Abstract
Purpose
This study is aimed to evaluate the impact of catheter contact angle on lesion formation and durability of pulmonary vein isolation (PVI).
Methods
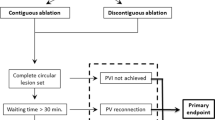
Both in vitro experiment and retrospective observational study were conducted. For in vitro experiment, radiofrequency lesions were created on explanted swine hearts in three different catheter contact angles (0°, 45°, and 90°). In the retrospective observational study, we assessed patients who had undergone repeat catheter ablation due to atrial fibrillation recurrence after initial PVI. When pulmonary vein (PV) reconnection was observed, we analyzed the previous ablation points within and without the gap area. The gap areas were where ablation had changed the PV activation sequence or eliminated the PV potential in the repeat session.
Results
In the in vitro experiment, lesion width was the smallest (5.3 ± 0.4 mm) in perpendicular contact compared to 0° (vs 5.8 ± 0.5 mm, p = 0.040) and 45° (vs 6.4 ± 0.4 mm, p < 0.001). In the retrospective observational study, we assessed 666 tags of 16 patients with PV reconnections, and 60 tags were in the gap area. Tags in the gap area had longer interlesion distance (odds ratio [OR] 1.49, p < 0.001), greater contact force variability (OR 1.03, p = 0.008), and higher rate of perpendicular contact (OR 3.26, p < 0.001) on multivariate analysis.
Conclusions
Perpendicular contact was associated with a smaller lesion and higher rate of PV reconnection.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Pulmonary vein isolation (PVI) is a cornerstone therapy in catheter ablation of atrial fibrillation (AF) [1]. Studies on AF recurrence rates after initial ablation procedures have been variable, ranging from 20 to 80% in several studies, and 20–50% of patients require a repeat ablation procedure to achieve sinus rhythm during long-term follow-up [2, 3]. The left atrial (LA)–pulmonary vein (PV) reconnection after initial PVI is one of the main causes of AF recurrence [4]. Therefore, durable lesion formation is important in preventing recurrences of AF.
Three-dimensional mapping systems, irrigation catheters, and contact-force (CF) sensing catheter have been developed to improve lesion durability. Furthermore, force–time integral (FTI) and other lesion indexing algorithms, including ablation index (AI), have been used as surrogates for radiofrequency (RF) dose and lesion size. However, LA–PV reconnection remains unclear with these instruments [5,6,7].
Catheter stability can be a factor of durable lesion formation beyond FTI or AI. Makimoto et al. supposed that, even if the mean CF applied is within the target range, a large variability of the actual CF value during RF application suggests catheter instability [8]. Ullah et al. have also shown larger CF variability resulting in smaller impedance drop [9]. Moreover, they showed several factors associated with lesser impedance drop: catheter CF variability > 5 g, catheter drift > 3.5 mm, sinus rhythm, and perpendicular contact [9]. However, little is known about the effect of catheter contact angle against the myocardium on lesion formation and durability of PVI.
This study aimed to evaluate the impact of catheter contact angle on lesion formation and durability of PVI.
2 Methods
We conducted both in vitro experiment and retrospective observational study. The retrospective analysis was in accordance with the “Declaration of Helsinki” and approved by the Ethics Committee of Teine Keijinkai Hospital (2–020,132-00).
2.1 In vitro experiments
The swine’s heart ventricular tissue was dissected and pinned to a tissue holder that was fixed in a saline bath. Using a CARTO system (Biosense Webster, Inc.) and a ThermoCool SmartTouch irrigated-tip CF sensing RF ablation catheter (Biosense Webster, Inc.), RF lesions were created with ablation power of 20 W for 15 s with saline 8-mL/min irrigation in two different catheter CFs (5 g and 10 g) and three different catheter contact angles (0°, 45°, and 90°) (Fig. 1A). Five radiofrequency applications were applied under each condition, and 30 lesions were created. The lesions were sectioned along their major axis, and widths and depths were measured (Fig. 1B). We also investigated each FTI, AI, impedance before RF application (pre-impedance), impedance after RF application (post-impedance), and impedance change (impedance drop).
