Abstract
Background
High-power short-duration (HPSD) ablation has emerged as an alternative to conventional standard-power long-duration (SPLD) ablation. We aim to assess the efficacy and safety of HPSD versus SPLD for atrial fibrillation (AF) ablation.
Methods
A systematic review and meta-analysis of randomized controlled trials (RCTs) retrieved from PubMed, WOS, SCOPUS, EMBASE, and CENTRAL were performed through August 2023. We used RevMan V. 5.4 to pool dichotomous data using risk ratio (RR) and continuous data using mean difference (MD) with a 95% confidence interval (CI). PROSPERO ID: CRD42023471797.
Results
We included six RCTs with a total of 694 patients. HPSD was significantly associated with a decreased total procedure time (MD: -22.88 with 95% CI [-36.13, -9.63], P = 0.0007), pulmonary vein isolation (PVI) time (MD: -19.73 with 95% CI [-23.93, -15.53], P < 0.00001), radiofrequency time (MD: -10.53 with 95% CI [-12.87, -8.19], P < 0.00001). However, there was no significant difference between HPSD and SPLD ablation with respect to the fluoroscopy time (MD: -0.69 with 95% CI [-2.00, 0.62], P = 0.30), the incidence of esophageal lesions (RR: 1.15 with 95% CI [0.43, 3.07], P = 0.77), and the incidence of first pass isolation (RR: 0.98 with 95% CI [0.88, 1.08], P = 0.65).
Conclusion
HPSD ablation was significantly associated with decreased total procedure time, PVI time, and radiofrequency time compared with SPLD ablation. On the contrary, SPLD ablation was significantly associated with low maximum temperature.
Graphical Abstract

Similar content being viewed by others
1 Introduction
Current guidelines recommend catheter ablation for patients with symptomatic atrial fibrillation (AF) who are refractory or intolerant to anti-arrhythmic drugs (AAD). Additionally, catheter ablation may serve as an initial rhythm-control strategy for certain patients experiencing symptomatic paroxysmal AF, with the goal of alleviating symptoms and mitigating progression to persistent AF [1]. Catheter ablation was shown to be more effective in maintaining normal sinus rhythm than AAD [2,3,4,5,6,7].
The prime triggers behind AF initiation and perpetuation are ectopic electrical discharges stemming from pulmonary veins in the left atrium [8]. Therefore, ablation procedures aim to isolate the pulmonary vein by creating circumferential ablation lesions that encircle the pulmonary veins ostia. Radiofrequency ablation (RFA) and cryo-ablation are the commonly used and approved ablation techniques with comparable efficacy [9, 10].
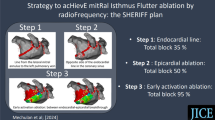
RFA delivers thermal energy to cauterize cardiac tissue. The efficacy and safety of RFA depend on achieving full-thickness and durable lesions without causing collateral damage, such as esophageal thermal injury (ETI) and pericardial effusion due to cardiac perforation. The key factors influencing the design of the created lesion, including its size and depth, are power, duration, catheter stability, and contact force [11]. Recently, high-power short-duration (HPSD) ablation (40–50 W) has emerged as an alternative to conventional standard-power long-duration (SPLD) ablation (25–35 W). Retrospective studies comparing HPSD to SPLD ablation have suggested shorter procedure times with comparable efficacy and safety profiles with HPSD lesions [12,13,14]. Theoretically, the HPSD technique delivers more significant resistive heating to the surrounding myocardium, whereas the SPLD technique delivers more significant conductive heating within the distal myocardium and surrounding structures [15]. Several randomized controlled trials (RCTs) have been conducted to compare HPSD and SPLD RFA outcomes [16,17,18,19,20,21].
To thoroughly assess the existing data and aid in clinical decision-making, we conducted this systematic review and meta-analysis to investigate outcomes, such as procedure duration, recurrence rates, first-pass isolation rates, and safety profile between HPSD and SPLD in AF patients undergoing RFA.
2 Methodology
2.1 Protocol registration
This study complied with the PROSPERO protocol, registered under ID: CRD42023471797. We adhered to the PRISMA statement guidelines for systematic reviews and meta-analysis [22] and the Cochrane Handbook for Systematic Reviews and Meta-Analysis [23] guidelines.
