Abstract
Purpose
The aim of this study is to describe a new simple score to predict the occurrence of severe adverse events in patients admitted for syncope to a tertiary cardiology referral center.
Methods
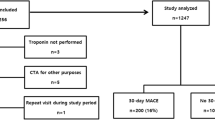
Three hundred ninety-three subjects with emergency department visits for syncope were identified and followed prospectively. The primary endpoint was death or unplanned hospital admission after the syncopal episode. The score consisted of sum of the following: previous syncope (2 points), an abnormal electrocardiogram (3 points), and history of heart disease (4 points). The accuracy of our score was compared to other scores available in the literature.
Results
Of the 393 subjects, 87 were diagnosed with syncope secondary to structural or electrical heart disease and 306 with noncardiac syncope. The primary endpoint occurred in 202 cases, including death occurring in 25 patients during the 12-month follow-up. The 30-day event rate for the primary endpoint was 26.5 %. The c-statistic for the new score was 0.76 (95 % CI 0.71–0.80) similar to other scores when applied to our sample. Patients with a score of 3 out of 9 had a hazard ratio of 3.46 (95 % CI 1.22–6.11) for death during the follow-up.
Conclusions
In the study population, the new syncope score detected patients with an increased risk of death after discharge from a syncopal event. Our score predicted adverse events comparably to other scores reported in the literature. It has the advantage of being simple and easily obtained from the history and an inexpensive noninvasive test—the ECG.



Similar content being viewed by others
Abbreviations
- AV:
-
Atrioventricular
- Bpm:
-
Beats per minute
- CAD:
-
Coronary artery disease
- CI:
-
Confidence interval
- COPD:
-
Chronic obstructive pulmonary disease
- ECG:
-
Electrocardiogram
- Hb:
-
Hemoglobin
- HR:
-
Hazard ratio
- ICD:
-
International Classification of Diseases
- LBBB:
-
Left bundle branch block
- OR:
-
Odds ratio
- RBBB:
-
Right bundle branch block
- Sat:
-
Oxygen saturation
- SAH:
-
Systemic arterial hypertension
References
Reed MJ, Hir BC, Newby DE, Coull AJ, Bs C, Prescott RJ, et al. The ROSE (risk stratification of syncope in the emergency department) study. JACC. 2010;55:713–721. doi:10.1016/j.jacc.2009.09.049.
Del Rosso A, Ungar A, Maggi R, Giada F, Petix NR, De Santo T, et al. Clinical predictors of cardiac syncope at initial evaluation in patients referred urgently to a general hospital: the EGSYS score. Heart. 2008;94:1620–6. doi:10.1136/hrt.2008.143123
Colivicchi F. Development and prospective validation of a risk stratification system for patients with syncope in the emergency department: the OESIL risk score. Eur Heart J. 2003;24:811–819. doi:10.1016/S0195-668X(02)00827-8.
Quinn J V, Stiell IG, McDermott DA, Kohn MA, Wells GA. The San Francisco Syncope Rule vs physician judgment and decision making. Am J Emerg Med. 2005;23:782–6. doi:10.1016/j.ajem.2004.11.009.
Grossman SA, Fischer C, Lipsitz LA, Mottley L, Sands K, Thompson S, et al. Predicting adverse outcomes in syncope. J Emerg Med. 2007; 33:233–9. doi:10.1016/j.jemermed.2007.04.001.
Hensher M, Price M, Adomakoh S. Referral Hospitals. In: Jamison DT, Breman JG, Measham AR, Alleyne G, Claeson M, Evans DB, Jha P, et al., editors. Disease control priorities in developing countries. 2nd ed. Washington: World Bank; 2006.
Dudley R, KL J, Brand R, DJ R, Milstein A. Selective referral to high-volume hospitals: Estimating potentially avoidable deaths. JAMA. 2000;283:1159–1166. doi:10.1001/jama.283.9.1159.
Joynt KE, Orav EJ, Jha AK. The association between hospital volume and processes, outcomes, and costs of care for congestive heart failure. Ann Intern Med. 2011;154:94. doi:10.7326/0003-4819-154-2-201101180-00008.
Fischer LM, Dutra JPP, Mantovani A, Lima GG de, Leiria TLL. Predictors of hospitalization in patients with syncope assisted in specialized cardiology hospital. Arq Bras Cardiol. 2013;101:480–6. doi:10.5935/abc.20130206.