Representative catheter position during radiofrequency application to Swine’s heart (A) and the lesion (B). Radiofrequency applications were conducted on the swine’s heart ventricular tissue in a saline bath (A). The lesions were sectioned along their major axis, and widths and depths were measured (B)
2.2 Retrospective observation study
2.2.1 Patient population
We included 27 consecutive patients who underwent repeat catheter ablation due to AF recurrence after initial PVI using the CARTO system and VisiTag™ module from October 1, 2017, to August 31, 2019. All patients provided written informed consent before the procedures.
2.2.2 Catheter ablation procedure
All patients underwent the procedure under sedation. Transesophageal echocardiography was performed to rule out thrombus in the left atrium before the procedure. After dual transseptal puncture, 3D electroanatomical maps of the LA and PVs were reconstructed with a PentaRay (Biosense Webster, Inc.) in each session. In the first session, extensive encircling PVI was performed by point-by-point RF application using a ThermoCool SmartTouch irrigated-tip CF sensing RF ablation catheter (Biosense Webster, Inc.). Ablation power was 20–25 W for posterior wall and 25–30 W for anterior wall, and the target ablation index was 375 for posterior wall and 425 for anterior wall. Ablation lesion was manually tagged routinely after the catheter was stabilized to record the catheter position and the vector arrows showing actual angle of catheter tip to the tissue (Fig. 2B). VisiTag™ was also annotated automatically on the lesion, based on the location stability setting of 3 mm for 10 s with respiration adjustment and without force over time or impedance drop filters. When first-pass isolation was not achieved, reablation would be applied at the sites with conduction gap until both exit and entrance blocks were achieved. In the repeat session, RF ablation was applied at the sites with conduction gap if LA–PV reconnection was observed.
Representative VisiTags shown in the CARTO system. Ablation areas were divided into ten areas for each ipsilateral pulmonary vein (A). Ablation points were manually tagged to record the catheter position and the vector arrows showing actual angle of catheter tip to tissue. Perpendicular contact was defined when the angle between the vertical line to the ablation catheter and the vector arrow was > 60° (B). Recorded VisiTag information (C). Dmax is the maximum distance to the adjacent tags. AR, anterior roof; AS, anterior superior; AC, anterior carina; AI, anterior inferior; AB, anterior bottom; PR, posterior roof; PS, posterior superior; PC, posterior carina; PI, posterior inferior; PB, posterior bottom; FTI, force–time integral; AI, ablation index
2.2.3 Study measurements
We assessed the previous RF application of patients with LA–PV reconnection confirmed in the repeat session. The tags were excluded from the analysis if two or more VisiTags were annotated with one RF application. The PVI line of each ipsilateral PV was divided into ten areas by anterior/posterior and roof/superior/carina/inferior/bottom (Fig. 2A). The gap areas were defined where RF ablation had changed the PV activation sequence or eliminated the PV potential in the repeat session. The angle between the vector arrow and vertical line to the ablation catheter was measured by a semicircular protractor, using the ablation point recorded in the initial session. Perpendicular contact was defined when the angle between the vertical line to the ablation catheter and the vector arrow was > 60° (Fig. 2B). We investigated all VisiTag™ information of initial PVI: ablation time, ablation power, catheter temperature, CF, FTI, AI, generator impedance, and maximum distance to the adjacent tags (Dmax) (Fig. 2C). CF variability was defined as the difference between maximum and minimum CF.
2.3 Statistical analysis
In in vitro experiments, to compare three different catheter contact angles, we performed the one-way analysis of variance. We also performed Student’s t-test to compare two groups. In the retrospective analysis of PVI, all ablation information was compared using Student’s t-test and chi-square test for continuous and categorical variables, respectively. Univariate analysis was conducted on factors identified as significant by these methods; then, multivariate analysis with a logistic regression model was performed using the significant variables identified by univariate analysis to define an independent predictor of the gap area. We also assessed the points without Dmax > 6 mm and evaluated them in the same way. Receiver operating characteristic analysis was performed to determine the optimal cut-off value of Dmax that exhibited optimal sensitivity and specificity. The value for the maximum Youden index was considered as the optimal cut-off point. A P-value < 0.05 was considered statistically significant. All statistical analyses were performed using EZR (Saitama Medical Center, Jichi Medical University, Saitama, Japan), a graphical user interface for R (The R Foundation for Statistical Computing, Vienna, Austria) designed to add statistical functions frequently used in biostatistics [10].