2.2 Data sources & search strategy
Data Sources & Search Strategy: PubMed (Medline), EMBASE, Web of Science, SCOPUS, and Cochrane Central Register of Controlled Trials (CENTRAL) were scoured by two researchers (A.M.A. and M.A.) from their inception to August 2023. A distinct search approach was applied to each database, as detailed in (Table S1).
2.3 Eligibility criteria
RCTs followed the following Population, Intervention, Comparison, and Outcomes (PICO) criteria were included: population (P): patients with paroxysmal and persistent AF; intervention (I): HPSD; control (C): SPLD; outcome (O): our primary outcomes were total procedure time, pulmonary vein isolation (PVI) time, radiofrequency (RF) application time, fluoroscopy time, and esophageal lesions while secondary outcomes included: AF recurrence, atrial flutter (AFL)/ atrial tachycardia (AT) recurrence, atrial arrhythmias recurrence, first pass left pulmonary vein (LPV) isolation, first pass right pulmonary vein (RPV) isolation, and first pass isolation. In addition, safety outcomes included any complications and maximum temperature. Studies were excluded if they were: (1) letters, theses, editorials, book chapters, cohort studies, case series, case reports, single-arm studies, animal studies, in vitro research, or preliminary studies; (2) research where data was solely sourced from abstracts.
2.4 Study selection
The initial step was to screen titles and abstracts independently by three researchers (O.A., M.A.A., and A.A.) using the Covidence online platform. Post deduplication removal, dual independent screening was applied to each citation. The same reviewers undertook the full-text review, with discrepancies settled by a third reviewer (A.M.A. and M.A.) in accordance with our previous eligibility criteria.
2.5 Data extraction
A standardized Excel extraction template, which had undergone preliminary testing, was employed by four reviewers (O.A., M.A., and A.A.) to retrieve pertinent information from the selected studies. This encompassed: (1) a summary section detailing the study's design, nation of origin, the number of participating centers, total participants, aims for the intervention and control, techniques employed for both, power specifications, essential inclusion prerequisites, primary results, and the span of the follow-up; (2) baseline information (Number of patients in each group, sex (male), age (Years), BMI, CHA2DS2-VASc score, left ventricular ejection fraction (LVEF), AF type (paroxysmal or persistent). We also included comorbidities, which include hypertension, diabetes mellitus, ischemic heart disease (IHD), or coronary artery disease, obstructive sleep apnea, and stroke; and (3) study outcomes (AF Recurrence, AFL/AT recurrence, atrial arrhythmias recurrence, first pass LPV isolation, first pass RPV isolation, and first pass isolation, total procedure time, PVI time, RF application time, fluoroscopy time, maximum temperature. We also looked at safety data, which included any complications and esophageal lesions. Conflicts were discussed and resolved by consensus.
2.6 Risk of bias and certainty of evidence
Three reviewers (M.A., O.A., and A.A.) independently used the Cochrane ROB2 tool [24] for quality assessment. The domains that were evaluated included the risk of bias resulting from the randomization process, the risk of bias due to deviation from the intended intervention, the risk of bias due to missing outcome data, the risk of bias in measuring the outcome, and the risk of bias in selecting the reported results. The reviewers resolved any conflicts by consensus.
M.A. used the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) guidelines [25, 26] to evaluate the certainty of evidence for each outcome. The decisions made were justified and recorded.
2.7 Statistical analysis
RevMan v5.3 was used to run the statistical analysis [27]. To pool the results of dichotomous outcomes, we used the risk ratio (RR), while for the continuous outcomes, we used the mean difference (MD), both with a 95% confidence interval (CI). We performed both the Chi-square and I-square tests to evaluate heterogeneity, where the Chi-square test detects the presence of heterogeneity, and the I-square test evaluates its degree. I-square was interpreted In accordance with the Cochrane Handbook (chapter nine) [23] as follows: heterogeneity is not significant for 0–40 percent, moderate for 30–60 percent, substantial for 50–90 percent, and considerable for 75–100 percent. We considered an alpha level below 0.1 for the Chi-square test to detect significant heterogeneity. A leave-one-out sensitivity analysis was employed to resolve the heterogeneity by excluding each study one time from the pooled analyzed studies.
We made a subgroup analysis between studies that used ≥ 50 W versus < 50 W in the HPSD arm.
3 Results
3.1 Search results and study selection
Using our search strategy, we searched (PubMed, Cochrane, Embase, Web of Science, and Scopus), and reached 1534 studies. A total of 834 duplicate studies were removed, and 616 were excluded after screening their titles and abstracts. We reviewed the full text of the remaining 84 studies; 78 were removed from the final assessment and subsequent data analysis (Fig. 1).
