Abstract
Background
The strategy of cardiac implantable electronic device (CIED) implantations performed as day-case admissions has gained a wider acceptance overtime; however, data on safety are still limited. This study aims to investigate the safety of a same-day discharge protocol introduced in our hospital for the postprocedural management of patients undergoing CIED implantation.
Methods
Α prospective, non-interventional, non-randomised study performed in a single high-volume implanting centre for a 16-month period (March 2020 to June 2021). At total of 821 of 965 (85.1%) patients scheduled for elective CIED implantation were considered to be eligible for inclusion in the Short-stay Device Management Protocol. These patients were compared with a historical group of 932 patients, meeting the same inclusion criteria.
Results
Procedure was successful in 812 patients (98.9%), committed to same-day discharge versus 921 of 932 patients (98.8%) admitted for overnight stay (p = 0.87). Overall, 90-day complication rate was comparable in both groups (4.14% vs 4.07%, p = 0.95), as was major (1.46% vs. 1.82%, p = 0.55) and minor (2.67% vs. 2.25%, p = 0.64) complication rates. The composite early post-procedural complication rates and late post-procedural complication rates were comparable among groups (0.97 vs 1.18%, p = 0.70 and 0.73% vs 0.64%, p = 0.83, respectively). Six hundred sixty-seven patients (84%) preferred the same-day discharge strategy. Finally, a reduction of 792 bed-days was recorded, resulting in possible financial Health System benefits.
Conclusions
Same-day discharge is feasible and safe in the majority of patients referred for CIED implantation. Additionally, same-day discharge is preferred by patients and may reduce procedure-related costs due to significant bed-day reductions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Implantation of cardiac implantable electronic devices (CIED) has increased significantly in the last two decades worldwide as a result of technological improvement, expansion in indications, experience, and ageing of population [1,2,3]. Despite these achievements, CIED therapy may still be associated with significant peri- and/or post-procedural complications. Major and minor complications rates vary considerably among different studies ranging between 4 and 12% with most of them occurring during the early post-implantation period [3,4,5,6,7,8,9,10,11]. In order to minimise complication risk and maximise safety, CIED implantations were followed by an overnight in-hospital stay as a standard practice in most institutions including our hospital.
On the other hand, a number of previous studies, most of which were non-randomised, demonstrated that early mobilisation and same-day discharge is safe, does not add to the complication rate, and reduces procedure-related costs [12,13,14,15,16,17,18,19,20,21].Two subsequent surveys in 2014 and 2021, organised by the European Heart Rhythm Association (EHRA), showed that implantations were performed as day-case admissions in 30% and 50%, respectively, indicating a wider acceptance of this strategy overtime; however, the optimal management protocol remains a matter of debate [22, 23].
In our institution, non-urgent procedures were temporarily suspended on September 2020, as a result of the COVID-19 pandemic, in order to minimise exposure to the corona-virus, prioritising bed utilisation by the increased number of COVID-19 patients and preserve human and material resources. In our department, we introduced a novel short-stay, same-day discharge protocol for the postprocedural management of patients for whom CIED implantation or generator replacement was absolutely necessary.
In the present manuscript, we report our experience with this strategy in carefully selected patients. Our aim was to investigate whether this change in clinical practice, albeit introduced under the urgent and unexpected conditions of the pandemic, is safe to be adopted in the long term. In addition, we aimed to evaluate patient satisfaction/anxiety, resulting from hospital practice change.
2 Material and methods
2.1 Study design and patient population
This prospective, non-interventional, non-randomised, open-label, study was performed in a single high-volume device implanting centre in Greece, for a 16-month period, between March 2020 and June 2021.
All adult patients referred for a CIED implantation or generator replacement, either electively or urgently, were assessed with regard to the possibility of being included in a novel Short-stay Device Management Protocol introduced in our hospital due to the pandemic circumstances. Exclusion criteria for participation in the study were as follows: (a) pacemaker-dependent patients, (b) those with mechanical prosthetic valves under oral anticoagulation therapy, (c) patients with atrial fibrillation receiving anticoagulation therapy and a high-risk for thromboembolic events, (d) patients with a prior history of pulmonary embolism, (e) individuals with a previous history of venous thromboembolism other than pulmonary embolism and a high risk for a recurrent episode, (f) haemodynamically unstable patients, and (g) patients with any other life-threatening co-morbidity or systematic disease that could potentially compromise their safety. Exclusion criteria are further analysed in Table 1.
