Abstract
Purpose
The purpose of this study was to investigate the relationship between the accessory pathway location and brain natriuretic peptide (BNP) level in patients with Wolff–Parkinson–White (WPW) syndrome.
Methods
We divided 102 WPW syndrome patients with normal left ventricular systolic function into four groups: those with manifest right (MR, n = 14), manifest septal (MS, n = 11), manifest left (ML, n = 30), and concealed (C, n = 47) accessory pathways. BNP level and electrophysiological properties, including difference in timing of the ventricular electrogram between the His bundle area and the distal coronary sinus area (His–CS delay), which indicate intraventricular dyssynchrony, were compared.
Results
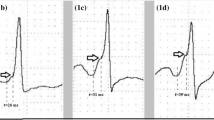
BNP levels (pg/dl) were higher in the MR and MS groups than in the ML and C groups (MR, 64 ± 58; MS, 55 ± 45; ML, 17 ± 15; C, 25 ± 21; P < 0.001). AV intervals (ms) were shorter in the MR and MS groups than in the ML and C groups (MR, 76 ± 16; MS, 83 ± 6; ML, 101 ± 19; C, 136 ± 20; P < 0.001). His–CS delay (ms) was longer in the MR group than in the other groups (MR, 50 ± 15; MS, 21 ± 7; ML, 23 ± 10; C, 19 ± 8; P < 0.001). The AV interval (P < 0.01) and the His–CS delay (P < 0.001) were negatively and positively correlated, respectively, with the BNP level.
Conclusion
Anterograde conduction with a right or septal accessory pathway increased the BNP level in WPW syndrome patients with normal cardiac function.



Similar content being viewed by others
References
Hishida H, Sotobata I, Koike Y, Okumura M, Mizuno Y. Echocardiographic patterns of ventricular contraction in the Wolff-Parkinson-White syndrome. Circulation. 1976;54:567–70.
Chandra MS, Kerber RE, Brown DD, Funk DC. Echocardiography in Wolff-Parkinson-White syndrome. Circulation. 1976;53:943–6.
Francis GS, Theroux P, O’Rourke RA, Hagan AD, Johnson AD. An echocardiographic study of interventricular septal motion in the Wolff-Parkinson-White syndrome. Circulation. 1976;54:174–8.
Tomaske M, Janousek J, Rázek V, Gebauer RA, Tomek V, Hindricks G, et al. Adverse effects of Wolff-Parkinson-White syndrome with right septal or posteroseptal accessory pathways on cardiac function. Europace. 2008;10:181–9.
Kwon BS, Bae EJ, Kim GB, Noh CI, Choi JY, Yun YS. Septal dyskinesia and global left ventricular dysfunction in pediatric Wolff-Parkinson-White syndrome with septal accessory pathway. J Cardiovasc Electrophysiol. 2010;21:290–5.
De Boeck BW, Teske AJ, Leenders GE, Mohamed Hoesein FA, Loh P, van Driel VJ, et al. Detection and quantification by deformation imaging of the functional impact of septal compared to free wall preexcitation in the Wolff-Parkinson-White syndrome. Am J Cardiol. 2010;106:539–46.
Park HE, Chang SA, Kim JH, Oh IY, Choi EK, Oh S. Left ventricular dyssynchrony in pre-excitation syndrome: effect of accessory pathway location and reversibility after ablation therapy. Heart Vessels. 2013;28:199–207.
Udink ten Cate FE, Kruessell MA, Wagner K, Trieschmann U, Emmel M, Brockmeier K, et al. Dilated cardiomyopathy in children with ventricular preexcitation: the location of the accessory pathway is predictive of this association. J Electrocardiol. 2010;43:146–54.
Fukunaga H, Akimoto K, Furukawa T, Takahashi K, Kishiro M, Shimizu T, et al. Improvement in non-tachycardia-induced cardiac failure after radiofrequency catheter ablation in a child with a right-sided accessory pathway. Heart Vessels. 2013;28:802–7.
Fujii J, Wantanabe H, Watanabe T, Takahashi N, Ohta A, Kato K. M-mode and cross-sectional echocardiographic study of the left ventricular wall motions in complete left bundle-branch block. Br Heart J. 1979;42(3):255–60.
Tsutamoto T, Wada A, Maeda K, Hisanaga T, Maeda Y, Fukai D, et al. Attenuation of compensation of endogenous cardiac natriuretic peptide system in chronic heart failure: prognostic role of plasma brain natriuretic peptide concentration in patients with chronic symptomatic left ventricular dysfunction. Circulation. 1997;96:509–16.
