusions on perioperative and long-term outcome in patients following hepatic resection for colorectal metastases. Ann Surg. 2003;237(6):860–9.
Jones RM, Moulton CE, Hardy KJ. Central venous pressure and its effect on blood loss during liver resection. Br J Surg. 1998;85(8):1058–60.
Johnson M, Mannar R, Wu AV. Correlation between blood loss and inferior vena caval pressure during liver resection. Br J Surg. 1998;85(2):188–90.
Wang WD, Liang LJ, Huang XQ, Yin XY. Low central venous pressure reduces blood loss in hepatectomy. World J Gastroenterol. 2006;12(6):935–9.
Melendez JA, Arslan V, Fischer ME, Wuest D, Jarnagin WR, Fong Y, Blumgart LH. Perioperative outcomes of major hepatic resections under low central venous pressure anesthesia: blood loss, blood transfusion, and the risk of postoperative renal dysfunction. J Am Coll Surg. 1998;187(6):620–5.
Soonawalla ZF, Stratopoulos C, Stoneham M, Wilkinson D, Britton BJ, Friend PJ (2008) Role of the reverse-Trendelenberg patient position in maintaining low-CVP anaesthesia during liver resections. Langenbeck’s Arch Surg. 393(2):195–8.
Gelman S. Venous function and central venous pressure: a physiologic story. Anesthesiology. 2008;108(4):735–48.
Stümpfle R, RIga A, Deshpande R, Mudan SS, Baikady RR. Anaesthesia for metastatic liver resection surgery. Curr Anesth Crit Care. 2009;20:3–7.
Sand L, Rizell M, Houltz E, Karlsen K, Wiklund J, Odenstedt Herges H, Stenqvist O, Lundin S. Effect of patient position and PEEP on hepatic, portal and central venous pressures during liver resection. Acta Anaesthesiol Scand. 2011;55(9):1106–12.
Zoghbi WA, Enriquez-Sarano M, Foster E, Grayburn PA, Kraft CD, Levine RA, Nihoyannopoulos P, Otto CM, Quinones MA, Rakowski H, Stewart WJ, Waggoner A, Weissman NJ, American Society of E. Recommendations for evaluation of the severity of native valvular regurgitation with two-dimensional and Doppler echocardiography. J Am Soc Echocardiogr. 2003;16(7):777–802.
Dolgin M, New York Heart Association, Criteria Committee. Nomenclature and criteria for diagnosis of diseases of the heart and great vessels. 9th edn. Boston:Little, Brown; 1994.
Levey AS, Eckardt KU, Tsukamoto Y, Levin A, Coresh J, Rossert J, De Zeeuw D, Hostetter TH, Lameire N, Eknoyan G. Definition and classification of chronic kidney disease: a position statement from kidney disease: improving global outcomes (KDIGO). Kidney Int. 2005;67(6):2089–100.
Pestana D, Espinosa E, Eden A, Najera D, Collar L, Aldecoa C, Higuera E, Escribano S, Bystritski D, Pascual J, Fernandez-Garijo P, de Prada B, Muriel A, Pizov R. Perioperative goal-directed hemodynamic optimization using noninvasive cardiac output monitoring in major abdominal surgery: a prospective, randomized, multicenter, pragmatic trial: POEMAS Study (PeriOperative goal-directed thErapy in Major Abdominal Surgery). Anesth Analg. 2014;119(3):579–87.
Salzwedel C, Puig J, Carstens A, Bein B, Molnar Z, Kiss K, Hussain A, Belda J, Kirov MY, Sakka SG, Reuter DA. Perioperative goal-directed hemodynamic therapy based on radial arterial pulse pressure variation and continuous cardiac index trending reduces postoperative complications after major abdominal surgery: a multi-center, prospective, randomized study. Crit Care. 2013;17(5):R191.
Schäberle W (2011) Ultrasonography in vascular diagnosis. vol 2, Second edn. Springer Berlin.
Truong JL, Cyr DP, Lam-McCulloch J, Cleary SP, Karanicolas PJ. Consensus and controversy in hepatic surgery: a survey of Canadian surgeons. J Surg Oncol. 2014;110(8):947–51.
Kato M, Kubota K, Kita J, Shimoda M, Rokkaku K, Sawada T. Effect of infra-hepatic inferior vena cava clamping on bleeding during hepatic dissection: a prospective, randomized, controlled study. World J Surg. 2008;32(6):1082–7. doi:10.1007/s00268-007-9445-0.