Individuals with an indication for CIED implantation or generator replacement were informed about the changes in patient management practice introduced in our institution under the circumstances of the pandemic, prior to the intervention. Moreover, they consented to allow access in their medical records for study purposes. At baseline, demographic data, medical history, indication for new implantation, type of device, and additional clinical data were recorded. A scheduled visit at the cardiology device outpatient department of our hospital was performed 24-h post-implantation, and subsequently 1 week, 1 month, and 3 months post-implantation. At each visit, the clinical status and pacing parameters of the device were recorded. Unscheduled visits were also possible according to symptoms. Moreover, urgent or elective hospital-readmissions were decided on a case-by-case basis according to the clinical findings.
The main endpoints of the study were the presence of major periprocedural complications, assessed during hospital short-stay; early post-procedural complications, assessed during 24-h and 1-week visits and late post-procedural complications; and assessed during 1-month and 3-montjh visits. Secondary endpoint was identification of a minor implantation–related complication, during assessment at the same monitoring periods.
In the present study, we compared the results of the prospectively observed patient group (Group A) with data from a historical cohort of adult patients who underwent CIED implantation or generator replacement from 1 March 2018 to 30 June 2019 (Group B) according to the Standard-stay Device Management Protocol, before the onset of the COVID-19 pandemic. Group B patient data were retrospectively analysed after applying similar exclusion criteria.
Patients’ demographics and co-morbidities, such as the presence of arterial hypertension, diabetes mellitus, dyslipidaemia, established cerebrovascular, or coronary artery disease and atrial fibrillation, were systematically recorded.
2.2 Standard-stay device management protocol
In the pre-COVID-19 pandemic era, patients scheduled for elective CIED implantation or generator replacement as well as uncomplicated patients admitted through the Emergency Department requiring CIED implantation were committed to a single overnight hospital stay. Subsequently, patients were discharged in the next morning provided that general clinical status including the implantation site, pacing parameters, and results from 12-lead electrocardiogram (ECG) were satisfactory. In the case of the occurrence of a complication, hospital stay was extended accordingly.
2.3 Short-stay device management protocol
Implantations were performed in the electrophysiology lab with local anaesthesia solely, without using additional intravenous sedation. Antibiotic prophylaxis was performed, similar to patients who underwent an overnight stay in the hospital, by means of a single vancomycin dose of 1 g (or 1.5 g for patients with body weight of more than 80 kg). Infusion was started 60 to 120 min before implantation and continued at a recommended rate of 1 g per hour (or 1.5 g over 90 min). All procedures were performed according to the standard practice for CIED implantation or CIED generator replacement.
Directly after the device implantation/generator replacement, patients who had a periprocedural complication or those requiring extended clinical observation, cardiac monitoring, or additional treatment were identified and admitted. The remaining patients were observed for 1 h after undergoing generator replacement and 2 h after pacemaker implantation, implantable cardioverter defibrillator (ICD) implantation, or biventicular pacemaker implantation. Monitoring occurred without continuous electrocardiographic monitoring, in a dedicated area of the cardiac catheterisation and electrophysiology laboratory. Patients were ambulated progressively within the first hour post-intervention.
Subsequently, a formal triage was performed to determine whether the patient was deemed suitable for early discharge. In the absence of symptoms or ECG changes, absence of abnormalities at the implantation site, and adequate pacing and sensing parameters, the patient was discharged. Oral analgesics, such as paracetamol, were prescribed for pain control in these patients.
Patients not fulfilling these prerequisites were transferred to the overnight stay facilities and were discharged the next day or later in the event of subsequent complications. Figure 1 summarises the patient management procedure following the Overnight-Stay and the Short-Stay Device Management Protocol.
2.4 Definitions
“CIED implantations” included patients scheduled for single- or dual-chamber pacemaker, single- or dual-chamber ICD, or biventricular pacemaker or ICD implantations.
In the present study, we included the following incidences in the “major complications” category: cardiac perforation; pericardial tamponade; life threatening haemothorax or pneumothorax requiring intervention; pocket hematoma requiring evacuation; pacing system and/or pocket infection; tricuspid valve damage; thromboembolism including peripheral embolism or cerebrovascular accident; deep vein thrombosis; lead dislodgement; sensing failure; failure to capture due to lead fracture; insulation problems etc.; and death related to implantation procedure.