Chen HH, Burnett JC. Natriuretic peptides in the pathophysiology of congestive heart failure. Curr Cardiol Rep. 2000;2:198–205.
Ohba H, Takada H, Musha H, Nagashima J, Mori N, Awaya T, et al. Effects of prolonged strenuous exercise on plasma levels of atrial natriuretic peptide and brain natriuretic peptide in healthy men. Am Heart J. 2001;141:751–8.
Cosío FG, Anderson RH, Kuck KH, Becker A, Borggrefe M, Campbell RW, et al. Living anatomy of the atrioventricular junctions. A guide to electrophysiologic mapping. A Consensus Statement from the Cardiac Nomenclature Study Group, Working Group of Arrhythmias, European Society of Cardiology, and the Task Force on Cardiac Nomenclature from NASPE. Circulation. 1999;100:e31–7.
Pitzalis MV, Iacoviello M, Romito R, Guida P, De Tommasi E, Luzzi G, et al. Ventricular asynchrony predicts a better outcome in patients with chronic heart failure receiving cardiac resynchronization therapy. J Am Coll Cardiol. 2005;45:65–9.
Tulevski II, Groenink M, van Der Wall EE, van Veldhuisen DJ, Boomsma F, Stoker J, et al. Increased brain and atrial natriuretic peptides in patients with chronic right ventricular pressure overload: correlation between plasma neurohormones and right ventricular dysfunction. Heart. 2001;86:27–30.
Redfield MM, Rodeheffer RJ, Jacobsen SJ, Mahoney DW, Bailey KR, Burnett Jr JC. Plasma brain natriuretic peptide concentration: impact of age and gender. J Am Coll Cardiol. 2002;40:976–82.
Horwich TB, Hamilton MA, Fonarow GC. B-type natriuretic peptide levels in obese patients with advanced heart failure. J Am Coll Cardiol. 2006;47:85–90.
Burke MA, Cotts WG. Interpretation of B-type natriuretic peptide in cardiac disease and other comorbid conditions. Heart Fail Rev. 2007;12:23–36.
Tsutamoto T, Wada A, Sakai H, Ishikawa C, Tanaka T, Hayashi M, et al. Relationship between renal function and plasma brain natriuretic peptide in patients with heart failure. J Am Coll Cardiol. 2006;47:582–6.
Vickery S, Price CP, John RI, Abbas NA, Webb MC, Kempson ME, et al. B-Type natriuretic peptide (BNP) and amino-terminal proBNP in patients with CKD: relationship to renal function and left ventricular hypertrophy. Am J Kidney Dis. 2005;46:610–20.
Levin ER, Gardner DG, Samson WK. Natriuretic peptides. N Engl J Med. 1998;339:321–8.
Pappone C, Vicedomini G, Manguso F, Saviano M, Baldi M, Pappone A, et al. Wolff-Parkinson-White syndrome in the era of catheter ablation: insights from a registry study of 2169 patients. Circulation. 2014;130:811–9.
Bunch TJ, May HT, Bair TL, Anderson JL, Crandall BG, Cutler MJ, et al. Long-term natural history of adult Wolff-Parkinson-White syndrome patients treated with and without catheter ablation. Circ Arrhythm Electrophysiol. 2015;8:1465–71.
Pediatric and Congenital Electrophysiology Society (PACES), Heart Rhythm Society (HRS), American College of Cardiology Foundation (ACCF), American Heart Association (AHA), American Academy of Pediatrics (AAP), Canadian Heart Rhythm Society (CHRS), et al. PACES/HRS expert consensus statement on the management of the asymptomatic young patient with a Wolff-Parkinson-White (WPW, ventricular preexcitation) electrocardiographic pattern: developed in partnership between the Pediatric and Congenital Electrophysiology Society (PACES) and the Heart Rhythm Society (HRS). Endorsed by the governing bodies of PACES, HRS, the American College of Cardiology Foundation (ACCF), the American Heart Association (AHA), the American Academy of Pediatrics (AAP), and the Canadian Heart Rhythm Society (CHRS). Heart Rhythm. 2012;9:1006–24.
Acknowledgments
This research received no grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Funding
This study was not funded.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
For this type of study, formal consent is not required.
Rights and permissions
About this article
Cite this article
Nakatani, Y., Kumagai, K., Naito, S. et al. Accessory pathway location affects brain natriuretic peptide level in patients with Wolff–Parkinson–White syndrome. J Interv Card Electrophysiol 48, 81–88 (2017). https://doi.org/10.1007/s10840-016-0205-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10840-016-0205-7