Abstract
Purpose
Inflammation is implicated in cardiovascular disease (CVD), but the association of total serum immunoglobulin (Ig) A, G, and M with CVD across the whole spectrum of atherosclerosis in community-dwelling elderly is unknown.
Methods
This study was embedded in the Rotterdam Study, an ongoing population-based cohort study. We performed Cox regression for the associations of Igs with incident atherosclerotic CVD (ACVD; composite of myocardial infarction, revascularization, and stroke), cardiovascular mortality, and all-cause mortality, and multinomial logistic regression for the association between Igs and coronary artery calcification (CAC) scores. We adjusted for age, sex, lifestyle, and cardiovascular risk factors and presented results per standard deviation increase.
Results
We included 8767 participants (median age 62.2 years, 57% women). Higher IgG was associated with an increased ACVD risk (hazard ratio [HR]: 1.08; 95% confidence interval [95% CI]: 1.01–1.15). Higher IgA and IgG were associated with an increased cardiovascular mortality risk, mainly within Ig reference ranges, and with an increased all-cause mortality risk, although less marked. Higher IgA was associated with severe atherosclerosis, i.e., CAC score > 400 (odds ratio: 1.29; 95% CI: 1.03–1.62), while for higher IgG a trend was seen with severe atherosclerosis.
Conclusion
In middle-aged and older individuals from the general population, higher serum IgA and IgG, but not IgM, are associated with CVD, cardiovascular mortality, and severe atherosclerosis, particularly within Ig reference ranges and independent of serum C-reactive protein. Future studies are needed to elucidate potential causality of the reported associations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cardiovascular disease (CVD) is the main cause of disability and mortality worldwide with atherosclerosis as the most common underlying pathology [1, 2]. The etiology of atherosclerosis is complex but involves several metabolic and inflammatory factors [2, 3]. Coronary artery calcification (CAC), considered an early manifestation of atherosclerosis, is positively correlated with the extent of atherosclerosis and related to inflammation as well [4]. Recently, several components of the immune system have been targeted in an attempt to reduce inflammation leading to atherosclerosis with anti-interleukin-1 (IL-1) and anti-interleukin-6 (IL-6) targeted therapy showing promising results [5, 6].
In contrast, the contribution of immunoglobulins (Igs) to atherosclerosis has been relatively understudied [2, 3]. In mouse models, a decreased number of B2-cells due to B-cell activating factor receptor deficiency, resulting in diminished levels of IgG1, IgG2a, and IgM, was associated with less atherosclerosis [7]. However, reviews of studies mainly performed in rodents reported inconclusive results on the effects of serum Igs depending on the type of Ig. IgA and IgG may generally have a stimulating effect on atherosclerosis, e.g., via reaction with atherothrombotic or oxidation-specific epitopes, whereas IgM may be predominantly protective through neutralization of atherosclerotic antigens [8, 9].
Reviews of studies in humans reported various IgA and IgG auto-antibodies that were mostly associated with an increased risk of CVD, whereas results were inconclusive for the association between IgM auto-antibodies and CVD risk [10, 11]. Pathogen-specific antibodies have been related to CVD as well and over the years multiple trials were performed to assess the efficacy of antibiotic treatment in the prevention of CVD and cardiovascular mortality, but utility could not be demonstrated [12, 13]. However, studies on the association between total serum levels of Igs and CVD are sparse and show inconclusive results, while total serum Ig measurements are readily available in clinical practice and may provide a broader overview of the immune system status in the context of atherosclerosis. Two studies showed a relation between higher Ig levels and CVD [14, 15], while two other studies reported a relation between higher Ig levels and a lower risk of CVD or less severe cardiovascular outcomes [16, 17]. However, these studies were either cross-sectional or did not include time-to-event analyses, did not adjust for potential confounders including cardiovascular risk factors, or categorized serum Ig levels resulting in loss of information. One longitudinal population-based study failed to show an association between Igs and CVD, which could be due to being underpowered with a total of 47 nonfatal and 10 fatal ischemic events. Furthermore, the study was set in a different cardiovascular risk management era, with blood drawn in 1984 and four years of follow-up [18]. Due to the design of these previous studies, reverse causation cannot be ruled out. Furthermore, most studies were patient-based with mainly or exclusively male participants, thus limiting generalizability of results, and none of the studies investigated the association of Igs with subclinical atherosclerosis.
We performed the current study to address abovementioned limitations of previous studies in order to shed more light on the relation between Igs and the whole spectrum of atherosclerosis in individuals from the general population. To this end, we studied the association of serum Igs with atherosclerotic CVD (ACVD; composite of myocardial infarction, revascularization, and stroke), cardiovascular (both atherosclerotic and non-atherosclerotic) mortality, and CAC scores in a population-based cohort of middle-aged and older individuals with over 17 years of follow-up. We adjusted for serum C-reactive protein (CRP) to establish whether the association of serum Igs with cardiovascular outcomes is independent of currently known inflammatory pathways including CRP and ILs. Furthermore, we assessed the association between serum Igs and all-cause mortality to investigate potential differences that may proxy the relation of Igs with cardiovascular compared to systemic inflammation.