In addition, the following complications were classified as “minor”: haemothorax or pneumothorax not-requiring intervention, small wound hematomas not requiring evacuation, sustained non-life-threatening arrhythmias such as atrial fibrillation peri-procedurally, wound healing problems without signs of infection, increase in pacing threshold, or decrease in P or R wave sensing not requiring revision.
2.5 Ethical considerations
The study was approved by the hospital ethics committee and was conducted in accordance with the principles of the 1964 Helsinki declaration and its later amendments. Participants provided written informed consent prior to enrolment in the study. All personal data stored in electronic and hard-copy forms were pseudonymised. The study was approved by the “Scientific Council,” the local committee responsible for reviewing study protocols introduced in our hospital.
2.6 Patient satisfaction and preference
To measure patient satisfaction with same-day discharge compared to discharge following an overnight stay, an anonymous, standardised questionnaire consisting of 16 questions was provided to patients during their outpatient visit, 1-week post-implantation by the outpatient clinic nurse (Supplementary Fig. 1).
Patients’ perception was validated at the following fields: (a) adequacy of information received regarding treatment, (b) attendance of the medical and nursing staff during their hospital short-stay, (c) quality of the discharge procedure, and (d) the psychological status in the first 24 h and first week post implantation. In addition, the patients’ preference, regarding the implantation management strategy, was assessed.
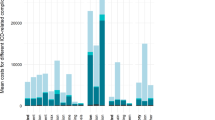
2.7 Possible impact on the cost
Hospital charges paid by health insurance funds remain constant at the specific Health System at which the present study was conducted. Therefore, a possible financial impact may be assumed, in the case that the change in our practice results in an overall reduction in hospital stay. Adopting this assumption, in the present study, we sought to calculate the reduction in hospital bed-days resulting from same-day discharge.
2.8 Statistical analysis
Shapiro–Wilk test and p-p plots were used to evaluate normality of variable distribution. Accordingly, continuous variables were expressed as mean ± standard deviation. Categorical variables were expressed as valid percentages. To test for differences in continuous variables between the two study groups, t-test was applied. Contingency tables and chi square test were used to test for differences in frequency of categorical variables among the two studied groups. All reported P values were based on two-sided hypotheses. A P value of < 0.05 was considered statistically significant. All statistical calculations were performed using SPSS software (version 25.0; SPSS Inc., Chicago, Illinois, USA) and Graph Pad prism version 6.
3 Results
3.1 Patients
During the 16-month enrolment period (1 March 2020 to 30 June 2021), a total of 965 CIED implantations and generator replacements were performed in our centre (60.3 procedures/ month). Of the 965 patients, 821 (85.1%) were considered to be eligible for same-day discharge post-procedure (Fig. 1). The mean age of this population (Group A) was 75.9 ± 10.1 years, and 329 patients (40.1%) were female.
Patient demographics and clinical and procedural characteristics were compared with a historical group (Group B) of 932 of the 1079 patients, who underwent CIED implantations and generator replacements during a 16-month period (1 March 2018 to 30 June 2019), and would have been eligible for early discharge, according to the exclusion criteria of the study. During this period, the overall implantation rate was 67.4 procedures/month. Patient data are shown in Table 2, and were well balanced between the two groups. No gender-based differences were present. Specifically, there was no difference between Groups A and B in age (75.9 ± 10.1 years vs. 76.8 ± 10.5 years, p = 0.07), female sex (40.1% vs. 42.1%, p = 0.71), and other potential confounders or risk factors (Supplementary Fig. 2).
Group A population included 148 generator replacement procedures, 511 pacemaker implantations (412 of which were dual chamber and 99 single chamber), 93 ICD implantations (84 of which were dual chamber and 9 single chamber), and 69 biventricular system implantations (15 pacemaker systems and 54 defibrillator systems), representing 18.0%, 62.3%, 11.3%, and 8.4% of the total procedures performed in the same time period. On the other hand, in Group B, indication for the procedure was generator replacement in 159 cases, pacemaker implantation in 564 cases (459 of which were dual chamber and 105 single chamber), ICD implantation in 104 cases (96 of which were dual chamber and 8 single chamber), and biventricular system implantation in 105 cases (24 pacemaker systems and 81 defibrillator systems), comprising 17.1%, 60.5%, 11.2%, and 11.3% of the overall number of procedures performed during that time interval. Importantly, between Group A and Group B, there was no difference according to type of procedure (p = 0.61).Active fixation atrial and ventricular leads were used in all implantation procedures, in both patients of Groups A and B. On the other hand, passive fixation left ventricular leads were used in all patients requiring cardiac resynchronisation therapy (CRT).
