Abstract
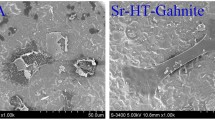
Hypoxia-inducible factor-1α (HIF-1α), a well-studied angiogenesis pathway, plays an essential role in angiogenesis-osteogenesis coupling. Targeting the HIF-1a pathway frequently leads to successful reconstruction of large-sized bone defects through promotion of angiogenesis. Dimethyloxalylglycine (DMOG) small molecule regulates the stability of HIF-1α at normal oxygen tension by mimicking hypoxia, which subsequently accelerates angiogenesis. The current study aims to develop a novel construct by seeding adipose derived mesenchymal stem cells (ADMSCs) onto a scaffold that contains DMOG to induce angiogenesis and regeneration of a critical size calvarial defect in a rat model. The spongy scaffolds have been synthesized in the presence and absence of DMOG and analyzed in terms of morphology, porosity, pore size, mechanical properties and DMOG release profile. The effect of DMOG delivery on cellular behaviors of adhesion, viability, osteogenic differentiation, and angiogenesis were subsequently evaluated under in vitro conditions. Histological analysis of cell-scaffold constructs were also performed following transplantation into the calvarial defect. Physical characteristics of fabricated scaffolds confirmed higher mechanical strength and surface roughness of DMOG-loaded scaffolds. Scanning electron microscopy (SEM) images and MTT assay demonstrated the attachment and viability of ADMSCs in the presence of DMOG, respectively. Osteogenic activity of ADMSCs that included alkaline phosphatase (ALP) activity and calcium deposition significantly increased in the DMOG-loaded scaffold. Computed tomography (CT) imaging combined with histomorphometry and immunohistochemistry analysis showed enhanced bone formation and angiogenesis in the DMOG-loaded scaffolds. Therefore, spongy scaffolds that contained DMOG and had angiogenesis ability could be utilized to enhance bone regeneration of large-sized bone defects.









Similar content being viewed by others
References
Arvidson K, Abdallah BM, Applegate LA, Baldini N, Cenni E, Gomez-Barrena E. et al. Bone regeneration and stem cells. J Cell Mol Med. 2011;15:718–46. https://doi.org/10.1111/j.1582-4934.2010.01224.x.
Khan SN, Cammisa FP Jr., Sandhu HS, Diwan AD, Girardi FP, Lane JM. The biology of bone grafting. J Am Acad Orthop Surg. 2005;13:77–86.
Frohlich M, Grayson WL, Wan LQ, Marolt D, Drobnic M, Vunjak-Novakovic G. Tissue engineered bone grafts: biological requirements, tissue culture and clinical relevance. Curr Stem Cell Res Ther. 2008;3:254–64.
Lokmic Z, Mitchell GM. Engineering the microcirculation. Tissue Eng Part B Rev. 2008;14:87–103. https://doi.org/10.1089/teb.2007.0299.
Kaigler D, Wang Z, Horger K, Mooney DJ, Krebsbach PH. VEGF scaffolds enhance angiogenesis and bone regeneration in irradiated osseous defects. J Bone Miner Res. 2006;21:735–44. https://doi.org/10.1359/jbmr.060120.
Khojasteh A, Fahimipour F, Eslaminejad MB, Jafarian M, Jahangir S, Bastami F. et al. Development of PLGA-coated beta-TCP scaffolds containing VEGF for bone tissue engineering. Mater Sci Eng C Mater Biol Appl. 2016;69:780–8. https://doi.org/10.1016/j.msec.2016.07.011.
Leach JK, Kaigler D, Wang Z, Krebsbach PH, Mooney DJ. Coating of VEGF-releasing scaffolds with bioactive glass for angiogenesis and bone regeneration. Biomaterials. 2006;27:3249–55. https://doi.org/10.1016/j.biomaterials.2006.01.033.
Chen RR, Silva EA, Yuen WW, Mooney DJ. Spatio-temporal VEGF and PDGF delivery patterns blood vessel formation and maturation. Pharm Res. 2007;24:258–64. https://doi.org/10.1007/s11095-006-9173-4.