Methods
Study Design and Participants
This study was embedded in the Rotterdam Study (RS), an ongoing prospective population-based cohort study including middle-aged and older inhabitants of Ommoord, Rotterdam, the Netherlands. The RS started in 1990 and included interested inhabitants of the study area that were aged 55 years or over. The RS was extended with additional independent cohorts in 2000 and 2006 and for these cohorts, inhabitants aged 55 years or over (RS cohort II) respectively 45 years or over (RS cohort III) that were not previously invited were invited to participate. By the end of 2008, 14,926 participants aged 45 years or over had been enrolled (response rate 72%). In 2016, enrollment for a fourth cohort started aimed at inhabitants of the study area aged 40 years or over. After study entry, medical records of general practitioners (GPs) are continuously linked to the RS database and outcomes of interest are validated according to standardized guidelines by medical experts in the field. In addition, each participant is re-examined every three to six years at the research center in Ommoord and through home interviews. The RS complies with the declaration of Helsinki and has been approved by the medical ethics committee of the Erasmus University Medical Center (registration number MEC 02.1015) and by the Dutch Ministry of Health, Welfare and Sport (Population Screening Act WBO, license number 1071272–159,521-PG). The RS has been entered into the Netherlands National Trial Register and into the WHO International Clinical Trials Registry Platform under shared catalogue number NTR6831. More detailed information can be found elsewhere [19].
For this study, we included participants of three independent RS cohorts (RS I-3, II-1, and III-1) with written informed consent for follow-up, available measurements of serum IgA, IgG, and/or IgM at study baseline, and information on cardiovascular outcomes of interest (n = 8767).
Assessment of Serum Igs
Blood was drawn at the research center through 1997–1999 (RS cohort I-3), 2000–2001 (RS cohort II-1), and 2006–2008 (RS cohort III-1) and the moment of blood drawing was considered the study baseline. Serum samples were subsequently stored at − 80 °C. Serum IgA, IgG, and IgM measurements took place between 2016 and 2018 through an immunoturbidimetric assay (Tina-quant® IgA/IgG/IgM Gen. 2, Roche Diagnostics GmbH, Mannheim, Germany). Recommended reference ranges according to the manufacturer’s protocol were 0.7–4.0 g/L for IgA, 7.0–16.0 g/L for IgG, and 0.4–2.3 g/L for IgM. As previously described, reference ranges based on 2.5th and 97.5th percentiles for the RS population were 0.86–4.76 g/L for IgA, 6.20–15.10 g/L for IgG, and 0.28–2.64 g/L for IgM [20].
Assessment of ACVD, Cardiovascular and All-Cause Mortality, and CAC
ACVD was defined as myocardial infarction, revascularization (percutaneous coronary intervention or coronary artery bypass graft), or stroke in accordance with previous research and specific guidelines [21]. Information on prevalent (at baseline) ACVD was retrieved through home interviews, linkage with the Nationwide Medical Registry (a national registry of all hospital discharge diagnoses of all Dutch inhabitants), and medical records of GPs. Information on incident (during follow-up) ACVD was retrieved through continuous automated linkage with medical records of GPs containing ICPC codes as diagnosed by GPs or medical specialists and was subsequently validated as described previously [22,23,24]. Follow-up of myocardial infarction, revascularization, and the composite endpoint of ACVD was complete until January 1, 2015. Follow-up of stroke (comprising all stroke cases, i.e., ischemic, hemorrhagic, and unspecified) was complete until January 1, 2016.
Information on mortality was retrieved from medical records of GPs, hospitals, and nursing homes. Two independent research physicians classified mortality according to ICPC and ICD-10 codes. Subsequently, all coded events were reviewed by a senior physician in the field to confirm the diagnosis. Date of death was retrieved from the medical records or municipality records. Cardiovascular mortality was composed of atherosclerotic and non-atherosclerotic mortality. Atherosclerotic mortality was defined as mortality due to coronary heart disease, cerebrovascular disease, or other atherosclerotic disease (ICPC codes K75-K77, K90-K92; ICD-10 codes I21-I25, I50, I60-I70, I71.3, I71.4, I73-I74, I77-I79, Y60.5) and non-atherosclerotic mortality was defined as mortality due to other cardiovascular disease (ICPC codes K78-K87, K93-K94, K99; ICD-10 codes I05-I13, I15, I26-I28, I30-I49, I51-I52, I71[excluding I71.3 and I71.4]-I72, I80-I83, I97-I99, T82) in accordance with previous literature [22]. Follow-up of cardiovascular mortality was complete until January 1st 2015. All-cause mortality comprised any (both cardiac and non-cardiac) mortality and its follow-up was complete until May 24, 2018.
CAC scores were available in a random subset of RS cohorts I-3 and II-1 (n = 1622) and were measured by electronbeam computed tomography (EBT; C-150 Imatron Scanner, GE Healthcase, South San Francisco, CA). Participants had to lie still and hold their breath during the assessment. Thirty-eight images were obtained from the aorta root to the heart with 100-ms scan time and 3-mm slice thickness. CAC was quantified with AccuImage software (AccuImage Diagnostics Corp), displaying all pixels with a density of > 130 Hounsfield units (HU). Calcification was defined as ≥ 2 adjacent pixels of > 130 HU. CAC scores were calculated by multiplication of the area of individual calcifications in mm2 with a factor based on the peak density of the calcification. All individual CAC scores were combined to obtain a total CAC score for the entire coronary epicardial system. Assessment of CAC was performed by two independent experienced physicians [25].