3.2 Procedural success, postprocedural observation, and discharge
Procedure was successful in 812 of 821 patients (98.9%), committed to same-day discharge versus 921 of 932 patients (98.8%) admitted for overnight stay (p = 0.87). In 4 of the 9 unsuccessful cases in Group A and in 5 of 11 unsuccessful cases in Group B, failure was due to failed coronary sinus catheterisation in patients with an indication for biventricular system implantation. In the remaining 5 and 6 unsuccessful cases in Groups A and B respectively, failure was due to severe venous access problems. In these cases, implantation of leadless pacing systems was performed in 10 patients (5 of Group A and 5 of Group B) and implantation of a subcutaneous ICD system was performed in 1 patient in Group B.
3.3 Periprocedural complications, patient observation, and discharge
During the observation period, another 20 patients scheduled to same-day discharge developed an indication for extended hospital stay and were admitted to hospital, in addition to the 9 patients in which implantation was unsuccessful. On the basis of the formal triage after the observation time-period, 96.5% of patients (792 of 821) scheduled to same-day discharge was, indeed, considered suitable for immediate discharge. Thus, overall, during the 16-month study period, 792 of 965 patients (82.1%) referred to our department for a new pacemaker implantation or generator replacement were eventually managed as day-cases.
During the periprocedural period, no death was recorded. Only 20 of 821 patients (2.43%) experienced a total of 20 significant complications, 7 of which were classified as major (e.g. 5 lead dislodgments requiring revision and 2 ventricular perforations) and 13 were considered to be minor (e.g. 8 pocket hematomas, 3 vasovagal episodes, and 2 episodes of pneumothorax not requiring intervention) (Table 3; Supplementary Fig. 3).
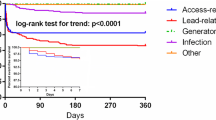
3.4 Complications and follow-up
Tables 3 and 4 and Supplementary Fig. 4 show the occurrence of the various clinical events specified by time of occurrence. No death directly related to pacemaker implantation was recorded in the same-day discharge group within the first 3 months post-procedure. In the overnight-stay group, also none of the patients died during the early post-procedural period; however, one patient died due to acute cerebrovascular accident, and another patient due to heart failure deterioration, during the 3-month follow-up period.
During or immediately after intervention, 20 of 821 patients (2.43%) in the same-day discharge group manifested an acute complication, as did 21 of 932 patients (2.25%) of the overnight-stay group (p = 0.80). Only 5 complications were recorded during the assessment, 24 h post procedure (0.61%) in the 821 patients of Group A versus 7 complications in the 932 patients of Group B (0.75%) (p = 0.72). During assessment on 1-week, 1-month, and 3-month visits, the presence of a pacing-related complication was revealed in 3 (0.36%), 2 (0.24%), and 4 (0.48%) of the 821 patients of same-day discharge group respectively, as was in 4 (0.43%), 2 (0.21%), and 4 (0.43%) of the 932 patients of the overnight-stay group (p = ns for all). Three-month follow-up was completed for all patients.
The overall 90-day complication rate was comparable in both groups (4.14% in Group A vs 4.07% in Group B, p = 0.95), as was the major and minor complication rate (major complication: 1.46% vs. 1.82%, p = 0.55, and minor complication: 2.67% vs. 2.25%, p = 0.64, for Group A and Group B, respectively). Finally, the composite early post-procedural (assessed during 24-h and 1-week visits) complication rates were comparable among same-day discharge group and overnight-stay group (0.97 vs 1.18%, p = 0.70) as were the composite late post-procedural (assessed during 1-month and 3-month visits) complication rates (0.73% in Group A vs 0.64% in Group B, p = 0.83).
No unscheduled readmission was required in the same-day discharge patient group, after the 24-h outpatient visit assessment. However, 2 readmissions were performed (one due to lead dislodgment and one due to capture failure) after 1st week assessment, whereas 3 admissions were performed (one due to lead fracture and 2 due to pacing system infection) after the 3-month assessment. In the overnight-stay group, two patients were readmitted after the 1st week assessment (due to lead fracture), 2 after 1st month assessment (one due to lead dislodgment and one due to pacing system infection), and another 2 after the 3-month assessment (due to pacing system infection) (Table 3).