3 Results
3.1 In vitro experiments
In perpendicular contact (contact angle of 90°), lesion width was the smallest (5.3 ± 0.4 mm) compared to 0° (vs 5.8 ± 0.5 mm, p = 0.040) and 45° (vs 6.4 ± 0.4 mm, p < 0.001), while lesion depth had no significant differences (Fig. 3). FTI and AI had no significant differences among the three groups (Table 1). As for generator impedance, both impedance drop and impedance before RF application were the largest in 45° (Table 1).
3.2 Retrospective analysis of PVI
Table 2 shows the baseline characteristics of the included patients. The overall patients included 22 men (81.5%) with mean age of 60.7 ± 9.4 years. Ten patients (37.0%) had paroxysmal AF. The mean period from the previous session was 358.4 ± 202.4 days. The LA–PV reconnections were detected in 21 ipsilateral PVs (38.9%) in 16 patients (59.3%). We assessed 666 tags of these 16 patients, and 60 tags were in the gap area. The left anterior carina area was the most frequent site of the gap area (n = 14), following the right posterior carina area (n = 11), the right posterior superior area (n = 8), and the left posterior superior area (n = 5). The tags in the gap area had higher rate of perpendicular contact (50.0% vs 16.7%, p < 0.001), longer Dmax (6.9 ± 1.8 vs 5.9 ± 1.5, p < 0.001), lower minimum CF (2.3 ± 3.5 vs 4.8 ± 5.1, p < 0.001), greater CF variability (30.2 ± 20.9 vs 24.1 ± 14.5, p = 0.003), lower FTI (243.2 ± 142.0 vs 289.0 ± 145.8, p = 0.020), higher ablation power, and lower impedance (maximum, minimum), although other variables, such as AI and impedance drop, showed no significant differences (Table 3). In the multivariate analysis, longer Dmax (OR 1.49, p < 0.001), larger CF variability (OR 1.03, p = 0.008), and perpendicular contact (OR 3.26, p < 0.001) were associated with the gap area (Table 3). Moreover, 19 of 381 points with Dmax ≤ 6 mm were detected in the gap area. In ablation points with Dmax ≤ 6 mm, larger CF variability (OR 1.05, p = 0.005) and perpendicular contact (OR 3.47, p = 0.025) were the predictors of PV reconnection on multivariate analysis (Table 4).
Table 5 shows the comparison between non-perpendicular (n = 535) and perpendicular contact (n = 131). Although maximum CF was significantly high in perpendicular contact than non-perpendicular contact (31.9 ± 21.9 vs 28.6 ± 14.8, p < 0.040), minimum CF was low (2.2 ± 3.4 vs 5.2 ± 5.2, p < 0.001), resulting in larger CF variability (29.8 ± 20.9 vs 23.4 ± 13.2, p < 0.001). As for generator impedance, perpendicular contact was associated with lower maximum and minimum impedance with lower impedance drop compared to non-perpendicular contact. Figure 4 shows the common gap areas and the frequency of perpendicular contact in each area. The common gap areas were left anterior carina, left posterior-superior area, right postero-superior area and right posterior carina. The frequency of perpendicular contact was 37.8–65.2%.
The common gap areas and the frequency of perpendicular contact in each area. The common gap areas are highlighted, and the frequency of perpendicular contact is shown in each area. The most common gap area is the left carina anterior area (n = 14), following the right carina posterior area (n = 11), the right posterior superior area (n = 8), and the left posterior superior area (n = 5). AR, anterior roof; AS, anterior superior; AC, anterior carina; AI, anterior inferior; AB, anterior bottom; PR, posterior roof; PS, posterior superior; PC, posterior carina; PI, posterior inferior; PB, posterior bottom
4 Discussion
Our data shows that (I) the lesion size is small in perpendicular contact and (II) perpendicular contact is a strong predictor of the LA–PV reconnection in PVI.