Assessment of Baseline Covariates
Weight, height, and blood pressure were measured at the research center in Ommoord. Body mass index (BMI) was defined as weight divided by height squared (kg/m2). Blood pressure was measured twice at the right brachial artery with the participant in sitting position. The average of these two consecutive measurements was taken. Hypertension was defined as a blood pressure exceeding 140/90 mmHg or as the use of blood pressure lowering medication with the indication of hypertension. Information on baseline type 2 diabetes (DM) was collected from GPs and pharmacies and assessed through blood samples collected at the research center. DM was defined as a fasting blood glucose concentration of ≥ 7.0 mmol/L, a non-fasting blood glucose concentration of ≥ 11.1 mmol/L (when fasting samples were unavailable), or as the use of blood glucose-lowering drugs or dietary treatment for diabetes. Smoking status, alcohol consumption, and highest attained education (as proxy for socioeconomic status) were assessed through questionnaires during home interviews. Smoking status was defined as never, former, or current smoker. Alcohol consumption was reported in gram/day and categorized into none, mild (0–10 g/day), moderate (10–20 g/day), or heavy (> 20 g/day). Physical activity was assessed using validated questionnaires and expressed in standardized metabolic equivalent of task (MET) hours/week [26, 27]. Serum triglycerides and total cholesterol (mmol/L) were measured using an automated enzymatic procedure. Serum CRP (mg/L) was measured with an immunoturbidimetric assay. Baseline use of medication known to potentially alter serum Ig levels (systemic corticosteroids, antiepileptic drugs, angiotensin converting enzyme inhibitors, cytostatics, immunomodulators, and/or immunosuppressants) was established during home interviews and coded based on the Anatomical Therapeutic Chemical Classification System. None of the participants used intravenous or subcutaneous Igs.
Statistical Analyses
Serum Igs were standardized for all analyses to facilitate comparison of results. In the longitudinal analyses, participants were followed until the first event of interest, death, or end of follow-up, whichever came first. All analyses included three models, adjusting for potential confounders based on biological plausibility and previous comparable research [21]. In the first model, we adjusted for age and sex. In the second model, we additionally adjusted for smoking status, alcohol consumption, physical activity, and highest attained education. The third model included confounders that could also act as mediators and comprised BMI, DM, hypertension, serum triglycerides, CRP, and total serum cholesterol additional to the first two models. The longitudinal analyses also included RS cohort in all models to take temporal trends into account.
The association between serum Igs and incident ACVD (both composite and the individual endpoints of myocardial infarction, revascularization, and stroke) was assessed through Cox proportional hazards regression analyses after exclusion of participants with prevalent ACVD. The proportional hazards assumption was checked through the Schoenfeld test and plot and was met for all analyses. A sensitivity analysis was performed by excluding participants with serum Ig levels outside our calculated reference ranges (0.86–4.76 g/L for IgA, 6.20–15.10 g/L for IgG, and 0.28–2.64 g/L for IgM) and users of medication known to potentially alter serum Ig levels in order to limit the influence of transient outliers in serum Ig levels. With respect to stroke, we also examined the association of Igs with ischemic stroke.
The association of serum Igs with cardiovascular mortality (atherosclerotic, non-atherosclerotic, and combined) and all-cause mortality was assessed by Cox proportional hazards regression analyses. Proportional hazards were checked and confirmed for all analyses. For cardiovascular mortality, we stratified by prevalent ACVD status, age (cut-off 65 years), and sex, and performed a sensitivity analysis after exclusion of participants with serum Ig levels outside the reference range and users of medication known to potentially alter serum Ig levels. For comparison, we applied both the assay recommended and our own calculated reference ranges in this sensitivity analysis. We furthermore displayed the risk of cardiovascular mortality for participants with the highest compared to the lowest Ig reference value (4.76 vs 0.86 g/L for IgA, 15.10 vs 6.20 g/L for IgG, and 2.64 vs 0.28 g/L for IgM) while keeping all other covariates constant by testing contrasts of the Cox proportional hazards regression analyses.
For the association between serum Igs and CAC score, we categorized CAC scores into no (score = 0), mild (score 0–100), moderate (score 100–400), or severe calcification (score > 400) based on the most commonly used classification system [28]. The association between serum Igs and CAC score categories was assessed through multinomial logistic regression analyses, while taking no calcification as the reference category. There was no multicollinearity and the linearity of log odds assumption was met. We performed a sensitivity analysis by excluding participants with serum Ig levels outside abovementioned calculated reference ranges and users of medication known to potentially alter serum Ig levels.
Missing values in covariates were imputed with multivariate imputation by chained Eqs. (4 imputations, 10 iterations). Missingness was < 2% for all covariates, except for physical activity and alcohol consumption (14.1% and 20.4% respectively). Convergence was reached and the distribution of covariates before and after imputation was similar. All analyses were performed with R Statistical Software version 4.0.2. Provided that effect estimates of the second and third models were comparable, we described the fully adjusted models in the results, unless stated otherwise.