Lead dislodgment, occurring in the periprocedural or early-postprocedural period, was the most frequent major complication in both study groups, recognised in 0.73% of the cases in Group A and 0.85% of the cases in Group B (p = 0.98). Two patients in Group A and 2 patients in Group B (p = 0.90) developed myocardial perforation with mild pericardial effusions, without progression to cardiac tamponade and without requirement for surgical intervention, albeit resulting in extended hospitalisation. Ten patients in Group A (1.22%) developed mild to moderate pocket haematomas, whereas this complication occurred in 9 patients in Group B (0.96%), 2 of which required re-intervention for haematoma evacuation (p = 0.61). Lead fracture occurred in two patients in Group A and also in two patients in Group B (p = 0.90). In an additional 0.85% (n = 7) and 0.96% (n = 9) in Groups A and B respectively (p = 0.80), an increase in pacing threshold was observed, without the need for lead revision. A pneumothorax was detected in 2 cases in the same-day discharge group (0.24%) as was in 3 cases in the overnight-stay group (0.32%) (p = 0.74), however without requiring intervention. Finally, pacing system and/or pocket infection occurring as a late complication was detected in 2 (0.24%) and 3 (0.32%) patients in Groups A and B respectively (p = 0.76).
3.5 Patient Satisfaction
All 792 patients, eventually discharged on the same day completed the Patient Satisfaction and Preference Questionnaire during their visit at Outpatient Department, 1 week post procedure (Supplementary Fig. 1). Six hundred eighty-nine patients (87%) characterised information received regarding their treatment as “adequate” (vs 5% who thought that it was “inadequate” and 8% who were not sure), 728 patients (92%) scored attendance of the medical and nursing staff during their hospital short-stay as “adequate” (vs 7% characterising it as “inadequate” and 1% not being sure), and 626 patients (79%) were satisfied with the discharge procedure (vs 11% who were “not satisfied” and 10% who were not sure). Six hundred sixty-seven patients (84%) answered that they preferred to be discharged on the same day over overnight-stay (vs 16% wishing an overnight-stay). Finally, 571 patients (72%) answered that they had no anxiety on the first 24-h post procedure (vs 19% reporting anxiety on the first 24 h and 9% not being sure) (Supplementary Fig. 5).
4 Cost
Eventually, 792 patients avoided an overnight stay in the hospital, and therefore, a reduction of 792 bed-days may be assumed, resulting in a potential significant financial benefit for the Health System, due to the reduction in hospital stay.
5 Discussion
Despite the significant technological improvements and the accumulated experience due to the increasing implantation rates of CIEDs in the European countries [24], complication rate is still considered to be non-neglectable. As in most other institutions, in our clinic, the current standard of care, for patients who undergo uncomplicated CIED implantations or generator replacements, either elective or urgent, is an overnight in-hospital stay. This approach is followed to overcome concerns regarding lead dislodgement or other major complications becoming evident in the first hours post-implantation. Access site complications (i.e. hematomas.) is also of concern, while overnight stay may be essential for management of comorbidities, such as renal insufficiency, diabetes, arterial hypertension, and congestive heart failure (CHF).
Nevertheless, the present study demonstrates that same-day discharge after elective or urgent CIED implantation or generator replacement can be performed safely in the vast majority of the patients. Following introduction of the novel protocol in our practice, 96.5% of patients scheduled to same-day discharge and 82.1% of the total number of patients referred to our department were eventually successfully managed as day-cases. The protocol identifies a few exclusion criteria, based on the clinical characteristics of the patients, that should be thoroughly applied. In same-day discharge group, the overall 90-day complication rate was found to be 4.14%, consistent with previous studies [4,5,6,7,8,9,10,11, 25]. Moreover, the overall 90-day complication rate was similar to that revealed at the overnight-stay group (4.07%). In addition, there were no significant differences among the two groups with regard to the rates of periprocedural, early-postprocedural, and late-postprocedural complications (Tables 3 and 4). Furthermore, major and minor complications rates were comparable among groups.
Therefore, according to our results, one may be reasonably confident that the 2 strategies do not lead to substantially different outcomes. Despite the fact that same-day discharge protocol was adopted in order to preserve an adequate number of beds in anticipation of a possible surge in COVID-19 cases as well as to reduce possible patient exposure to the virus, these data show safety and feasibility of this strategy and indicate that it could, potentially, be adopted as a standard clinical practice in the post-COVID-19 era.