4.1 RF lesion created in different catheter contact angles
In our in vitro study, although AI and FTI did not show significant differences among different catheter contact angles, the lesion width was small in the perpendicular contact and large in 45°. We also found that initial impedance was significantly high in 45°.
Recent in vitro study demonstrated by V. Calzolari et al. [11] is consistent with our study. RF lesions created on a porcine heart with different contact angles were evaluated, and they measured both superficial lesion size and cross-sectional lesion size. They have shown that both superficial lesion length and cross-sectional lesion length were larger in parallel contact than in perpendicular contact.
In vitro experiments have shown that FTI or ablation index is known to be associated with lesion size [12, 13]. However, AI and FTI do not consider contact angle at ablation sites that affect initial impedance, which in turn can influence lesion formation [14].
Lesions formed by RF application consist of two regions: a central region formed by resistive heating and a surrounding hemorrhagic region formed by conductive heat transfer that depends on application time. The lesion size influenced by resistive heating is determined by the amount of current delivered to the tissue [15]. According to Joule’s law, the amount of current is inversely proportional to the circuit impedance. Impedance represents resistance to current flow in the local tissue if other variables are under the same condition, including the RF generator, catheter, tissue distant to the heart, and return electrode, and in the general circuit cabling [16]. The resistance of local tissue can be affected by tissue properties, catheter CF, or surface area covered by the catheter tip. In our study, as the catheter CF was fixed, lower impedance before ablation in perpendicular contact might be due to the narrower contact area between the catheter tip and myocardium, resulting in a small lesion.
4.2 Factors of LA–PV reconnection in PVI
In our study, 38.9% of PVs (21 of 54) in 16 of 27 patients (59.3%) had PV reconnection in the repeat session. Univariate analysis showed several factors associated with PV reconnection: long interlesion distance; low minimum CF; high CF variability; low initial, maximum, and minimum impedance; and perpendicular contact.
The importance of catheter CF has been investigated in studies examining the reconnection of segments in PVI line during AF ablation. The EFFICAS I study has shown that PV reconnection at 3 months after PVI was strongly associated with minimum CF and minimum FTI at the site of gap. In the EFFICAS II study, although the PV reconnection rates decreased following the CF guidance from EFFICAS I (target 20 g, range 10–30 g, minimum 400 g*s FTI), 15% of PV reconnections were still detected [6].
Catheter stability has been considered an important factor beyond FTI. Catheter stability was previously assessed using CF variability or relative standard deviation of CF. One in vitro study using a contractile bench model simulating the beating heart showed more variable contact resulting in smaller lesions [12]. In the clinical study, Ullah et al. [9] demonstrated that lesions delivered with variability over 5 g are associated with a lower impedance drop, despite delivering the same FTI. They suggested that high degree of CF variability leads to a cooling effect on the tissue through stretching and unstretching, reducing the effect of ablation. Makimoto et al. [8] demonstrated that the relationship between the average and standard deviation of CF is correlated with acute PV reconnection. They show that ablation segments along the circumferential ablation lines delivered with lower average force and high variability are prone to form reconnection gaps. In our study, compared to non-perpendicular contact, larger maximum CF, lower minimum CF, and larger CF variability during application were observed especially in perpendicular contact, indicating larger CF variability. Therefore, perpendicular contact can be a predictive factor of catheter instability leading to a nondurable lesion.
Interlesion distance is another important factor. A ‘CLOSE’ protocol ablation, targeting an interlesion distance ≤ 6 mm, AI ≥ 400, and ≥ 550 at the posterior and anterior walls, has been reported with better outcome with lower PV reconnection and lower AF recurrence rate [7]. In our study, 19 of 381 points with Dmax ≤ 6 mm were still detected in the gap area. Once interlesion distance ≤ 6 mm was achieved, CF variability and perpendicular contact were the only two predictors of PV reconnection in the multivariate analysis. Although it has been reported that CF variability did not differ if AI is constant [7], when focusing on patients with PV reconnection, CF variability and perpendicular contact might be additional factors beyond AI in terms of durable lesion formation.