Results
We included 8,767 participants with a median age of 62.2 years and of whom 57% were women. Median values of IgA, IgG, and IgM were 2.10, 9.70, and 0.85 g/L respectively. Standard deviations (SDs) were 1.06 for IgA, 2.39 for IgG, and 0.98 for IgM. At baseline, 822 (9.4%) participants had prevalent ACVD. Baseline characteristics are displayed in Table 1. In participants without prevalent ACVD, 1020 incident ACVD events occurred during a median follow-up of 8.3 years (interquartile range [IQR]: 6.8–14.0), with an incidence rate of 13.4 per 1000 person-years. A total of 655 events occurred of cardiovascular mortality (median follow-up 8.6 years; IQR: 7.0–14.2) and 2,992 events of all-cause mortality (median follow-up 10.0 years; IQR: 7.7–15.4). Completeness of follow-up for cardiovascular mortality was 99.2% [29].
Association Between Serum Igs and Incident ACVD
IgA was not associated with the composite outcome of incident ACVD or with myocardial infarction, revascularization, or stroke separately (Table 2). Higher IgG was associated with a modestly increased risk of ACVD (hazard ratio [HR] per SD: 1.08; 95% confidence interval [95% CI]: 1.01–1.15) and this was driven by an increased risk of myocardial infarction and revascularization. IgM was not associated with incident ACVD (Table 2).
Effect estimates did not materially change after exclusion of participants with Ig levels outside the reference range and users of potentially Ig-altering medication (Supplementary Table S1). Effect estimates for the association of serum Igs with ischemic stroke were comparable to those with all stroke (Supplementary Table S2).
Association Between Serum Igs and Cardiovascular and All-Cause Mortality
Higher IgA was associated with an increased risk of all cardiovascular (HR: 1.13 per SD; 95% CI: 1.06–1.21) and atherosclerotic cardiovascular mortality (HR: 1.14 per SD; 95% CI: 1.05–1.23). The association between higher IgA and non-atherosclerotic cardiovascular mortality did not reach statistical significance (HR per SD: 1.11; 95% CI: 0.98–1.25) (Table 3). Higher IgG was associated with all cardiovascular (HR: 1.14 per SD; 95% CI: 1.07–1.22), atherosclerotic (HR: 1.12 per SD; 95% CI: 1.04–1.22), and non-atherosclerotic cardiovascular mortality (HR: 1.19 per SD; 95% CI: 1.05–1.34). IgM was not associated with cardiovascular mortality risk (Table 3).
Effect sizes for higher IgA and IgG increased after exclusion of participants with Ig levels outside the reference range and users of potentially Ig-altering medication (Table 3). Results after exclusion of participants with Ig levels outside assay recommended reference ranges were comparable to results after exclusion of participants with Ig levels outside our calculated reference ranges (Table 3, Supplementary Table S3).
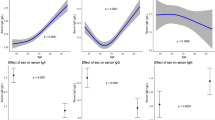
Participants with highest vs lowest reference value of IgA, and similar values for all other covariates, had higher risks of all cardiovascular (HR: 1.58; 95% CI: 1.23–2.02) and atherosclerotic cardiovascular mortality (HR: 1.63; 95% CI: 1.22–2.19). Similar results were retrieved for the associations of highest vs lowest reference IgG value with the risk of all cardiovascular (HR: 1.65; 95% CI: 1.28–2.11) and atherosclerotic cardiovascular mortality (HR: 1.55; 95% CI: 1.15–2.09) (Fig. 1, Supplementary Table S4). In addition, the highest vs lowest reference value of IgG was associated with an almost twofold increased risk of non-atherosclerotic cardiovascular mortality (Fig. 1, Supplementary Table S4).
Association between highest compared to lowest reference immunoglobulin levels and risk of cardiovascular mortality. Depicted are HRs (colored dots) and 95% CIs (colored horizontal lines) for the association of highest compared to lowest reference value of serum IgA (4.76 vs 0.86 g/L), IgG (15.10 vs 6.20 g/L), and IgM (2.64 vs 0.28 g/L) with different types of cardiovascular mortality. HRs are adjusted for age, sex, Rotterdam Study cohort, smoking status, alcohol consumption, physical activity, and highest attained education. 95% CI, 95% confidence interval; HR, hazard ratio; IgA/IgG/IgM, immunoglobulin A/G/M
In general, effect estimates for the associations between serum Igs and all cardiovascular and atherosclerotic cardiovascular mortality were comparable when stratified by age, sex, or prevalent ACVD status. However, for non-atherosclerotic mortality we reported stronger associations in women than men for higher IgA (HR: 1.24 vs 1.01 per SD) and IgG (HR: 1.25 vs 1.09 per SD). Furthermore, we found stronger associations with non-atherosclerotic mortality in participants ≤ 65 compared to > 65 years for higher IgA (HR: 1.34 vs 1.08 per SD) and IgG (HR: 1.55 vs 1.19 per SD) and in participants without compared to with prevalent ACVD (HR for IgA: 1.18 vs 0.91 per SD; HR for IgG: 1.28 vs 1.09 per SD) (Supplementary Table S5).
Higher IgA was associated with an increased risk of all-cause mortality (HR: 1.09 per SD; 95% CI: 1.05–1.12), as was higher IgG (HR: 1.06 per SD; 95% CI: 1.03–1.10). IgM was not associated with all-cause mortality risk (Supplementary Table S6).
Association Between Serum Igs and CAC
Higher IgA was associated with severe CAC (odds ratio [OR] per SD: 1.29; 95% CI: 1.03–1.62) (Table 4). Higher IgG was also associated with severe CAC, although not statistically significantly (OR per SD: 1.16; 95% CI: 0.95–1.43). IgM was not associated with CAC score (Table 4).