Another important finding was that same-day discharge after CIED implantation or generator replacement did not lead to unexpected cardiac events or to an excess of implantation site complications. In our study, careful peri-procedural monitoring followed by a maximum 2-h observation period allowed adequate triage of patients to same-day discharge or alternatively to admission and a more extended clinical observation. Early mobilisation during the first hour post-procedurally was safe and feasible and did not lead to additional complications.
Our study shows that patients at risk for postprocedural complications can be identified effectively in a day-case setting on the basis of predefined clinical criteria. Moreover, a definitive decision for same-day discharge can be made only after an uncomplicated clinical course of maximum 2 h, depending on the type of the intervention. Patients should be adequately selected for additional observation to anticipate postprocedural complications.
The concept of day-case CIED implantations was first proposed over 30 years ago [12, 13]; however, evidence regarding the safety of this strategy is still limited. Previous studies demonstrated that early ambulation and short-term observation after CIED implantation is safe and does not result in an increased complication rate [14,15,16,17,18,19,20,21]. Although these data originating from large-scale registries and non-randomised studies suggest that most patients can be discharged safely within 24 h of successful CIED implantation [15, 17,18,19], evidence from large-scale, randomised controlled studies is limited. On the other hand, available prospective, controlled studies, although recruiting a relatively small number of patients, have also demonstrated no significant difference in the rate of complications between inpatient and same-day discharge groups [14, 16, 20, 21]. Our results are in line with these findings data, showing safety of early mobilisation and same-day discharge, post CIED implantation. Complication rates in these studies were not increased in the same-day discharge patient group and were comparable to those reported in the literature. On the other hand, other authors remain sceptical, suggesting that since many complications occur during the early post-implantation period, it might not be optimal to discharge patients in ≤ 24 h [23].
According to the results of a European Heart Rhythm Association (EHRA) survey published in 2014, elective device implantations were performed by the participating centres as day-case admissions in 30%, with a single overnight stay in 47%, with two-night admissions in 13%, and with more than two-night admissions in 10% [22]. However, a more recent EHRA survey published in 2021 demonstrated a significant shift in the clinical practice towards same-day discharge, since approximately 50% of respondents already implement this strategy at their institutions following implantations of pacemakers with one or two intracardiac leads [26]. Our study provides additional evidence towards this direction, showing that, currently, a change in clinical practice is reasonable and may be justified by procedural outcomes.
Another finding of the present study is a significant decrease in CIED implantations during the COVID-19 pandemic, from 67.4 procedures/month to 60.3 procedures/month. This reduction by 10.5% may however have happened due to various other factors as well. Nevertheless, these findings are consistent with reports from various other countries [27,28,29,30].
A reduction in hospital stays and the application of day-case facilities were shown to reduce procedure-related costs. In the present study, same-day discharge led in a potential cost reduction, due to the reduction of cost paid by the insurance funds to the hospital for bed. Therefore, a potential change in the strategy of CIED implantations management might result in substantial financial resources savings for the health system.
Finally, 84% of the patients reported a preference for a same-day discharge strategy. Moreover, the vast majority of the patients was very satisfied for avoiding hospitalisation, especially in the COVID-19 era, and demonstrated relatively low rates of anxiety and feeling unsecure after early discharge.
This prospective study provides additional evidence on the safety of short-stay CIED implantation; however, lack of randomisation, observational, and single-centre design limit the generalisation of our findings. Furthermore, our hospital is a relatively high-volume centre and implantations were performed by highly experienced implanting physicians, and therefore, results may not be generalised and extrapolated to low-volume settings. Third, in order to determine effectiveness and safety of the novel protocol in a real-world setting, we compared prospectively collected data with findings obtained retrospectively, by a recent historical cohort. Fourth, patient exclusion both in Group A and in Group B might have been influenced by selection bias. The decision to enrol a patient at the same-day discharge protocol is clinical, and therefore, there might be a tension to include lower-risk patients in this group. Fifth, the conditions during the COVID pandemic may not be exactly comparable to the historical controls. For example, factors such as community infection rates would be expected to be higher, whereas masking and social isolation might lower risk and increase patient acceptance of recovery at home. Finally, the selection of the exclusion criteria involves a degree of arbitrariness. The definition of the category of patients unsuitable for same-day discharge should undergo extensive validation.