3.2 Characteristics of included studies
In brief, six RCTs [16,17,18,19,20,21] were included for the final review and data analysis. The total number of patients was 694, with 411 patients in the HPSD group and 283 in the SPLD group. More details about the trials’ inclusion criteria, ablation guidance, and ablation target with baseline trials’ participants' comorbidities are outlined in (Table 1, 2, and S2-S3).
3.3 Risk of bias and certainty of evidence
We used Cochrane RoB 2 to assess the risk of bias. One study had an overall high risk of bias [17], while five studies had an overall some concerns [16, 18,19,20,21]. Results are shown in (Fig. 2). In addition, the authors’ descriptions of the consequences of their decisions are outlined in (Table S4). Finally, the certainty of evidence is demonstrated in a GRADE evidence profile (Table 3).
Quality assessment of risk of bias in the included trials. The upper panel presents a schematic representation of risks (low = green, unclear = yellow, and high = red) for specific types of biases of each study in the review. The lower panel presents risks (low = green, unclear = yellow, and high = red) for the subtypes of biases of the combination of studies included in this review
3.4 Primary outcomes
HPSD ablation was significantly associated with decreased total procedure time (MD: -22.88 with 95% CI [-36.13, -9.63], P = 0.0007) (Fig. 3A), PVI time (MD: -19.73 with 95% CI [-23.93, -15.53], P < 0.00001) (Fig. 3B), and radiofrequency application time (MD: -10.53 with 95% CI [-12.87, -8.19], P < 0.00001) (Fig. 3C). However, there was no significant difference between HPSD and SPLD ablation in fluoroscopy time (MD: -0.69 with 95% CI [-2.00, 0.62], P = 0.30) (Fig. 3D) and the incidence of esophageal lesions (RR: 1.15 with 95% CI [0.43, 3.07], P = 0.77) (Fig. 3E).
The pooled studies were homogenous in PVI time (I2 = 48%, P = 0.15) and esophageal lesions (I2 = 0%, P = 0.99). However, pooled studies were heterogeneous in total procedure time (I2 = 86%, P < 0.00001), radiofrequency application time (I2 = 76%, P = 0.006), and fluoroscopy time (I2 = 84%, P = 0.002). Regarding total procedure time and radiofrequency application time, heterogeneity was not resolved by leave-one-out sensitivity analysis. Regarding fluoroscopy time, heterogeneity was best resolved by excluding Shin et al. 2021 (I2 = 3%, P = 0.31) (Table S5).
Test for subgroup analysis based on the power used in the HPSD group was not significant across all outcomes (P > 0.1) (Figures S1-S5).
3.5 Secondary outcomes
HPSD was significantly associated with decreased incidence of AF recurrence (RR: 0.60 with 95% CI [0.37, 0.98], P = 0.04) (Fig. 4A). However, there was no significant difference between HPSD and SPLD ablation in the incidence of AFL/AT recurrence (RR: 0.61 with 95% CI [0.24, 1.54], P = 0.29) (Fig. 4B), the incidence of atrial arrhythmias recurrence (RR: 0.91 with 95% CI [0.64, 1.28], P = 0.58) (Fig. 4C), the incidence of first pass isolation (RR: 0.98 with 95% CI [0.88, 1.08], P = 0.65) (Fig. 4D), the incidence of first pass LPV isolation (RR: 1.00 with 95% CI [0.93, 1.07], P = 0.92) (Fig. 5A), the incidence of first pass RPV isolation (RR: 1.06 with 95% CI [0.88, 1.27], P = 0.54) (Fig. 5B), and the incidence of any complications (RR: 1.15 with 95% CI [0.50, 2.67], P = 0.74) (Fig. 5C). On the contrary, SPLD ablation was significantly associated with low maximum temperature (MD: 3.91 with 95% CI [0.98, 6.84], P = 0.009) (Fig. 5D).
The pooled studies were homogenous in AF recurrence (I2 = 44%, P = 0.15), AFL/AT recurrence (I2 = 0%, P = 0.98), atrial arrhythmias recurrence (I2 = 42%, P = 0.16), first pass isolation (I2 = 0%, P = 0.32), first pass LPV isolation (I2 = 11%, P = 0.34), and the incidence of any complications (I2 = 0%, P = 1.00). However, pooled studies were heterogeneous in first-pass RPV isolation (I2 = 70%, P = 0.02). Regarding first-pass RPV isolation, leave-one-out sensitivity analysis did not resolve heterogeneity (Table S5).
