Abstract
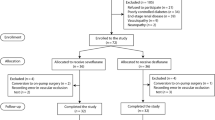
General anesthesia can affect microcirculatory properties. However, differential effects on the microcirculation according to the anesthetic technique used during thoracoscopic surgery have not been well documented. We conducted a randomized clinical trial in which the effects of desflurane and propofol, both with remifentanil, on systemic arterial oxygenation during one-lung ventilation were compared in patients undergoing thoracoscopic surgery. As a subgroup analysis, we compared the effects of two commonly used anesthetic techniques, desflurane–remifentanil (n = 52) and propofol–remifentanil (n = 48), on tissue oxygen saturation using a vascular occlusion test in patients undergoing thoracoscopic surgery. Tissue oxygen saturation was higher in the desflurane than the propofol group (mean ± standard deviation, 83 ± 6 vs. 80 ± 9, 84 ± 6 vs. 76 ± 10, and 87 ± 7 vs. 77 ± 10 % at 30 and 60 min of one-lung ventilation and at two-lung ventilation; adjusted p = 0.026, <0.001, and <0.001, respectively). The recovery slope during the vascular occlusion test, reflecting microvascular reperfusion adequacy, was higher in the desflurane than the propofol group during surgery (mean difference, 0.5 %/s; 95 % CI 0.0–0.9 %/s; p = 0.037). Desflurane–remifentanil anesthesia is associated with better microcirculation than propofol–remifentanil anesthesia in patients undergoing thoracoscopic surgery.




Similar content being viewed by others
References
Kim TK, Cho YJ, Min JJ, Murkin JM, Bahk JH, Hong DM, Jeon Y. Tissue microcirculation measured by vascular occlusion test during anesthesia induction. J Clin Monit Comput. 2016;30:41–50.
Gomez H, Torres A, Polanco P, Kim HK, Zenker S, Puyana JC, Pinsky MR. Use of non-invasive NIRS during a vascular occlusion test to assess dynamic tissue O2 saturation response. Intensive Care Med. 2008;34:1600–7.
Crookes BA, Cohn SM, Bloch S, Amortegui J, Manning R, Li P, Proctor MS, Hallal A, Blackbourne LH, Benjamin R, Soffer D, Habib F, Schulman CI, Duncan R, Proctor KG. Can near-infrared spectroscopy identify the severity of shock in trauma patients? J Trauma. 2005;58:806–16.
Creteur J, Carollo T, Soldati G, Buchele G, De Backer D, Vincent JL. The prognostic value of muscle StO2 in septic patients. Intensive Care Med. 2007;33:1549–56.
Leone M, Blidi S, Antonini F, Meyssignac B, Bordon S, Garcin F, Charvet A, Blasco V, Albanese J, Martin C. Oxygen tissue saturation is lower in nonsurvivors than in survivors after early resuscitation of septic shock. Anesthesiology. 2009;111:366–71.
Payen D, Luengo C, Heyer L, Resche-Rigon M, Kerever S, Damoisel C, Losser MR. Is thenar tissue hemoglobin oxygen saturation in septic shock related to macrohemodynamic variables and outcome? Crit Care. 2009;13(Suppl 5):S6.
Smith RS, Murkin JM. A novel assessment of peripheral tissue microcirculatory vasoreactivity using vascular occlusion testing during cardiopulmonary bypass. J Cardiothorac Vasc Anesth. 2014;28:1217–20.
Putnam B, Bricker S, Fedorka P, Zelada J, Shebrain S, Omari B, Bongard F. The correlation of near-infrared spectroscopy with changes in oxygen delivery in a controlled model of altered perfusion. Am Surg. 2007;73:1017–22.
Shapiro NI, Arnold R, Sherwin R, O’Connor J, Najarro G, Singh S, Lundy D, Nelson T, Trzeciak SW, Jones AE. The association of near-infrared spectroscopy-derived tissue oxygenation measurements with sepsis syndromes, organ dysfunction and mortality in emergency department patients with sepsis. Crit Care. 2011;15:R223.
Ostergaard L, Granfeldt A, Secher N, Tietze A, Iversen NK, Jensen MS, Andersen KK, Nagenthiraja K, Gutierrez-Lizardi P, Mouridsen K, Jespersen SN, Tonnesen EK. Microcirculatory dysfunction and tissue oxygenation in critical illness. Acta Anaesthesiol Scand. 2015;59:1246–59.
Cho YJ, Ryu H, Lee J, Park IK, Kim YT, Lee YH, Lee H, Hong DM, Seo JH, Bahk JH, Jeon Y. A randomised controlled trial comparing incentive spirometry with the Acapella® device for physiotherapy after thoracoscopic lung resection surgery. Anaesthesia. 2014;69:891–8.
Kim SH, Choi YS, Lee JG, Park IH, Oh YJ. Effects of a 1:1 inspiratory to expiratory ratio on respiratory mechanics and oxygenation during one-lung ventilation in the lateral decubitus position. Anaesth Intensive Care. 2012;40:1016–22.
De Backer D, Donadello K, Cortes DO. Monitoring the microcirculation. J Clin Monit Comput. 2012;26:361–6.
Ekbal NJ, Dyson A, Black C, Singer M. Monitoring tissue perfusion, oxygenation, and metabolism in critically ill patients. Chest. 2013;143:1799–808.