6 Conclusion
Taking into account the study limitations, and especially the fact that this is a non-randomised study, the control group of which is studied retrospectively, we may however conclude that same-day discharge is feasible and safe in the majority of patients referred for CIED implantation or generator replacement. Early patient mobilisation and same-day discharge does not lead to additional complications compared with overnight stay. Additionally, our data indicate that a change in every-day clinical practice towards managing these patients as day-cases is preferred by the patients, increasing the level of their satisfaction, and may be cost-effective for health-care systems, due to the reduction in hospital bed-days. A randomised, multicentre study will probably further establish the utility of this strategy.
Change history
21 December 2022
A Correction to this paper has been published: https://doi.org/10.1007/s10840-022-01458-9
References
Greenspon AJ, Patel JD, Lau E, et al. Trends in permanent pacemaker implantation in the United States from 1993 to 2009: increasing complexity of patients and procedures. J Am Coll Cardiol. 2012;60:1540–5.
Raatikainen MJ, Arnar DO, Merkely B, et al. Access to and clinical use of cardiac implantable electronic devices and interventional electrophysiological procedures in the European Society of Cardiology Countries: 2016 Report from the European Heart Rhythm Association. Europace. 2016;18Suppl3:iii1-iii79.
Brignole M, Auricchio A, Baron-Esquivias G, et al. 2013 ESC Guidelines on cardiac pacing and cardiac resynchronization therapy: the Task Force on cardiac pacing and resynchronization therapy of the European Society of Cardiology (ESC). Developed in collaboration with the European Heart Rhythm Association (EHRA). Eur Heart J.2013;34:22812329.
Udo EO, Zuithoff NP, van Hemel NM, et al. Incidence and predictors of short- and long-term complications in pacemaker therapy: the FOLLOWPACE study. Heart Rhythm. 2012;95:728–35.
Kiviniemi MS, Pirnes MA, Eränen HJ, et al. Complications related to permanent pacemaker therapy. Pacing Clin Electrophysiol. 1999;22:711–20.
Kirkfeldt RE, Johansen JB, Nohr EA, et al. Complications after cardiac implantable electronic device implantations: an analysis of a complete, nationwide cohort in Denmark. Eur Heart J. 2014;35:1186–94.
van Rees JB, de Bie MK, Thijssen J, et al. Implantation-related complications of implantable cardioverter-defibrillators and cardiac resynchronization therapy devices: a systematic review of randomized clinical trials. J Am Coll Cardiol. 2011;58:995–1000.
Klug D, Balde M, Pavin D, et al. Risk factors related to infections of implanted pacemakers and cardioverter-defibrillators: results of a large prospective study. Circulation. 2007;116:1349–55.
Johansen JB, Jørgensen OD, Møller M, et al. Infection after pacemaker implantation: infection rates and risk factors associated with infection in a population-based cohort study of 46299 consecutive patients. Eur Heart J. 2011;328:991–8.
Poole JE, Gleva MJ, Mela T, et al. Complication rates associatedwith pacemaker or implantable cardioverter-defibrillatorgenerator replacements and upgrade procedures: resultsfrom the REPLACE registry. Circulation. 2010;122:1553–61.
Fanourgiakis J, Simantirakis E, Maniadakis N, et al. Complications related to cardiac rhythm management device therapy and their financial implication: a prospective single-center two year survey. Hellenic J Cardiol. 2016;57:33–8.
Haywood GA, Camm AJ, Ward DE. Insertion of permanent pacemakers as a day case procedure BMJ. 1989;299:1139.
Haywood GA, Jones SM, Camm AJ, et al. Day case permanent pacing. Pacing Clin Electrophysiol. 1991;14:773–7.
Miracapillo G, Costoli A, Addonisio L, et al. Early mobilization after pacemaker implantation. J Cardiovasc Med (Hagerstown). 2006;7:197–202.
Villalba S, Roda J, Quesada A, et al. Retrospective study of patients who undergo pacemaker implantation in short-stay ambulatory surgery. Long-term follow-up and cost analysis. Rev EspCardiol. 2004;57:234–40.
Choudhuri I, Desai D, Walburg J, et al. Feasibility of early discharge after implantable cardioverter-defibrillator procedures. J Cardiovasc Electrophysiol. 2012;23:1123–9.
Darda S, Khouri Y, Gorges R, et al. Feasibility and safety of same-day discharge after implantable cardioverter defibrillator placement for primary prevention. Pacing Clin Electrophysiol. 2013;36:885–91.
