Abstract
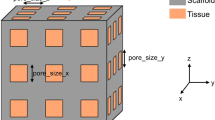
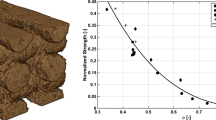
In bone tissue engineering, both geometrical and mechanical properties of a scaffold play a major part in the success of the treatment. The mechanical stresses and strains that act on cells on a scaffold in a physiological environment are a determining factor on the subsequent tissue formation. Computational models are often used to simulate the effect of changes of internal architectures and external loads applied to the scaffold in order to optimise the scaffold geometry for the prospective implantation site. Finite element analysis (FEA) based on computer models of the scaffold is a common technique, but would not take into account actual inaccuracies due to the manufacturing process. Image based FEA using CT scans of fabricated scaffolds can provide a more accurate analysis of the scaffold, and was used in this work in order to accurately simulate and predict the mechanical performance of bone tissue engineering scaffolds, fabricated using selective laser sintering (SLS), with a view to generating a methodology that could be used to optimise scaffold design. The present work revealed that an approach that assumes isotropic properties of SLS fabricated scaffolds will lead to inaccurate predictions of the FE model. However, a dependency of the greyvalue of the CT scans and the mechanical properties was discovered, which may ultimately lead to accurate FE models without the need of experimental validation.














Similar content being viewed by others
References
Langer R, Vacanti J. Tissue engineering. Science. 1993;260:920–6.
Brown TD. Techniques for mechanical stimulation of cells in vitro: a review. J Biomech. 2000;33:3–14.
Butler DL, Goldstein SA, Guilak F. Functional tissue engineering, the role of biomechanics. J Biomech Eng. 2000;122:570–5.
Davies J. Mechanisms of endosseous integration. Int J Prosthodont. 1998;11:391–401.
Hollister SJ, Lin CY. Computational design of tissue engineering scaffolds. Comput Methods Appl Mech Eng. 2007;196:2991–8.
Ikegame M, Ishibashi K, Yoshizawa T, Shimomura J, Komori T, Ozawa H, et al. Tensile stress induces bone morphogenetic protein 4 in preosteoblastic and fibroblastic cells, which later differentiate into osteoblasts leading to osteogenesis in the mouse calvariae in organ culture. J Bone Miner Res. 2001;16:24–32.
Lo H, Ponticiello MS, Leong KW. Fabrication of controlled release biodegradable foams by phase separation. Tissue Eng. 1995;1:15–28.
Mullender M, Haj AJE, Yang Y, van Duin MA, Burger EH, Klein-Nulend J. Mechanotransduction of bone cells in vitro: mechanobiology of bone tissue. Med Biol Eng Comput. 2006;42:14–21.
Wettergreen MA, Bucklen S, Starly B, Yuksel E, Sun W, Liebschner MAK. Creation of a unit block library of architectures for use in assembled scaffold engineering. Comput Aided Des. 2005;37:1141–9.
Cheah CM, Chua CK, Leong KR, Chua SW. Development of a tissue engineering scaffold structure library for rapid prototyping. Part 2: parametric library and assembly program. Int J Adv Manuf Technol. 2003;21:302–12.
Luxner M, Stampfl J, Pettermann H. Finite element modeling concepts and linear analyses of 3D regular open cell structures. J Mater Sci. 2005;40:5859–66.
Naing MW, Chua CK, Leong KF, Wang Y. Fabrication of customised scaffolds using computer-aided design and rapid prototyping techniques. Rapid Prototyp J. 2005;11:249–59.
Yang S, Leong K-F, Du Z, Chua C-K. The design of scaffolds for use in tissue engineering. Part I. Traditional factors. Tissue Eng. 2001;7:679–89.
Williams JM, Adewunmi A, Schek RM, Flanagan CL, Krebsbach PH, Feinberg SE, et al. Bone tissue engineering using polycaprolactone scaffolds fabricated via selective laser sintering. Biomaterials. 2005;26:4817–27.
Eshraghi S, Das S. Micromechanical finite-element modeling and experimental characterization of the compressive mechanical properties of polycaprolactone–hydroxyapatite composite scaffolds prepared by selective laser sintering for bone tissue engineering. Acta Biomater. 2012;8:3138–43.
Cahill S, Lohfeld S, McHugh P. Finite element predictions compared to experimental results for the effective modulus of bone tissue engineering scaffolds fabricated by selective laser sintering. J Mater Sci. 2009;20:1255–62.
Jaecques SVN, Van Oosterwyck H, Muraru L, Van Cleynenbreugel T, De Smet E, Wevers M, et al. Individualised, micro CT-based finite element modelling as a tool for biomechanical analysis related to tissue engineering of bone. Biomaterials. 2004;25:1683–96.
Lacroix D, Chateau A, Ginebra M-P, Planell JA. Micro-finite element models of bone tissue-engineering scaffolds. Biomaterials. 2006;27:5326–34.
Sandino C, Planell JA, Lacroix D. A finite element study of mechanical stimuli in scaffolds for bone tissue engineering. J Biomech. 2008;41:1005–14.
Van Cleynenbreugel T, Schrooten J, Van Oosterwyck H, Vander Sloten J. Micro-CT-based screening of biomechanical and structural properties of bone tissue engineering scaffolds. Med Biol Eng Comput. 2006;44:517–25.
Lohfeld S, Tyndyk MA, Cahill S, Flaherty N, Barron V, McHugh PE. A method to fabricate small features on scaffolds for tissue engineering via selective laser sintering. J Biomed Sci Eng. 2010;3:138–47.
Harrison NM, McDonnell PF, O’Mahoney DC, Kennedy OD, O’Brien FJ, McHugh PE. Heterogeneous linear elastic trabecular bone modelling using micro-CT attenuation data and experimentally measured heterogeneous tissue properties. J Biomech. 2008;41:2589–96.
Teo JCM, Si-Hoe KM, Keh JEL, Teoh SH. Correlation of cancellous bone microarchitectural parameters from microCT to CT number and bone mechanical properties. Mater Sci Eng C. 2007;27:333–9.
Tuan HS, Hutmacher DW. Application of micro CT and computation modeling in bone tissue engineering. Comput Aided Des. 2005;37:1151–61.
Caulfield B, McHugh PE, Lohfeld S. Dependence of mechanical properties of polyamide components on build parameters in the SLS process. J Mater Process Technol. 2007;182:477–88.
Acknowledgments
Thanks for performing the µCT scans to the University of Naples, Italy (PCL scaffolds), and to the University of Aberdeen, UK (PCL/TCP scaffolds). The authors acknowledge research funding from the European Union through the FP6 project “STEPS” (contract number FP6-500465).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lohfeld, S., Cahill, S., Doyle, H. et al. Improving the finite element model accuracy of tissue engineering scaffolds produced by selective laser sintering. J Mater Sci: Mater Med 26, 38 (2015). https://doi.org/10.1007/s10856-014-5376-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10856-014-5376-0