Test for subgroup analysis based on the power used in the HPSD group was not significant across all outcomes (P > 0.1) (Figures S6-S11).
4 Discussion
The important findings of our current investigation are 1) HPSD was significantly associated with reduced procedure time, PVI time, and RF application time; 2) No significant difference was observed between HPSD and SPLD ablation regarding fluoroscopy time; 3) No significant difference was found between HPSD and SPLD ablation with respect to esophageal lesions; 4) HPSD was significantly associated with a decreased incidence of AF recurrence compared to SPLD ablation; 5) No significant difference was observed between HPSD and SPLD ablation regarding the incidence of first-pass isolation or any complications.
Successful AF ablations aim to achieve electrical isolation of pulmonary veins by creating a transmural scar with minimal collateral tissue damage. Lesion quality is crucial for a durable PVI. The RF power, duration, contact force, and catheter stability determine the lesion characteristics, including its diameter and depth. Ablation index (AI) is a weighted formula incorporating power, duration, and contact force, which has been introduced to predict and quantify lesion quality, with RF power having the largest contributor to it [28,29,30].
HPSD ablation improves lesion quality by maximizing resistive heating and minimizing conductive heating. Additionally, collateral tissue injury with respect to the esophagus can primarily be reduced by minimizing conductive heating as well [11, 31]. Resistive heating is a direct form of energy that occurs immediately upon catheter-myocardium interaction and ceases with RF application termination. On the other hand, conductive heating is an indirect form of energy transfer that affects distant tissues and continues even after RF application for a few seconds [15].
In our analysis, despite the significant association between HPSD and reduced AF recurrence, no significant association was observed between HPSD and AFL/AT recurrence. This discrepancy might be attributed to the role of pulmonary veins as an essential source of AF, unlike AFL/AT. Consequently, optimizing PVI lesion quality would be beneficial in AF rather than AFL/AT.
There was some noted variability in the definitions of SPLD ablation and HPSD ablation across the included studies. While HPSD was most frequently defined as 40-50W power, O’Neill et al. utilized the QDOT MICRO catheter, specifically designed for HPSD ablation, delivering a notably high power (90w) over 4 s in a temperature-controlled mode), which did not significantly correlate with reduced arrhythmias recurrence [19].
Atrioesophageal fistula (AEF) is a feared complication of AF ablation with a mortality of 60–70%. The incidence of AEF is 0.1 to 0.25% among AF ablation procedures, and it represents the second most common cause of death following AF ablation procedures along with stroke [32,33,34]. Even though our results demonstrated a significant association between HPSD ablation and a higher maximum temperature, there was no significant difference between HPSD and SPLD ablation in the incidence of esophageal lesions, suggesting that the higher temperature with HPSD did not result in clinically significant esophageal lesions.
Safety of HPSD ablation was demonstrated by Winkle et al., who reported very low complication rates in 10,284 patients [13]. Additionally, Vassalo et al. reported similar safety, similar efficacy, and reduced procedural and RF time in their observational study comparing HPSD to SPLD ablation [35]. Dhillon et al. analysis, including 100 patients, demonstrated shorter procedure times, reduced PV reconnection, and similar recurrence compared to SPLD [36].
Esophageal injury is a major concern, especially during posterior wall ablation. A prospective study by Chen et al. reported esophageal lesions in 3.5% of 122 patients undergoing HPSD AF ablation [37]. Another prospective study by Muller et al. reported esophageal lesions in 6% of 953 patients undergoing HPSD AF ablations [38]. A non-randomized comparison by Kaneshiro showed no difference in the incidence of esophageal lesions among 271 patients (7% versus 8%). The mechanism behind the safety profile of HPSD AF ablation is thought to involve maximizing resistive heating and minimizing conductive heating [11, 31]. Using Kansas City Classification, Francke et al. reported esophageal lesions graded as two deep ulcers (Type 2B) in the standard group and 13 cases in the HPSD group, which were three erythema (Type 1), nine superficial ulcers (Type 2A) and one deep ulcer (Type 2B) [17], Wielandts et al. reported a superficial ulcer (Type 2A) in the control group and perforation without communication with the atria (Type 3A), and Chieng et al. reported all ETI cases as superficial ulcers (Type 2A) [21]. However, O’Neill et al. reported one esophageal ulcer in the SPLD group and one small superficial esophageal erosion in the HPSD group [19].