After exclusion of participants with IgG levels outside the reference range and users of potentially Ig-altering medication, the association of higher IgG with severe CAC was more pronounced (OR per SD: 1.36; 95% CI: 1.00–1.84) (Supplementary Table S7).
Discussion
In this study, we report that higher serum IgA and IgG levels were associated with an increased risk of all cardiovascular, atherosclerotic, and non-atherosclerotic cardiovascular mortality. Higher serum IgG levels were furthermore associated with an increased risk of ACVD. The reported associations with ACVD and cardiovascular mortality were supported by the association of higher IgA and trend of higher IgG with severe atherosclerosis. Higher serum IgA and IgG were associated with an increased risk of all-cause mortality as well, although less pronounced. Serum IgM was not associated with any of the outcomes. Our reported associations were independent of CRP, which has indirectly been targeted in anti-IL-1 and anti-IL-6 therapy, since these ILs can promote CRP production [30]. This may imply involvement of serum Igs in novel inflammatory processes that could potentially be targeted in patients with a high residual risk of CVD, although more research is needed to investigate this.
Previously, Igs have been detected in the intima of human atherosclerotic plaques [9]. We believe that our results may underline a potential direct effect of Igs on atherosclerosis, ACVD and cardiovascular mortality by binding to atherosclerotic antigens or particles. Vascular calcification, including CAC, is strongly driven by inflammation [31, 32]. Calcifying nanoparticles are thought to play a causal role in vascular calcification, potentially by promoting endothelial dysfunction and downregulation of atheroprotective transcription factors among others [33, 34]. Higher IgG levels directed against calcifying nanoparticles were demonstrated in Turkish individuals with CAC and these IgG levels correlated positively with CAC score [33]. It has been implicated that IgG bound to calcifying nanoparticles can promote further calcification, thus resulting in a vicious loop of inflammation and calcification [35]. Igs may induce or promote atherosclerosis by binding to atherosclerotic antigens as well [8]. Anti-β2-glycoprotein 1 IgA and IgG antibodies have been reported in patients with atherosclerosis and play an important role in atherogenesis, as they facilitate uptake of oxidized low-density lipoprotein by macrophages [36,37,38]. Antigen-bound IgG can furthermore activate macrophages via Fc receptors and promote foam cell formation, thus inducing plaque formation [39, 40]. Apolipoprotein A1-bound IgG may also inhibit the function of high-density lipoprotein cholesterol [40]. Previously, higher serum IgA levels have been reported in patients with atherosclerosis compared to controls [41]. More recently, IgA antibodies against phosphocholine and Streptococcus pneumoniae cell wall polysaccharide were found to be associated with an increased CVD risk, suggesting a potential pathway via gut microbiota and phospholipid synthesis [42]. Igs directed to other pathogens, including Chlamydia pneumoniae and Helicobacter pylori have been related with atherosclerosis and CVD as well [43, 44]. Possible mechanisms include vascular inflammation due to molecular mimicry or endotoxin-induced increased uptake of lipids by macrophages [44].
The reported associations of serum Igs with ACVD and cardiovascular mortality could partly be explained by underlying atherosclerosis. Higher CAC scores have previously been associated with an increased risk of coronary heart disease, stroke, cardiovascular mortality, cancer related mortality, and all-cause mortality [45, 46]. Interestingly, within the composite outcome of ACVD, we only reported a trend of higher IgG with myocardial infarction and revascularization. HRs for the association with both total and ischemic stroke were around 1, suggesting that the cerebrovascular system is less susceptible for the effects of serum Igs, which may have to do with shielding by the blood brain barrier [47]. However, we also showed an association between higher IgG and non-atherosclerotic cardiovascular mortality, implying that serum Igs are involved in cardiovascular inflammation that bypasses atherosclerosis. A recent Japanese study concluded that Ig free light chain levels were significantly higher in patients with atrial fibrillation, heart failure with sinus rhythm, and hypertrophic cardiomyopathy compared to healthy controls [48]. This suggests that serum Igs may be associated with cardiac disease through pathways other than atherosclerosis as well, future studies should investigate this.
Interestingly, the majority of the associations with cardiovascular mortality were enhanced within the reference range. It is possible that spikes in serum Ig levels are temporary and that chronic low-grade elevated Ig levels on the other hand are clinically relevant with respect to cardiovascular (and potentially other inflammatory) outcomes, as is seen with high-sensitivity CRP levels [49]. Furthermore, participants with reference range Ig levels and without use of potentially Ig-altering medication may have more stable serum Ig levels over time, thus being less likely to suffer from regression towards the mean. We also consistently reported stronger and significant associations of higher IgA and IgG with cardiovascular mortality in participants without baseline ACVD. This may imply that serum Igs could be directly associated with cardiovascular mortality, independent of pre-existing atherosclerosis and ACVD. Furthermore, it may argue against reverse causation (i.e., pre-existing atherosclerotic disease influencing serum Ig levels).
Lastly, we reported associations of higher IgA and IgG levels with all-cause mortality. This is line with the results of a previous population-based study in military men [50]. However, effect estimates for all-cause mortality were smaller than those for cardiovascular mortality, underlining the potentially more prominent contribution of serum Igs to cardiovascular inflammation.