Alsop AT, Pence JC, Weisgerber DW, Harley BAC, Bailey RC. Photopatterning of vascular endothelial growth factor within collagen-glycosaminoglycan scaffolds can induce a spatially confined response in human umbilical vein endothelial cells. Acta Biomater. 2014;10:4715–22. https://doi.org/10.1016/j.actbio.2014.07.002.
Fan L, Li J, Yu Z, Dang X, Wang K. The hypoxia-inducible factor pathway, prolyl hydroxylase domain protein inhibitors, and their roles in bone repair and regeneration. Biomed Res Int. 2014;2014:239356. https://doi.org/10.1155/2014/239356.
Wang Y, Wan C, Gilbert SR, Clemens TL. Oxygen sensing and osteogenesis. Ann N Y Acad Sci. 2007;1117:1–11. https://doi.org/10.1196/annals.1402.049.
Keith B, Johnson RS, Simon MCHIF1alpha. and HIF2alpha: sibling rivalry in hypoxic tumour growth and progression. Nat Rev Cancer. 2011;12:9–22. https://doi.org/10.1038/nrc3183.
Wilson WR, Hay MP. Targeting hypoxia in cancer therapy. Nat Rev Cancer. 2011;11:393–410. https://doi.org/10.1038/nrc3064.
Jaakkola P, Mole DR, Tian YM, Wilson MI, Gielbert J, Gaskell SJ. et al. Targeting of HIF-alpha to the von Hippel-Lindau ubiquitylation complex by O2-regulated prolyl hydroxylation. Science. 2001;292:468–72. https://doi.org/10.1126/science.1059796.
Berra E, Benizri E, Ginouves A, Volmat V, Roux D, Pouyssegur J. HIF prolyl-hydroxylase 2 is the key oxygen sensor setting low steady-state levels of HIF-1alpha in normoxia. EMBO J. 2003;22:4082–90. https://doi.org/10.1093/emboj/cdg392.
Mole DR, Schlemminger I, McNeill LA, Hewitson KS, Pugh CW, Ratcliffe PJ, et al. 2-oxoglutarate analogue inhibitors of HIF prolyl hydroxylase. Bioorg Med Chem Lett. 2003;13:2677–80.
Holotnakova T, Ziegelhoffer A, Ohradanova A, Hulikova A, Novakova M, Kopacek J. et al. Induction of carbonic anhydrase IX by hypoxia and chemical disruption of oxygen sensing in rat fibroblasts and cardiomyocytes. Pflug Arch. 2008;456:323–37. https://doi.org/10.1007/s00424-007-0400-6.
Peng J, Lai ZG, Fang ZL, Xing S, Hui K, Hao C. et al.Dimethyloxalylglycine prevents bone loss in ovariectomized C57BL/6J mice through enhanced angiogenesis and osteogenesis. PLoS ONE. 2014;9:e112744. https://doi.org/10.1371/journal.pone.0112744.
Vogel S, Wottawa M, Farhat K, Zieseniss A, Schnelle M, Le-Huu S. et al.Prolyl hydroxylase domain (PHD) 2 affects cell migration and F-actin formation via RhoA/rho-associated kinase-dependent cofilin phosphorylation. J Biol Chem. 2010;285:33756–63.https://doi.org/10.1074/jbc.M110.132985.
Qi X, Liu Y, Ding ZY, Cao JQ, Huang JH, Zhang JY. et al. Synergistic effects of dimethyloxallyl glycine and recombinant human bone morphogenetic protein-2 on repair of critical-sized bone defects in rats. Sci Rep. 2017;7:42820. https://doi.org/10.1038/srep42820.
Oryan A, Kamali A, Moshiri A, Baghaban Eslaminejad M. Role of mesenchymal stem cells in bone regenerative medicine: what is the evidence?. Cells Tissues Organs. 2017;204:59–83. https://doi.org/10.1159/000469704.