Atherton G, McAloon CJ, Chohan B, et al. Safety and cost-effectiveness of same-day cardiac resynchronization therapy and implantable cardioverter defibrillator implantation. Am J Cardiol. 2016;117:1488–93.
Spitzer SG, Andresen D, Kuck KH, et al. Long-term outcomes after event-free cardioverter defibrillator implantation: comparison between patients discharged within 24 h and routinely hospitalized patients in the German DEVICE registry. Europace. 2017;19:968–75.
Peplow J, Randall E, Campbell-Cole C, et al. Day-case device implantation—a prospective single-center experience including patient satisfaction data. Pacing Clin Electrophysiol. 2018;41:546–52.
Budano C, Garrone P, Castagno D, et al. Same-day CIED implantation and discharge: is it possible? The E-MOTION trial (Early MObilization after pacemaker implantaTION). Int J Cardiol. 2019;288:82–6.
Todd D, Bongiorni MG, Hernandez-Madrid A, et al. Scientific Initiative Committee, European Heart Rhythm Association. Standards for device implantation and follow-up: personnel, equipment, and facilities: results of the European Heart Rhythm Association Survey. Europace. 2014;16:1236–9.
Ohlow MA, Awada H, Laubscher M, et al. Very early discharge after cardiac implantable electronic device implantations: is this the future? J Interv Card Electrophysiol. 2021;60:231–7.
Raatikainen MJ, Arnar DO, Merkely B, et al. Access to and clinical use of cardiac implantable electronic devices and interventional electrophysiological procedures in the European Society of Cardiology Countries: 2016 Report from the European Heart Rhythm Association. Europace. 2016;18Suppl 3:iii1-iii79.
Sideris S, Trachanas K, KelesidisI, et al. Cardiac resynchronization therapy: a review of pathophysiology and clinical applications. Hellenic J Cardiol. 2015;56:451–60.
König S, Svetlosak M, Grabowski M, et al. Utilization and perception of same-day discharge in electrophysiological procedures and device implantations: an EHRA survey. Europace. 2021;23:149–56.
Aranda RS, Castellano NP, Pérez OC, et al. Domínguez. Impact of the first wave of the SARS-CoV-2 pandemic on preferential/emergent pacemaker implantation rate. Spanish study Rev EspCardiol. 2021;74:469–72.
Leyva F, Zegard A, Okafor O, et al. Cardiac operations and interventions during the COVID-19 pandemic: a nationwide perspective. Europace. 2021;23:928–36.
Fersia O, Bryant S, Nicholson R, et al. The impact of the COVID-19 pandemic on cardiology services. Open Heart. 2020;7:e001359.
Gonzales-Luna AC, Torres-Valencia JO, Alarcón-Santos JE, et al. Impact of COVID-19 on pacemaker implant. J Arrhythm. 2020;36:845–8.
Author information
Authors and Affiliations
Contributions
Dr Skevos Sideris is the main investigator of the study; responsible for the conception, organisation, and supervision of the study; and for the final approval of the manuscript submitted. Dr Stefanos Archontakis participated in study design, data analysis and interpretation, and manuscript drafting. Dr Evangelos Oikonomouand Dr Emmanouil Charitakis did the statistical analysis. Dr Konstantinos Sideris, Dr Ageliki Laina, Dr Dimitra Tirovola, and Dr Dimitra Paraskeuopoulou participated in manuscript drafting. Dr Panagiotis Kostakis and Dr Ioannis Doudoulakis participated in literature revision. Dr Petros Arsenos and Dr Ioannis Ntalakouras participated in data collection and patients’ follow-up. Prof Konstantinos Gatzoulis (Director of the EP Laboratory) and Prof Konstantinos Tsioufis (Director of the Cardiology Department) reviewed the manuscript, supervised the study, and also approved the manuscript submitted.
Corresponding author
Ethics declarations
Ethical approval
The study was approved by the hospital ethics committee and was conducted in accordance with the principles of the 1964 Helsinki declaration and its later amendments.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: In this article the author name Evangelos Oikonomou was incorrectly written as Evangelos K. Oikonomou.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Archontakis, S., Oikonomou, E., Sideris, K. et al. Safety of same-day discharge versus overnight stay strategy following cardiac device implantations: a high-volume single-centre experience. J Interv Card Electrophysiol 66, 471–481 (2023). https://doi.org/10.1007/s10840-022-01319-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10840-022-01319-5