Costantino G, Perego F, Dipaola F, Borella M, Galli A, Cantoni G, et al. Short- and long-term prognosis of syncope, risk factors, and role of hospital admission. Results from the STePS (Short-Term Prognosis of Syncope) study. J Am Coll Cardiol. 2008;51:276–83.
Anon. ICD-10 classification. BMJ. 2010; 341.
Sun BC, Costantino G, Barbic F, Bossi I, Casazza G, Dipaola F, et al. Priorities for emergency department syncope research. Ann Emerg Med. 2014; 64:649–655.e2. doi:10.1016/j.annemergmed.2014.04.014.
Moya A, Sutton R, Ammirati F, Blanc J-J, Brignole M, Dahm JB, et al. Guidelines for the diagnosis and management of syncope (version 2009). Eur Heart J. 2009; 30:2631–71. doi:10.1093/eurheartj/ehp298.
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. 2015; 370:1453–1457. doi:10.1016/S0140-6736(07)61602-X.
Alboni P, Brignole M, Menozzi C, Raviele A, Del Rosso A, Dinelli M, Solano A, et al. Diagnostic value of history in patients with syncope with or without heart disease. J Am Coll Cardiol. 2001;37:1921–8.
Kapoor WN, Hanusa BH. Is syncope a risk factor for poor outcomes? Comparison of patients with and without syncope. Am J Med. 1996;100:646–55.
Brignole M, Disertori M, Menozzi C, Raviele A, Alboni P, Pitzalis M V, et al. Management of syncope referred urgently to general hospitals with and without syncope units. Europace. 2003;5:293–8.
Brignole M, Hamdan MH. New concepts in the assessment of syncope. J Am Coll Cardiol. 2012;59:1583–1591. doi:10.1016/j.jacc.2011.11.056.
Ammirati F, Colivicchi F, Minardi G, De Lio L, Terranova A, Scaffidi G, et al. [The management of syncope in the hospital: the OESIL Study (Osservatorio Epidemiologico della Sincope nel Lazio)]. G Ital Cardiol. 1999;29:533–9.
Blanc J-J, L’Her C, Touiza A, Garo B, L’Her E, Mansourati J. Prospective evaluation and outcome of patients admitted for syncope over a 1 year period. Eur Heart J. 2002;23:815–20. doi:10.1053/euhj.2001.2975.
Leifer A. Clinical judgment, clinical decision rules, and evidence-based medicine: thoughts on ‘an observation of failure to validate the San Francisco Syncope Rule’. Ann Emerg Med. 2009;53:164. doi:10.1016/j.annemergmed.2008.08.037.
Sun BC, Mangione CM, Merchant G, Weiss T, Shlamovitz GZ, Zargaraff G, et al. External validation of the San Francisco Syncope Rule. Ann Emerg Med. 2007;49:420–7, 427.e1–4. doi:10.1016/j.annemergmed.2006.11.012.
Costantino G, Casazza G, Reed M, Bossi I, Sun B, Del Rosso A, et al. Syncope risk stratification tools vs clinical judgment: an individual patient data meta-analysis. Am J Med. 2014;127:1126.e13–25. doi:10.1016/j.amjmed.2014.05.022.
Reed MJ, Henderson SS, Newby DE, Gray AJ. One-year prognosis after syncope and the failure of the ROSE decision instrument to predict one-year adverse events. Ann Emerg Med. 2011;58:250–6. doi:10.1016/j.annemergmed.2010.12.021.
Ungar A, Del Rosso A, Giada F, Bartoletti A, Furlan R, Quartieri F, et al. Early and late outcome of treated patients referred for syncope to emergency department: the EGSYS 2 follow-up study. Eur Heart J. 2010;31:2021–6. doi:10.1093/eurheartj/ehq017.
Ruwald MH, Hansen ML, Lamberts M, Kristensen SL, Wissenberg M, Olsen A-MS, et al. Accuracy of the ICD-10 discharge diagnosis for syncope. Europace. 2013;15:595–600.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The institutional research ethics committee in compliance with the Declaration of Helsinki approved the study.
Conflict of interest
The authors declare that they have no conflict of interest.
Funding
Dr. Essebag is the recipient of a Clinician Scientist award from the Canadian Institutes of Health Research (CIHR).
Rights and permissions
About this article
Cite this article
Gomes, D.G., Kus, T., Sant’anna, R.T. et al. Simple risk stratification score for prognosis of syncope. J Interv Card Electrophysiol 47, 153–161 (2016). https://doi.org/10.1007/s10840-016-0165-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10840-016-0165-y