Important strengths or our study include the population-based design with a balanced distribution of men and women, long follow-up with negligible loss to follow-up, and ascertainment of cardiovascular outcomes based on internationally applied clinical criteria and guidelines. We also possessed a wide range of meticulously measured potential confounders. However, our study also knows some limitations. Despite comprehensive adjustment, as with all observational studies, residual confounding cannot be ruled out. We only had serum Ig measurements at baseline, and were therefore unable to associate changes in Ig levels over time with risk of ACVD and mortality. Furthermore, the RS consists of a mainly Caucasian population, possibly limiting extrapolation of our results to other populations. Future studies are warranted to replicate our findings in other populations and to elucidate the underlying pathophysiological pathways and mechanisms. If causality is demonstrated, these pathophysiological processes may be investigated as modifiable treatment target in patients with a residual inflammatory CVD risk. Independent of a causal relationship, applicability of serum Igs as cardiovascular biomarker should be assessed.
Conclusions
In middle-aged and older individuals from the general population, higher serum IgA and IgG, but not serum IgM, are associated with an increased risk of ACVD, cardiovascular mortality, and severe atherosclerosis. Although we hypothesize a potential causal relationship between serum Igs and cardiovascular morbidity and mortality, future studies are needed to confirm this. Alternatively, utility of serum Igs as biomarker in cardiovascular risk management should be assessed.
Data Availability
Data can be obtained upon request. Requests should be directed towards the management team of the Rotterdam Study (datamanagement.ergo@erasmusmc.nl), which has a protocol for approving data requests. Because of restrictions based on privacy regulations and informed consent of the participants, data cannot be made freely available in a public repository.
References
Joseph P, Leong D, McKee M, Anand SS, Schwalm JD, Teo K, et al. Reducing the global burden of cardiovascular disease, Part 1: The Epidemiology and Risk Factors. Circ Res. 2017;121(6):677–94.
Schaftenaar F, Frodermann V, Kuiper J, Lutgens E. Atherosclerosis: the interplay between lipids and immune cells. Curr Opin Lipidol. 2016;27(3):209–15.
Hansson GK, Hermansson A. The immune system in atherosclerosis. Nat Immunol. 2011;12(3):204–12.
Li JJ, Zhu CG, Yu B, Liu YX, Yu MY. The role of inflammation in coronary artery calcification. Ageing Res Rev. 2007;6(4):263–70.
Ridker PM, Everett BM, Thuren T, MacFadyen JG, Chang WH, Ballantyne C, et al. Antiinflammatory therapy with canakinumab for atherosclerotic disease. N Engl J Med. 2017;377(12):1119–31.
Anstensrud AK, Woxholt S, Sharma K, Broch K, Bendz B, Aakhus S, et al. Rationale for the ASSAIL-MI-trial: a randomised controlled trial designed to assess the effect of tocilizumab on myocardial salvage in patients with acute ST-elevation myocardial infarction (STEMI). Open Heart. 2019;6(2):e001108.
Kyaw T, Tay C, Hosseini H, Kanellakis P, Gadowski T, MacKay F, et al. Depletion of B2 but not B1a B cells in BAFF receptor-deficient ApoE mice attenuates atherosclerosis by potently ameliorating arterial inflammation. PLoS One. 2012;7(1):e29371.
Chistiakov DA, Orekhov AN, Bobryshev YV. Immune-inflammatory responses in atherosclerosis: Role of an adaptive immunity mainly driven by T and B cells. Immunobiol. 2016;221(9):1014–33.
Porsch F, Mallat Z, Binder CJ. Humoral immunity in atherosclerosis and myocardial infarction: from B cells to antibodies. Cardiovasc Res. 2021;117(13):2544–62.
Roux-Lombard P, Pagano S, Montecucco F, Satta N, Vuilleumier N. Auto-antibodies as emergent prognostic markers and possible mediators of ischemic cardiovascular diseases. Clin Rev Allergy Immunol. 2013;44(1):84–97.
Iseme RA, McEvoy M, Kelly B, Agnew L, Walker FR, Handley T, et al. A role for autoantibodies in atherogenesis. Cardiovasc Res. 2017;113(10):1102–12.
Wells BJ, Mainous AG 3rd, Dickerson LM. Antibiotics for the secondary prevention of ischemic heart disease: a meta-analysis of randomized controlled trials. Arch Intern Med. 2004;164(19):2156–61.
Sethi NJ, Safi S, Korang SK, Hrobjartsson A, Skoog M, Gluud C, et al. Antibiotics for secondary prevention of coronary heart disease. Cochrane Database Syst Rev. 2021;2:CD003610.
Czlonkowska A, Cyrta B, Korlak J. Immunological observations on patients with acute cerebral vascular disease. J Neurol Sci. 1979;43(3):455–64.
Kovanen PT, Manttari M, Palosuo T, Manninen V, Aho K. Prediction of myocardial infarction in dyslipidemic men by elevated levels of immunoglobulin classes A, E, and G, but not M. Arch Intern Med. 1998;158(13):1434–9.
Koltowski L, Filipiak KJ, Rdzanek A, Stepien V, Tarchalska-Krynska B, Opolski G. IgG, IgM and inflammatory markers serum concentration in patients with acute coronary syndrome: a pilot study. Kardiol Pol. 2012;70(10):1023–8.