In addition, we found that four RCTs reported no incidence of stroke in both groups [18,19,20,21]. Moreover, Francke et al. and Wielandts et al. reported no incidence of steam pops [17, 21]. However, O’Neill et al. reported the incidence of steam pops in one case in the HPSD arm [19].
In the POWER-AF trial, a narrower safety margin for HPSD on the posterior wall was observed, suggesting the need for increased preventive measures during posterior wall ablation and thorough post-procedural follow-up, including endoscopic evaluation.
Moreover, a recent meta-analysis of 15 retrospective observational studies with a total of 2,718 patients found that HPSD was associated with higher freedom from atrial arrhythmias (OR 1.44, P = 0.009), shorter total procedure duration (mean difference -37.35 min, P < 0.001), decreased fluoroscopy duration (mean difference -5.23 min, P < 0.001), and reduced RFA time (mean difference -16.26 min, p < 0.001), with a similar safety profile compared to SPLD [39].
These findings align with our study, indicating that HPSD ablation has a superior efficacy in preventing AF recurrence with shorter procedure and RFA time. The reduction in procedure time contributes to lower anaesthesia time and decreased anaesthesia-related complications. Furthermore, minimizing instrumentation time in the left atrium lowers the risk of periprocedural stroke, which is the second most common cause of death after AF ablation along with AEF [34].
5 Limitations
Our results must be interpreted cautiously, considering the Cochrane ROB2 tool. One of the six RCTs [17] was judged to have high concerns about bias arising from the randomization process. Additionally, five of the six RCTs [16, 18,19,20,21] were judged to have some concerns for bias arising from deviations in intended interventions. In addition, one of the six RCTs [18] was judged to have some concerns about bias arising from the randomization process. Lastly, two of the six RCTs [17, 21] were also judged to have some concerns about bias in selecting reported results.
Our study is limited by variations in SPLD ablation and HPSD ablation definitions across included RCTs. Specifically, the POWER PLUS trial compared very HPSD ablation at 90 W to hybrid ablation at 35–50 W, whereas other RCTs in our analysis employed 40–50 W in the interventional group, comparing it to standard ablation with 20–40 W. The POWER PLUS trial was the only study using the QDot catheter, contributing to the heterogeneity of this trial compared to all other included trials.
Most studies utilized an electroanatomic three-dimensional mapping system, with CARTO being the most commonly employed system. Generalizability of results to ablation procedures using alternative systems or without mapping may be limited.
There was some heterogeneity in the use of continuous intraprocedural esophageal temperature monitoring. While most studies employed temperature monitoring, Shin et al. and Francke et al. did not utilize any. Moreover, none of the studies reported differences in esophageal temperature spikes or alert rates between SPLD and HPSD ablation.
Subgroup analysis based on AF-type, paroxysmal versus persistent AF, was not applicable due to a lack of separate data for each AF-type.
6 Implications for future research
Future research is required to investigate the optimal power settings for AF ablation, given the variation in power thresholds across studies. Additionally, working towards standardizing protocols for HPSD and SPLD ablation procedures is essential to facilitate comparison across studies. Future research should investigate patient-reported outcomes to assess the quality of life and symptom improvement following ablation procedures.
7 Conclusion
Our systematic review and meta-analysis suggest that HPSD ablation is significantly associated with a decreased incidence of AF recurrence compared to SPLD ablation, with a comparable safety profile. HPSD ablation also significantly reduces procedure, PVI, and RF application time, with no significant difference in fluoroscopy time or the incidence of first-pass isolation. HPSD ablation could represent a safe and effective alternative to conventional SPLD ablation. On the contrary, SPLD ablation was significantly associated with low maximum temperature.
Data availability
Not applicable.
References
Joglar JA, Chung MK, Armbruster AL, Benjamin EJ, Chyou JY, Cronin EM, … Van Wagoner DR. 2023 ACC/AHA/ACCP/HRS Guideline for the Diagnosis and Management of Atrial Fibrillation: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2024;149(1):e1–e156. https://doi.org/10.1161/CIR.0000000000001193.