Tripodaki ES, Tasoulis A, Koliopoulou A, Vasileiadis I, Vastardis L, Giannis G, Argiriou M, Charitos C, Nanas S. Microcirculation and macrocirculation in cardiac surgical patients. Crit Care Res Pract. 2012;2012:654381.
Abdelmalak BB, Cata JP, Bonilla A, You J, Kopyeva T, Vogel JD, Campbell S, Sessler DI. Intraoperative tissue oxygenation and postoperative outcomes after major non-cardiac surgery: an observational study. Br J Anaesth. 2013;110:241–9.
Holmstrom A, Akeson J. Desflurane induces more cerebral vasodilation than isoflurane at the same A-line autoregressive index level. Acta Anaesthesiol Scand. 2005;49:754–8.
Sundeman H, Biber B, Martner J, Raner C, Winso O. Vasodilator effects of desflurane and isoflurane in the feline small intestine. Acta Anaesthesiol Scand. 1995;39:1105–10.
Weiskopf RB, Holmes MA, Eger EI 2nd, Johnson BH, Rampil IJ, Brown JG. Cardiovascular effects of I653 in swine. Anesthesiology. 1988;69:303–9.
Weiskopf RB, Cahalan MK, Eger EI 2nd, Yasuda N, Rampil IJ, Ionescu P, Lockhart SH, Johnson BH, Freire B, Kelley S. Cardiovascular actions of desflurane in normocarbic volunteers. Anesth Analg. 1991;73:143–56.
Hartman JC, Pagel PS, Proctor LT, Kampine JP, Schmeling WT, Warltier DC. Influence of desflurane, isoflurane and halothane on regional tissue perfusion in dogs. Can J Anaesth. 1992;39:877–87.
De Blasi RA, Palmisani S, Alampi D, Mercieri M, Romano R, Collini S, Pinto G. Microvascular dysfunction and skeletal muscle oxygenation assessed by phase-modulation near-infrared spectroscopy in patients with septic shock. Intensive Care Med. 2005;31:1661–8.
Koopmans M, Kuiper MA, Endeman H, Veenstra G, Vellinga NA, de Vos R, Boerma EC. Microcirculatory perfusion and vascular reactivity are altered in post cardiac arrest patients, irrespective of target temperature management to 33°C vs 36°C. Resuscitation. 2015;86:14–8.
Kim TK, Cho YJ, Min JJ, Murkin JM, Bahk JH, Hong DM, Jeon Y. Microvascular reactivity and clinical outcomes in cardiac surgery. Crit Care. 2015;19:316.
Lima A. Current status of tissue monitoring in the management of shock. Curr Opin Crit. 2016;22(3):274–8.
Cohn SM, Nathens AB, Moore FA, Rhee P, Puyana JC, Moore EE, Beilman GJ, StO2 in Trauma Patients Trial Investigators (2007) Tissue oxygen saturation predicts the development of organ dysfunction during traumatic shock resuscitation. J Trauma 62:44–55.
Park GR, Evans TN, Hutchins J, Borissov B, Gunning KE, Klinck JR. Reducing the demand for admission to intensive care after major abdominal surgery by a change in anaesthetic practice and the use of remifentanil. Eur J Anaesthesiol. 2000;17:111–9.
Albertin A, Dedola E, Bergonzi PC, Lombardo F, Fusco T, Torri G. The effect of adding two target-controlled concentrations (1–3 ng mL−1) of remifentanil on MAC BAR of desflurane. Eur J Anaesthesiol. 2006;23:510–6.
Ryu CG, Min SW, Kim J, Han SH, Do SH, Kim CS. Effect of remifentanil on arterial oxygenation during one-lung ventilation. J Int Med Res. 2010;38:1749–58.
Bruder EA, Ball IM, Ridi S, Pickett W, Hohl C. Single induction dose of etomidate versus other induction agents for endotracheal intubation in critically ill patients. Cochrane Database Syst Rev. 2015;1:CD010225.
Peeters B, Guiza F, Boonen E, Meersseman P, Langouche L, Van den Berghe G. Drug-induced HPA axis alterations during acute critical illness: a multivariable association study. Clin Endocrinol (Oxf). 2016. doi:10.1111/cen.13155.
Acknowledgments
The authors thank the Medical Research Collaborating Center for their advice concerning the statistical analyses.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The contents of this study have not been published elsewhere nor are being submitted elsewhere. The manuscript has been read and approved by all co-authors. Hippo Medical Company (Seoul, Korea) and Hutchinson (MN, USA) provided the Inspectra™ StO2 tissue oxygenation monitor during this study. Dr. Jeon received grant support from Ilsung Pharmaceuticals (research grant for studies). The remaining authors have disclosed that they do not have any potential conflicts of interest including commercial relationships such as consultation and equity interests.
Ethical approval
All procedures performed in the study involving human participates were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Cho, Y.J., Bae, J., Kim, T.K. et al. Microcirculation measured by vascular occlusion test during desflurane–remifentanil anesthesia is superior to that in propofol–remifentanil anesthesia in patients undergoing thoracic surgery: subgroup analysis of a prospective randomized study. J Clin Monit Comput 31, 989–997 (2017). https://doi.org/10.1007/s10877-016-9937-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-016-9937-2