Khamis RY, Hughes AD, Caga-Anan M, Chang CL, Boyle JJ, Kojima C, et al. High serum immunoglobulin g and m levels predict freedom from adverse cardiovascular events in Hypertension: a nested case-control substudy of the Anglo-Scandinavian cardiac outcomes trial. EBioMedicine. 2016;9:372–80.
Muscari A, Bozzoli C, Puddu GM, Sangiorgi Z, Dormi A, Rovinetti C, et al. Association of serum C3 levels with the risk of myocardial infarction. Am J Med. 1995;98(4):357–64.
Ikram MA, Brusselle G, Ghanbari M, Goedegebure A, Ikram MK, Kavousi M, et al. Objectives, design and main findings until 2020 from the Rotterdam Study. Eur J Epidemiol. 2020;35(5):483–517.
Khan SR, Chaker L, Ikram MA, Peeters RP, van Hagen PM, Dalm V. Determinants and reference ranges of serum immunoglobulins in middle-aged and elderly individuals: a population-based study. J Clin Immunol. 2021;(41):1902–14. https://doi.org/10.1007/s10875-021-01120-5.
Bano A, Chaker L, Mattace-Raso FUS, van der Lugt A, Ikram MA, Franco OH, et al. Thyroid function and the risk of atherosclerotic cardiovascular morbidity and mortality: the rotterdam study. Circ Res. 2017;121(12):1392–400.
Leening MJ, Kavousi M, Heeringa J, van Rooij FJ, Verkroost-van Heemst J, Deckers JW, et al. Methods of data collection and definitions of cardiac outcomes in the Rotterdam Study. Eur J Epidemiol. 2012;27(3):173–85.
Heshmatollah A, Dommershuijsen LJ, Fani L, Koudstaal PJ, Ikram MA, Ikram MK. Long-term trajectories of decline in cognition and daily functioning before and after stroke. J Neurol Neurosurg Psychiatry. 2021;92(11):1158–63.
Heshmatollah A, Darweesh SKL, Dommershuijsen LJ, Koudstaal PJ, Ikram MA, Ikram MK. Quantitative Gait impairments in patients with stroke or transient ischemic attack: a population-based approach. Stroke. 2020;51(8):2464–71.
Vliegenthart R, Oudkerk M, Hofman A, Oei HH, van Dijck W, van Rooij FJ, et al. Coronary calcification improves cardiovascular risk prediction in the elderly. Circ. 2005;112(4):572–7.
Stel VS, Smit JH, Pluijm SM, Visser M, Deeg DJ, Lips P. Comparison of the LASA Physical activity questionnaire with a 7-day diary and pedometer. J Clin Epidemiol. 2004;57(3):252–8.
Caspersen CJ, Bloemberg BP, Saris WH, Merritt RK, Kromhout D. The prevalence of selected physical activities and their relation with coronary heart disease risk factors in elderly men: the Zutphen Study, 1985. Am J Epidemiol. 1991;133(11):1078–92.
Neves PO, Andrade J, Moncao H. Coronary artery calcium score: current status. Radiol Bras. 2017;50(3):182–9.
Clark TG, Altman DG, De Stavola BL. Quantification of the completeness of follow-up. Lancet. 2002;359(9314):1309–10.
Ridker PM. From C-Reactive protein to interleukin-6 to Interleukin-1: moving upstream to identify novel targets for atheroprotection. Circ Res. 2016;118(1):145–56.
Wu M, Rementer C, Giachelli CM. Vascular calcification: an update on mechanisms and challenges in treatment. Calcif Tissue Int. 2013;93(4):365–73.
Clemente A, Traghella I, Mazzone A, Sbrana S, Vassalle C. Vascular and valvular calcification biomarkers. Adv Clin Chem. 2020;95:73–103.
Tulunay Kaya C, Sinan Ertas F, Hasan T, Candemir B, Ozdol C, Arikan Akan O, et al. Anticalcifying nanoparticle antibody titer is an independent risk factor for coronary artery calcification. Coron Artery Dis. 2011;22(6):394–400.
Shishkova D, Markova V, Sinitsky M, Tsepokina A, Velikanova E, Bogdanov L, et al. Calciprotein particles cause endothelial dysfunction under flow. Int J Mol Sci. 2020;21(22):8802. https://doi.org/10.3390/ijms21228802.
Kutikhin AG, Brusina EB, Yuzhalin AE. The role of calcifying nanoparticles in biology and medicine. Int J Nanomed. 2012;7:339–50.
Farsi A, Domeneghetti MP, Fedi S, Capanni M, Giusti B, Marcucci R, et al. High prevalence of anti-beta2 glycoprotein I antibodies in patients with ischemic heart disease. Autoimmun. 1999;30(2):93–8.
Iverson GM, von Muhlen CA, Staub HL, Lassen AJ, Binder W, Norman GL. Patients with atherosclerotic syndrome, negative in anti-cardiolipin assays, make IgA autoantibodies that preferentially target domain 4 of beta2-GPI. J Autoimmun. 2006;27(4):266–71.
Matsuura E, Kobayashi K, Kasahara J, Yasuda T, Makino H, Koike T, et al. Anti-beta 2-glycoprotein I autoantibodies and atherosclerosis. Int Rev Immunol. 2002;21(1):51–66.