Jons C, Hansen PS, Johannessen A, Hindricks G, Raatikainen P, Kongstad O, … Nielsen JC. The Medical ANtiarrhythmic Treatment or Radiofrequency Ablation in Paroxysmal Atrial Fibrillation (MANTRA-PAF) trial: clinical rationale, study design, and implementation. Europace. 2009;11(7):917–923. https://doi.org/10.1093/europace/eup122.
Calkins H, Reynolds MR, Spector P, Sondhi M, Xu Y, Martin A, … Sledge I. Treatment of atrial fibrillation with antiarrhythmic drugs or radiofrequency ablation: two systematic literature reviews and meta-analyses. Circ Arrhythm Electrophysiol. 2009;2(4), 349–361. https://doi.org/10.1161/CIRCEP.108.824789.
Bonanno C, Paccanaro M, La Vecchia L, Ometto R, Fontanelli A. Efficacy and safety of catheter ablation versus antiarrhythmic drugs for atrial fibrillation: a meta-analysis of randomized trials. J Cardiovasc Med (Hagerstown, Md). 2010;11(6):408–18. https://doi.org/10.2459/JCM.0b013e328332e926.
Nair GM, Nery PB, Diwakaramenon S, Healey JS, Connolly SJ, Morillo CA. A systematic review of randomized trials comparing radiofrequency ablation with antiarrhythmic medications in patients with atrial fibrillation. J Cardiovasc Electrophysiol. 2009;20(2):138–44. https://doi.org/10.1111/j.1540-8167.2008.01285.x.
Terasawa T, Balk EM, Chung M, Garlitski AC, Alsheikh-Ali AA, Lau J, Ip S. Systematic review: comparative effectiveness of radiofrequency catheter ablation for atrial fibrillation. Ann Intern Med. 2009;151(3):191–202. https://doi.org/10.7326/0003-4819-151-3-200908040-00131.
Morillo CA, Verma A, Connolly SJ, Kuck KH, Nair GM, Champagne J, … Natale A. Radiofrequency ablation vs antiarrhythmic drugs as first-line treatment of paroxysmal atrial fibrillation (RAAFT-2): a randomized trial. JAMA. 2014;311(7):692–700. https://doi.org/10.1001/jama.2014.467.
Haïssaguerre M, Jaïs P, Shah DC, Takahashi A, Hocini M, Quiniou G, … Clémenty J. Spontaneous Initiation of Atrial Fibrillation by Ectopic Beats Originating in the Pulmonary Veins. N Engl J Med. 1998;339(10), 659–666. https://doi.org/10.1056/NEJM199809033391003.
Luik A, Radzewitz A, Kieser M, Walter M, Bramlage P, Hörmann P, … Schmitt C. Cryoballoon versus open irrigated radiofrequency ablation in patients with paroxysmal atrial fibrillation: the prospective, randomized, controlled, noninferiority FreezeAF study. Circulation. 2015; 132(14), 1311–1319. https://doi.org/10.1161/CIRCULATIONAHA.115.016871.
Kuck K-H, Brugada J, Fürnkranz A, Metzner A, Ouyang F, Chun KRJ, … Tondo C. Cryoballoon or radiofrequency ablation for paroxysmal atrial fibrillation. N Engl J Med. 2016;374(23), 2235–2245. https://doi.org/10.1056/NEJMoa1602014.
Bourier F, Duchateau J, Vlachos K, Lam A, Martin CA, Takigawa M, … Jais P. High-power short-duration versus standard radiofrequency ablation: Insights on lesion metrics. J Cardiovasc Electrophysiol. 2018;29(11):1570–1575. https://doi.org/10.1111/jce.13724.
Nilsson B, Chen X, Pehrson S, Svendsen JH. The effectiveness of a high output/short duration radiofrequency current application technique in segmental pulmonary vein isolation for atrial fibrillation. Europace. 2006;8(11):962–5. https://doi.org/10.1093/europace/eul100.
Winkle RA, Mohanty S, Patrawala RA, Mead RH, Kong MH, Engel G, … Day JD. Low complication rates using high power (45–50 W) for short duration for atrial fibrillation ablations. Heart Rhythm. 2019; 16(2):165–169. https://doi.org/10.1016/j.hrthm.2018.11.031.
Bunch TJ, May HT, Bair TL, Crandall BG, Cutler MJ, Mallender C, … Day JD. Long-term outcomes after low power, slower movement versus high power, faster movement irrigated-tip catheter ablation for atrial fibrillation. Heart Rhythm. 2020;17(2):184–189. https://doi.org/10.1016/j.hrthm.2019.08.001.