Fu WL, Xiang Z, Huang FG, Gu ZP, Yu XX, Cen SQ. et al.Coculture of peripheral blood-derived mesenchymal stem cells and endothelial progenitor cells on strontium-doped calcium polyphosphate scaffolds to generate vascularized engineered bone. Tissue Eng Part A. 2015;21:948–59.https://doi.org/10.1089/ten.TEA.2014.0267.
Koob S, Torio-Padron N, Stark GB, Hannig C, Stankovic Z, Finkenzeller G. Bone formation and neovascularization mediated by mesenchymal stem cells and endothelial cells in critical-sized calvarial defects. Tissue Eng Part A. 2011;17:311–21. https://doi.org/10.1089/ten.TEA.2010.0338.
Strem BM, Hicok KC, Zhu M, Wulur I, Alfonso Z, Schreiber RE, et al. Multipotential differentiation of adipose tissue-derived stem cells. Keio J Med. 2005;54:132–41.
Baer PC, Geiger H. Adipose-derived mesenchymal stromal/stem cells: tissue localization, characterization, and heterogeneity. Stem Cells Int. 2012;2012:812693. https://doi.org/10.1155/2012/812693.
Rennerfeldt DA, Van Vliet KJ. Concise review: when colonies are not clones: evidence and implications of intracolony heterogeneity in mesenchymal. Stem Cells. 2016;34:1135–41. https://doi.org/10.1002/stem.2296.
Eslaminejad MB, Mirzadeh H, Mohamadi Y, Nickmahzar A. Bone differentiation of marrow-derived mesenchymal stem cells using beta-tricalcium phosphate-alginate-gelatin hybrid scaffolds. J Tissue Eng Regen Med. 2007;1:417–24. https://doi.org/10.1002/term.49.
Ceradini DJ, Kulkarni AR, Callaghan MJ, Tepper OM, Bastidas N, Kleinman ME. et al. Progenitor cell trafficking is regulated by hypoxic gradients through HIF-1 induction of SDF-1. Nat Med. 2004;10:858–64. https://doi.org/10.1038/nm1075.
Greijer AE, van der Groep P, Kemming D, Shvarts A, Semenza GL, Meijer GA. et al. Up-regulation of gene expression by hypoxia is mediated predominantly by hypoxia-inducible factor 1 (HIF-1). J Pathol. 2005;206:291–304. https://doi.org/10.1002/path.1778.
Kusumbe AP, Ramasamy SK, Adams RH. Coupling of angiogenesis and osteogenesis by a specific vessel subtype in bone. Nature. 2014;507:323–8. https://doi.org/10.1038/nature13145.
Riddle RC, Khatri R, Schipani E, Clemens TL. Role of hypoxia-inducible factor-1alpha in angiogenic-osteogenic coupling. J Mol Med (Berl). 2009;87:583–90. https://doi.org/10.1007/s00109-009-0477-9.
Wan C, Shao J, Gilbert SR, Riddle RC, Long F, Johnson RS. et al. Role of HIF-1alpha in skeletal development. Ann N Y Acad Sci. 2010;1192:322–6. https://doi.org/10.1111/j.1749-6632.2009.05238.x.
Asikainen TM, Ahmad A, Schneider BK, Ho WB, Arend M, Brenner M. et al. Stimulation of HIF-1alpha, HIF-2alpha, and VEGF by prolyl 4-hydroxylase inhibition in human lung endothelial and epithelial cells. Free Radic Biol Med. 2005;38:1002–13. https://doi.org/10.1016/j.freeradbiomed.2004.12.004.
Ding H, Gao YS, Wang Y, Hu C, Sun Y, Zhang C. Dimethyloxaloylglycine increases the bone healing capacity of adipose-derived stem cells by promoting osteogenic differentiation and angiogenic potential. Stem Cells Dev. 2014;23:990–1000. https://doi.org/10.1089/scd.2013.0486.
Rey S, Lee K, Wang CJ, Gupta K, Chen S, McMillan A. et al. Synergistic effect of HIF-1alpha gene therapy and HIF-1-activated bone marrow-derived angiogenic cells in a mouse model of limb ischemia. Proc Natl Acad Sci USA. 2009;106:20399–404. https://doi.org/10.1073/pnas.0911921106.