4.3 Difference between paroxysmal and persistent AF
When we compared paroxysmal AF (n = 10) with persistent AF (n = 17), the rate of perpendicular catheter contact was more frequently observed in paroxysmal AF (28.1% vs 6.7%, p = 0.001). Smaller left atrial volume was also observed in paroxysmal atrial fibrillation (60.1 ml vs 95.5 ml, p = 0.001). Therefore, because the catheter manipulation is limited in a small left atrium, achieving parallel catheter contact might be difficult in paroxysmal atrial fibrillation.
4.4 Limitations
Several limitations need to be underlined. An in vitro study was conducted under limited setting of CF, ablation time, and power. To avoid steam pop phenomenon, lower CF and lower power were selected compared with other in vitro studies [11,12,13,14]. CF variability was not evaluated, and it is not clear whether the lesion size difference of in vitro study is clinically significant. In addition, the superficial lesion width was not measured because we measured the lesion size after lesions were sectioned along their major axis. The major limitation of the retrospective study was that it was conducted in a single-center and had a small sample size. In particular, most of the study population were men (81.5%), although men account for a large percentage (64–83%) in other studies of patients with atrial fibrillation recurrence after catheter ablation [17,18,19]. Moreover, the operator’s habit to apply the catheter might have effect on the gap area because the contact angle tended to be the same in the same area. Further research including an in vivo animal study and a prospective study at multiple facilities is required.
5 Conclusion
Perpendicular contact was associated with smaller in vitro lesion size, and clinically, in this retrospective series including 27 patients, it was an indicator of catheter instability during PVI, resulting in nondurable lesion.
Abbreviations
- AF :
-
Atrial fibrillation
- AI :
-
Ablation index
- CF :
-
Contact-force
- EACTS :
-
European Association of Cardio-Thoracic Surgery
- FTI :
-
Force–time integral
- LA :
-
Left atrial
- PV :
-
Pulmonary vein
- PVI :
-
Pulmonary vein isolation
- ROC :
-
Receiver operating characteristic curve
References
Hindricks G, Potpara T, Dagres N, et al. 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS): the task force for the diagnosis and management of atrial fibrillation of the European Society of Cardiology (ESC) developed with the special contribution of the European Heart Rhythm Association (EHRA) of the ESC [published correction appears in Eur Heart J. 2021 Feb 1;42(5):507] [published correction appears in Eur Heart J. 2021 Feb 1;42(5):546–547] [published correction appears in Eur Heart J. 2021 Feb 1;42(5):541–543]. Eur Heart J. 2021;42(5):373–498. https://doi.org/10.1093/eurheartj/ehaa612
Murakawa Y, Nogami A, Shoda M, et al. Nationwide survey of catheter ablation for atrial fibrillation: the Japanese Catheter Ablation Registry of Atrial Fibrillation (J-CARAF)–report of 1-year follow-up. Circ J. 2014;78(5):1091–6. https://doi.org/10.1253/circj.cj-14-0099.
Tzou WS, Marchlinski FE, Zado ES, et al. Long-term outcome after successful catheter ablation of atrial fibrillation. Circ Arrhythm Electrophysiol. 2010;3(3):237–42. https://doi.org/10.1161/CIRCEP.109.923771.
Ouyang F, Antz M, Ernst S, et al. Recovered pulmonary vein conduction as a dominant factor for recurrent atrial tachyarrhythmias after complete circular isolation of the pulmonary veins: lessons from double Lasso technique. Circulation. 2005;111(2):127–35. https://doi.org/10.1161/01.CIR.0000151289.73085.36.
Neuzil P, Reddy VY, Kautzner J, et al. Electrical reconnection after pulmonary vein isolation is contingent on contact force during initial treatment: results from the EFFICAS I study. Circ Arrhythm Electrophysiol. 2013;6(2):327–33. https://doi.org/10.1161/CIRCEP.113.000374.
Kautzner J, Neuzil P, Lambert H, et al. EFFICAS II: optimization of catheter contact force improves outcome of pulmonary vein isolation for paroxysmal atrial fibrillation. Europace. 2015;17(8):1229–35. https://doi.org/10.1093/europace/euv057.