Kotadia ID, Williams SE, O’Neill M. High-power, Short-duration Radiofrequency Ablation for the Treatment of AF. Arrhythm Electrophysiol Rev. 2020;8(4):265–72. https://doi.org/10.15420/aer.2019.09.
Chieng D, Segan L, Sugumar H, Al-Kaisey A, Hawson J, Moore BM, … Kistler PM. Higher power short duration vs. lower power longer duration posterior wall ablation for atrial fibrillation and oesophageal injury outcomes: a prospective multi-centre randomized controlled study (Hi-Lo HEAT trial). Europace. 2023;25(2):417–424. https://doi.org/10.1093/europace/euac190.
Francke A, Taha NS, Scharfe F, Schoen S, Wunderlich C, Christoph M. Procedural efficacy and safety of standardized, ablation index guided fixed 50 W high-power short-duration pulmonary vein isolation and substrate modification using the CLOSE protocol. J Cardiovasc Electrophysiol. 2021;32(9):2408–17. https://doi.org/10.1111/jce.15158.
Lee AC, Voskoboinik A, Cheung CC, Yogi S, Tseng ZH, Moss JD, … Gerstenfeld EP. A Randomized Trial of High vs Standard Power Radiofrequency Ablation for Pulmonary Vein Isolation: SHORT-AF. JACC Clin Electrophysiol. 2023;9(7 Pt 2):1038–1047. https://doi.org/10.1016/j.jacep.2022.12.020.
O’Neill L, El Haddad M, Berte B, Kobza R, Hilfiker G, Scherr D, … Duytschaever M. Very high-power ablation for contiguous pulmonary vein isolation: results from the randomized POWER PLUS trial. JACC Clin Electrophysiol. 2023;9(4):511–522. https://doi.org/10.1016/j.jacep.2022.10.039.
Shin DG, Ahn J, Han S-J, Lim HE. Efficacy of high-power and short-duration ablation in patients with atrial fibrillation: a prospective randomized controlled trial. Europace. 2020;22(10):1495–501. https://doi.org/10.1093/europace/euaa144.
Wielandts J-Y, Kyriakopoulou M, Almorad A, Hilfiker G, Strisciuglio T, Phlips T, … Knecht S. Prospective randomized evaluation of high power during CLOSE-guided pulmonary vein isolation: the POWER-AF study. Circ Arrhythm Electrophysiol. 2021;14(1):e009112. https://doi.org/10.1161/CIRCEP.120.009112.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, … Moher D. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Syst Rev. 2021;10(1):89. https://doi.org/10.1186/s13643-021-01626-4.
Higgins JPT TJ, Chandler J, Cumpston M, Li T, Page MJ, WV (editors). Cochrane Handbook for Systematic Reviews of Interventions. 2023.
Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, … Higgins JPT. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ (Clin Res ed.). 2019;366:l4898. https://doi.org/10.1136/bmj.l4898.
Guyatt GH, Oxman AD, Kunz R, Vist GE, Falck-Ytter Y, Schünemann HJ. What is “quality of evidence” and why is it important to clinicians? BMJ (Clin Res ed). 2008;336(7651):995–8. https://doi.org/10.1136/bmj.39490.551019.BE.
Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, Schünemann HJ. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ (Clin Res ed). 2008;336(7650):924–6. https://doi.org/10.1136/bmj.39489.470347.AD.
RevMan | Cochrane Training [Internet]. [cited 2021 Aug 3]. Available from: https://training.cochrane.org/online-learning/core-software-cochrane-reviews/revmanNo Title. (n.d.). Accessed 28 Sept 2023.
Hussein A, Das M, Riva S, Morgan M, Ronayne C, Sahni A, … Gupta D. Use of ablation index-guided ablation results in high rates of durable pulmonary vein isolation and freedom from arrhythmia in persistent atrial fibrillation patients: The PRAISE study results. Circ Arrhythm Electrophysiol. 2018;11(9):e006576. https://doi.org/10.1161/CIRCEP.118.006576.
Das M, Loveday JJ, Wynn GJ, Gomes S, Saeed Y, Bonnett LJ, … Gupta D. Ablation index, a novel marker of ablation lesion quality: prediction of pulmonary vein reconnection at repeat electrophysiology study and regional differences in target values. Europace. 2017;19(5):775–783. https://doi.org/10.1093/europace/euw105.