Tan R, Niu X, Gan S, Feng Q.Preparation and characterization of an injectable composite. J Mater Sci Mater Med. 2009;20:1245–53.https://doi.org/10.1007/s10856-009-3692-6.
Wu C, Zhou Y, Chang J, Xiao Y. Delivery of dimethyloxallyl glycine in mesoporous bioactive glass scaffolds to improve angiogenesis and osteogenesis of human bone marrow stromal cells. Acta Biomater. 2013;9:9159–68. https://doi.org/10.1016/j.actbio.2013.06.026.
Aronson J. Temporal and spatial increases in blood flow during distraction osteogenesis. Clin Orthop Relat Res. 1994;301:124–31.
Mooney DJ, Mikos AG. Growing new organs. Sci Am. 1999;280:60–5.
Yu H, VandeVord PJ, Mao L, Matthew HW, Wooley PH, Yang SY. Improved tissue-engineered bone regeneration by endothelial cell mediated vascularization. Biomaterials. 2009;30:508–17. https://doi.org/10.1016/j.biomaterials.2008.09.047.
Agis H, Hueber L, Pour Sadeghian N, Pensch M, Gruber R. In vitro release of dimethyloxaloylglycine and l-mimosine from bovine bone mineral. Arch Oral Biol. 2014;59:1024–31. https://doi.org/10.1016/j.archoralbio.2014.05.027.
Kim BS, Mooney DJ. Development of biocompatible synthetic extracellular matrices for tissue engineering. Trends Biotechnol. 1998;16:224–30.
Min Z, Shichang Z, Chen X, Yufang Z, Changqing Z. 3D-printed dimethyloxallyl glycine delivery scaffolds to improve angiogenesis and osteogenesis. Biomater Sci. 2015;3:1236–44. https://doi.org/10.1039/c5bm00132c.
Engler AJ, Sen S, Sweeney HL, Discher DE. Matrix elasticity directs stem cell lineage specification. Cell. 2006;126:677–89. https://doi.org/10.1016/j.cell.2006.06.044.
Tokuda EY, Leight JL, Anseth KS. Modulation of matrix elasticity with PEG hydrogels to study melanoma drug responsiveness. Biomaterials. 2014;35:4310–8. https://doi.org/10.1016/j.biomaterials.2014.01.063.
Jaakkola P, Mole DR, Tian Y-M, Wilson MI, Gielbert J, Gaskell SJ, et al. Targeting of HIF-α to the von Hippel-Lindau ubiquitylation complex by O2- regulated prolyl hydroxylation. Science. 2001;292:468.
Blum JS, Barry MA, Mikos AG, Jansen JA. In vivo evaluation of gene therapy vectors in ex vivo-derived marrow stromal cells for bone regeneration in a rat critical-size calvarial defect model. Hum Gene Ther. 2003;14:1689–701. https://doi.org/10.1089/104303403322611719.
Cowan CM, Aghaloo T, Chou YF, Walder B, Zhang X, Soo C. et al. MicroCT evaluation of three-dimensional mineralization in response to BMP-2 doses in vitro and in critical sized rat calvarial defects. Tissue Eng. 2007;13:501–12. https://doi.org/10.1089/ten.2006.0141.
Yoon E, Dhar S, Chun DE, Gharibjanian NA, Evans GR. In vivo osteogenic potential of human adipose-derived stem cells/poly lactide-co-glycolic acid constructs for bone regeneration in a rat critical-sized calvarial defect model. Tissue Eng. 2007;13:619–27. https://doi.org/10.1089/ten.2006.0102.
Acknowledgements
The present research was financially supported by Royan Institute for Stem Cell Biology and Technology. We thank Ms. Fatemeh Safari and Mr. Mohammad Hossein Ghanian for their help.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Jahangir, S., Hosseini, S., Mostafaei, F. et al. 3D-porous β-tricalcium phosphate–alginate–gelatin scaffold with DMOG delivery promotes angiogenesis and bone formation in rat calvarial defects. J Mater Sci: Mater Med 30, 1 (2019). https://doi.org/10.1007/s10856-018-6202-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10856-018-6202-x