Phlips T, Taghji P, El Haddad M, et al. Improving procedural and one-year outcome after contact force-guided pulmonary vein isolation: the role of interlesion distance, ablation index, and contact force variability in the ‘CLOSE’-protocol. Europace. 2018;20(FI_3):f419-f427. https://doi.org/10.1093/europace/eux376
Makimoto H, Tilz RR, Lin T, et al. Incidence and anatomical locations of catheter instability during circumferential pulmonary vein isolation using contact force. Int Heart J. 2014;55(3):249–55. https://doi.org/10.1536/ihj.13-302.
Ullah W, Hunter RJ, Baker V, et al. Factors affecting catheter contact in the human left atrium and their impact on ablation efficacy. J Cardiovasc Electrophysiol. 2015;26(2):129–36. https://doi.org/10.1111/jce.12542.
Kanda Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone marrow transplant. 2013;48(3):452–8. https://doi.org/10.1038/bmt.2012.244.
Calzolari V, De Mattia L, Basso F, et al. Ablation catheter orientation: in vitro effects on lesion size and in vivo analysis during PVI for atrial fibrillation. Pacing Clin Electrophysiol. 2020;43(12):1554–63. https://doi.org/10.1111/pace.14106.
Shah DC, Lambert H, Nakagawa H, Langenkamp A, Aeby N, Leo G. Area under the real-time contact force curve (force-time integral) predicts radiofrequency lesion size in an in vitro contractile model. J Cardiovasc Electrophysiol. 2010;21(9):1038–43. https://doi.org/10.1111/j.1540-8167.2010.01750.x.
Mori H, Kato R, Sumitomo N, et al. Relationship between the ablation index, lesion formation, and incidence of steam pops. J Arrhythm. 2019;35(4):636–644. Published 2019 Jun 1. https://doi.org/10.1002/joa3.12195
Barkagan M, Rottmann M, Leshem E, Shen C, Buxton AE, Anter E. Effect of baseline impedance on ablation lesion dimensions: a multimodality concept validation from physics to clinical experience. Circ Arrhythm Electrophysiol. 2018;11(10):e006690. https://doi.org/10.1161/CIRCEP.118.006690.
Eick OJ. Factors influencing lesion formation during radiofrequency catheter ablation. Indian Pacing Electrophysiol J. 2003;3(3):117–128. Published 2003 Jul 1.
Bhaskaran A, Barry MA, Pouliopoulos J, et al. Circuit impedance could be a crucial factor influencing radiofrequency ablation efficacy and safety: a myocardial phantom study of the problem and its correction. J Cardiovasc Electrophysiol. 2016;27(3):351–7. https://doi.org/10.1111/jce.12893.
Kim YG, Boo KY, Choi JI, et al. Early recurrence is reliable predictor of late recurrence after radiofrequency catheter ablation of atrial fibrillation. JACC Clin Electrophysiol. 2021;7(3):343–51. https://doi.org/10.1016/j.jacep.2020.09.029.
Kim TH, Park J, Uhm JS, Joung B, Lee MH, Pak HN. Pulmonary vein reconnection predicts good clinical outcome after second catheter ablation for atrial fibrillation. Europace. 2017;19(6):961–7. https://doi.org/10.1093/europace/euw128.
Sultan A, Lüker J, Andresen D, et al. Predictors of atrial fibrillation recurrence after catheter ablation: data from the German Ablation Registry. Sci Rep. 2017;7(1):16678. Published 2017 Nov 30. https://doi.org/10.1038/s41598-017-16938-6
Author information
Authors and Affiliations
Contributions
Conceptualization: Kentaro Hayashi; methodology: Masayuki Ohta and Kentaro Hayashi; formal analysis and investigation: Hiroyuki Sato, Kandoh Kawahatsu, and Masaya Katagiri; writing — original draft preparation: Masayuki Ohta; writing — review and editing: Tomohiro Mita, Yoshio Kazuno, Shunsuke Sasaki, and Takahiro Doi; supervision: Mitsugu Hirokami and Satoshi Yuda.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ohta, M., Hayashi, K., Sato, H. et al. Impact of catheter contact angle on lesion formation and durability of pulmonary vein isolation. J Interv Card Electrophysiol 64, 677–685 (2022). https://doi.org/10.1007/s10840-022-01131-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10840-022-01131-1