Sage AP, Mallat Z. Multiple potential roles for B cells in atherosclerosis. Ann Med. 2014;46(5):297–303.
Sage AP, Tsiantoulas D, Binder CJ, Mallat Z. The role of B cells in atherosclerosis. Nat Rev Cardiol. 2019;16(3):180–96.
Muscari A, Bozzoli C, Gerratana C, Zaca F, Rovinetti C, Zauli D, et al. Association of serum IgA and C4 with severe atherosclerosis. Atheroscler. 1988;74(1–2):179–86.
Kankaanpaa J, Sampi M, Bloigu R, Wang C, Akhi R, Kesaniemi YA, et al. IgA antibodies to phosphocholine associate with long-term cardiovascular disease risk. Atheroscler. 2018;269:294–300.
Rezaee-Zavareh MS, Tohidi M, Sabouri A, Ramezani-Binabaj M, Sadeghi-Ghahrodi M, Einollahi B. Infectious and coronary artery disease. ARYA Atheroscler. 2016;12(1):41–9.
Gurfinkel E, Lernoud V. The role of infection and immunity in atherosclerosis. Expert Rev Cardiovasc Ther. 2006;4(1):131–7.
Mehta A, Pandey A, Ayers CR, Khera A, Sperling LS, Szklo MS, et al. Predictive Value of coronary artery calcium score categories for coronary events versus strokes: impact of sex and race: MESA and DHS. Circ Cardiovasc Imaging. 2020;13(8):e010153.
Peng AW, Mirbolouk M, Orimoloye OA, Osei AD, Dardari Z, Dzaye O, et al. Long-Term all-cause and cause-specific mortality in asymptomatic patients with CAC >/=1,000: results from the CAC Consortium. JACC Cardiovasc Imaging. 2020;13(1 Pt 1):83–93.
Villasenor R, Ozmen L, Messaddeq N, Gruninger F, Loetscher H, Keller A, et al. Trafficking of endogenous immunoglobulins by endothelial cells at the blood-brain barrier. Sci Rep. 2016;6:25658.
Matsumori A, Shimada T, Shimada M, Otani H, Drayson MT, Mason JW. Immunoglobulin free light chains as inflammatory biomarkers of atrial fibrillation. Circ Arrhythm Electrophysiol. 2020;13(11):e009017.
Ridker PM. A test in context: high-sensitivity C-Reactive protein. J Am Coll Cardiol. 2016;67(6):712–23.
Phillips AC, Carroll D, Drayson MT, Batty GD. Raised levels of immunoglobulin G, A and M are associated with an increased risk of total and cause-specific mortality: the Vietnam Experience Study. J Epidemiol Community Health. 2015;69(2):129–35.
Funding
This work was supported by Takeda Pharmaceutical Company Limited [IIR-NLD-002671 to V.A.S.H.D.]. The funder was not involved in the study design, collection, analysis, interpretation of data, the writing of this article, or the decision to submit it for publication.
The Rotterdam Study is supported by the Erasmus MC University Medical Center and Erasmus University Rotterdam; The Netherlands Organisation for Scientific Research (NWO); The Netherlands Organisation for Health Research and Development (ZonMw); the Research Institute for Diseases in the Elderly (RIDE); The Netherlands Genomics Initiative (NGI); the Ministry of Education, Culture and Science; the Ministry of Health, Welfare and Sports; the European Commission (DG XII); and the Municipality of Rotterdam.
Author information
Authors and Affiliations
Contributions
Conceptualization: S.R. Khan, V.A.S.H. Dalm, R.P. Peeters, P.M. van Hagen, L. Chaker.
Methodology: S.R. Khan, V.A.S.H. Dalm, L. Chaker.
Formal analysis and investigation: S.R. Khan.
Data curation: M.K. Ikram, M. Kavousi.
Writing – original draft preparation: S.R. Khan.
Writing – review and editing: S.R. Khan, V.A.S.H. Dalm, M.K. Ikram, R.P. Peeters, P.M. van Hagen, M. Kavousi, L. Chaker.
Supervision: V.A.S.H. Dalm, R.P. Peeters, P.M. van Hagen, L. Chaker.
Corresponding author
Ethics declarations
Ethics Approval
The Rotterdam Study has been approved by the Medical Ethics Committee of the Erasmus MC (registration number MEC 02.1015) and by the Dutch Ministry of Health, Welfare and Sport (Population Screening Act WBO, license number 1071272–159521-PG). The Rotterdam Study Personal Registration Data collection is filed with the Erasmus MC Data Protection Officer under registration number EMC1712001. The Rotterdam Study has been entered into the Netherlands National Trial Register (NTR; www.trialregister.nl) and into the WHO International Clinical Trials Registry Platform (ICTRP; https://apps.who.int/trialsearch/) under shared catalogue number NL6645 / NTR6831.
Consent to Participate
All participants provided written informed consent to participate in the study and to have their information obtained from treating physicians.
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Khan, S.R., Dalm, V.A.S.H., Ikram, M.K. et al. The Association of Serum Immunoglobulins with Risk of Cardiovascular Disease and Mortality: the Rotterdam Study. J Clin Immunol 43, 769–779 (2023). https://doi.org/10.1007/s10875-023-01433-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10875-023-01433-7