Calzolari V, De Mattia L, Indiani S, Crosato M, Furlanetto A, Licciardello C, … Olivari Z. In vitro validation of the lesion size index to predict lesion width and depth after irrigated radiofrequency ablation in a Porcine Model. JACC Clin Electrophysiol. 2017;3(10):1126–1135. https://doi.org/10.1016/j.jacep.2017.08.016.
Enomoto Y, Nakamura K, Ishii R, Toyoda Y, Asami M, Takagi T, … Nakamura M. Lesion size and adjacent tissue damage assessment with high power and short duration radiofrequency ablation: comparison to conventional radiofrequency ablation power setting. Heart Vessels. 2021;36(9):1438–1444. https://doi.org/10.1007/s00380-021-01833-y.
Chavez P, Messerli FH, Dominguez AC, Aziz EF, Sichrovsky T, Garcia D, … Danik S. Atrioesophageal fistula following ablation procedures for atrial fibrillation: systematic review of case reports. Open Heart. 2015;2(1):e000257. https://doi.org/10.1136/openhrt-2015-000257.
Kapur S, Barbhaiya C, Deneke T, Michaud GF. Esophageal Injury and Atrioesophageal Fistula Caused by Ablation for Atrial Fibrillation. Circulation. 2017;136(13):1247–55. https://doi.org/10.1161/CIRCULATIONAHA.117.025827.
Cappato R, Calkins H, Chen S-A, Davies W, Iesaka Y, Kalman J, … Skanes A. Prevalence and causes of fatal outcome in catheter ablation of atrial fibrillation. J Am College Cardiol. 2009;53(19):1798–1803. https://doi.org/10.1016/j.jacc.2009.02.022.
Vassallo F, Cunha C, Serpa E, Meigre LL, Carloni H, Simoes AJ, … Serpa R. Comparison of high-power short-duration (HPSD) ablation of atrial fibrillation using a contact force-sensing catheter and conventional technique: Initial results. J Cardiovasc Electrophysiol. 2019;30(10):1877–1883. https://doi.org/10.1111/jce.14110.
Dhillon G, Ahsan S, Honarbakhsh S, Lim W, Baca M, Graham A, … Hunter RJ. A multicentered evaluation of ablation at higher power guided by ablation index: Establishing ablation targets for pulmonary vein isolation. J Cardiovasc Electrophysiol. 2019;30(3):357–365. https://doi.org/10.1111/jce.13813.
Chen S, Chun KRJ, Tohoku S, Bordignon S, Urbanek L, Willems F, … Schmidt B. Esophageal endoscopy after catheter ablation of atrial fibrillation using ablation-index guided high-power: Frankfurt AI-HP ESO-I. JACC Clin Electrophysiol. 2020;6(10):1253–1261. https://doi.org/10.1016/j.jacep.2020.05.022.
Müller J, Berkovitz A, Halbfass P, Nentwich K, Ene E, Sonne K, … Deneke T. Acute oesophageal safety of high-power short duration with 50 W for atrial fibrillation ablation. Europace. 2022;24(6):928–937. https://doi.org/10.1093/europace/euab329.
Ravi V, Poudyal A, Abid Q-U-A, Larsen T, Krishnan K, Sharma PS, … Huang HD. High-power short duration vs. conventional radiofrequency ablation of atrial fibrillation: a systematic review and meta-analysis. Europace. 2021;23(5):710–721. https://doi.org/10.1093/europace/euaa327.
Funding
Open access funding provided by The Science, Technology & Innovation Funding Authority (STDF) in cooperation with The Egyptian Knowledge Bank (EKB). We received no funding for this study.
Author information
Authors and Affiliations
Contributions
A.M.A. conceived the idea. A.M.A. and M.A. designed the research workflow. A.M.A. and M.A. searched the databases. M.A.A, O.A., and A.A. screened the retrieved records, extracted relevant data, assessed the quality of evidence, and B.A. resolved the conflicts. A.M.A. and A.A.I. performed the analysis. A.M.A., R.G., and M.A. wrote the final manuscript. B.A. supervised the project. All authors have read and agreed to the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Conflicts of interest
The authors declare no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Amin, A.M., Ghaly, R., Ibrahim, A.A. et al. Efficacy and safety of high-power short-duration ablation for atrial fibrillation: a systematic review and meta-analysis of randomized controlled trials. J Interv Card Electrophysiol (2024). https://doi.org/10.1007/s10840-024-01782-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10840-024-01782-2