Kim YK, Chin JH, Kang SJ, Jun IG, Song JG, Jeong SM, Park JY, Hwang GS. Association between central venous pressure and blood loss during hepatic resection in 984 living donors. Acta Anaesthesiol Scand. 2009;53(5):601–6.
Chhibber A, Dziak J, Kolano J, Norton JR, Lustik S. Anesthesia care for adult live donor hepatectomy: our experiences with 100 cases. Liver Transpl. 2007;13(4):537–42.
Yoneda G, Katagiri S, Yamamoto M. Reverse Trendelenburg position is a safer technique for lowering central venous pressure without decreasing blood pressure than clamping of the inferior vena cava below the liver. J Hepatobiliary Pancreat Sci. 2015;22(6):463–6.
Saner FH, Pavlakovic G, Gu Y, Fruhauf NR, Paul A, Radtke A, Nadalin S, Malago M, Broelsch CE. Does PEEP impair the hepatic outflow in patients following liver transplantation? Intensive Care Med. 2006;32(10):1584–90.
Saner FH, Olde Damink SW, Pavlakovic G, van den Broek MA, Sotiropoulos GC, Radtke A, Nadalin S, Malago M, Paul A. Positive end-expiratory pressure induces liver congestion in living donor liver transplant patients: myth or fact. Transplantation. 2008;85(12):1863–6.
Saner FH, Olde Damink SW, Pavlakovic G, Sotiropoulos GC, Radtke A, Treckmann J, Beckebaum S, Cicinnati V, Paul A. How far can we go with positive end-expiratory pressure (PEEP) in liver transplant patients? J Clin Anesth. 2010;22(2):104–9.
Bredenberg CE, Paskanik AM. Relation of portal hemodynamics to cardiac output during mechanical ventilation with PEEP. Ann Surg. 1983;198(2):218–22.
Brienza N, Revelly JP, Ayuse T, Robotham JL. Effects of PEEP on liver arterial and venous blood flows. Am J Respir Crit Care Med. 1995;152(2):504–10.
Wakabayashi G, Cherqui D, Geller DA, Buell JF, Kaneko H, Han HS, Asbun H, O’Rourke N, Tanabe M, Koffron AJ, Tsung A, Soubrane O, Machado MA, Gayet B, Troisi RI, Pessaux P, Van Dam RM, Scatton O, Abu Hilal M, Belli G, Kwon CH, Edwin B, Choi GH, Aldrighetti LA, Cai X, Cleary S, Chen KH, Schon MR, Sugioka A, Tang CN, Herman P, Pekolj J, Chen XP, Dagher I, Jarnagin W, Yamamoto M, Strong R, Jagannath P, Lo CM, Clavien PA, Kokudo N, Barkun J, Strasberg SM. Recommendations for laparoscopic liver resection: a report from the second international consensus conference held in Morioka. Ann Surg. 2015;261(4):619–29.
Acknowledgements
AU initiated the study, collected data, performed the statistical analysis and wrote the manuscript. AU attests to the integrity of the original data and the analysis reported in this manuscript. SM participated in the design of the study, conducted the study, performed ultrasound measurements, collected data, helped to perform the statistical analysis and drafted and revised the manuscript. SM approved the final manuscript and attests to the integrity of the original data and the analysis reported in this manuscript. GG participated in the design of the study and drafted and revised the manuscript and approved the final manuscript. BO collected data and drafted and revised the manuscript and approved the final manuscript. DB, BN and LF participated in the design of the study and drafted and revised the manuscript. DB, BN and LF approved the final manuscript. CJT, DAR and SAH conceived of the study and participated in its design and coordination, statistical analysis and manuscript drafting and revision. CJT, DAR and SAH approved the final manuscript. CRB conducted the study, collected data, performed the statistical analysis and wrote the manuscript. CRB attests to the integrity of the original data and the analysis reported in this manuscript and is the archival author.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Daniel A. Reuter is a member of the Medical Advisory Board of Pulsion Medical Systems. All other authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
IRB
Ethics Committee of the Medical Board of Hamburg, Weidestraße 122b, 22083 Hamburg, Germany.
Additional information
Asi Ukere and Sebastian Meisner contributed equally to this work.
Rights and permissions
About this article
Cite this article
Ukere, A., Meisner, S., Greiwe, G. et al. The influence of PEEP and positioning on central venous pressure and venous hepatic hemodynamics in patients undergoing liver resection. J Clin Monit Comput 31, 1221–1228 (2017). https://doi.org/10.1007/s10877-016-9970-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-016-9970-1