Abstract
Background
Silent cerebral events (SCEs) have been observed on diffusion-weighted cerebral magnetic resonance imaging (MRI) in a substantial number of asymptomatic patients after atrial fibrillation (AF) ablation procedures. The purpose of this study was to investigate if periprocedural oral anticoagulation (OAC) management affects the incidence of new-onset SCE after radiofrequency catheter ablation (RFCA) of AF.
Methods and results
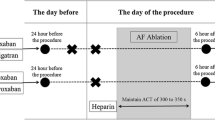
One hundred ninety-two consecutive patients (64 ± 10.1 years, 38.5 % women) with symptomatic paroxysmal (n = 80, 41.7 %) or persistent AF undergoing RFCA of AF were prospectively enrolled. Periprocedural anticoagulation strategies were defined as uninterrupted use of novel oral anticoagulants (NOACs) (group I, n = 64), interrupted use of NOACs (group II, n = 42), continuation of vitamin K antagonist (VKA) with an international normalized ratio (INR) between 2.0 and 3.0 (group III, n = 43), and VKA discontinuation bridged with low molecular weight heparin (group IV, n = 43). Cerebral MRI was performed 1 to 2 days after RFCA for detection of new SCE. Overall, new SCEs were detected in 41 patients (21.4 %) after AF ablation. New SCEs were detected in 12.5 % in group I, 35.7 % in group II, 18.6 % in group III, and 23.3 % in group IV (p < 0.05). Multivariable logistic regression analysis revealed persistent AF and discontinuation of periprocedural OAC (group II and IV) to be independent predictors for the development of SCE. No relevant complications were identified.
Conclusions
Periprocedural continuation of NOAC as well as continuation of VKA seems to be safe and significantly reduce the occurrence of SCE after AF ablation.



Similar content being viewed by others
Abbreviations
- ACT:
-
Activated clotting time
- AF:
-
Atrial fibrillation
- INR:
-
International normalized ratio
- FLAIR:
-
Fluid-attenuated inversion recovery
- LMH:
-
Low-molecular weight heparin
- LV-EF:
-
Left ventricular ejection fraction
- MRI:
-
Diffusion-weighted magnetic resonance imaging
- NOAC:
-
Novel/newer oral anticoagulant
- OAC:
-
Oral anticoagulation
- PVI:
-
Pulmonary vein isolation
- RFCA:
-
Radiofrequency catheter ablation
- SCE:
-
Silent cerebral event
- SCL:
-
Silent cerebral lesion
- TIA:
-
Transient ischemic attack
- UFH:
-
Unfractionated heparin
- VKA:
-
Vitamin K antagonist
References
Calkins, H., Reynolds, M. R., Spector, P., Sondhi, M., Xu, Y., Martin, A., Williams, C. J., & Sledge, I. (2009). Treatment of atrial fibrillation with antiarrhythmic drugs or radiofrequency ablation: two systematic literature reviews and meta-analyses. Circulation. Arrhythmia and Electrophysiology, 2, 349–361.
Santangeli, P., Di Biase, L., Horton, R., Burkhardt, J. D., Sanchez, J., Al-Ahmad, A., Hongo, R., Beheiry, S., Bai, R., Mohanty, P., Lewis, W. R., & Natale, A. (2012). Ablation of atrial fibrillation under therapeutic warfarin reduces periprocedural complications: evidence from a meta-analysis. Circulation. Arrhythmia and Electrophysiology, 5, 302–311.
Rojas-Hernandez, C. M., & Garcia, D. A. (2013). The novel oral anticoagulants. Seminars in Thrombosis and Hemostasis, 39, 117–126.
Lakkireddy, D., Reddy, Y. M., Di Biase, L., Vanga, S. R., Santangeli, P., Swarup, V., Pimentel, R., Mansour, M. C., D’Avila, A., Sanchez, J. E., Burkhardt, J. D., Chalhoub, F., Mohanty, P., Coffey, J., Shaik, N., Monir, G., Reddy, V. Y., Ruskin, J., & Natale, A. (2012). Feasibility and safety of dabigatran versus warfarin for periprocedural anticoagulation in patients undergoing radiofrequency ablation for atrial fibrillation: results from a multicenter prospective registry. Journal of the American College of Cardiology, 59, 1168–1174.
Kim, J. S., She, F., Jongnarangsin, K., Chugh, A., Latchamsetty, R., Ghanbari, H., Crawford, T., Suwanagool, A., Sinno, M., Carrigan, T., Kennedy, R., Saint-Phard, W., Yokokawa, M., Good, E., Bogun, F., Pelosi, F., Jr., Morady, F., & Oral, H. (2013). Dabigatran vs warfarin for radiofrequency catheter ablation of atrial fibrillation. Heart Rhythm, 10, 483–489.
Bassiouny, M., Saliba, W., Rickard, J., Shao, M., Sey, A., Diab, M., Martin, D. O., Hussein, A., Khoury, M., Abi-Saleh, B., Alam, S., Sengupta, J., Borek, P. P., Baranowski, B., Niebauer, M., Callahan, T., Varma, N., Chung, M., Tchou, P. J., Kanj, M., Dresing, T., Lindsay, B. D., & Wazni, O. (2013). Use of dabigatran for periprocedural anticoagulation in patients undergoing catheter ablation for atrial fibrillation. Circulation. Arrhythmia and Electrophysiology, 6, 460–466.
Deneke, T., Schade, A., Müller, P., Schmitt, R., Christopoulos, G., Krug, J., Szöllösi, G., Mügge, A., Kerber, S., & Nentwich, K. (2014). Acute safety and efficacy of a novel multipolar irrigated radiofrequency ablation catheter for pulmonary vein isolation. Journal of Cardiovascular Electrophysiology, 4, 339–345.
Deneke, T., Nentwich, K., Schmitt, R., Christhopoulos, G., Krug, J., Di Biase, L., Natale, A., Szöllösi, A., Mügge, A., Müller, P., Dietrich, J. W., Shin, D. I., Kerber, S., & Schade, A. (2014). Exchanging catheters over a single transseptal sheath during left atrial ablation is associated with a higher risk for silent cerebral events. Indian Pacing and Electrophysology Journal, 14, 240–249.
Deneke, T., Shin, D. I., Balta, O., Bünz, K., Fassbender, F., Mügge, A., Anders, H., Horlitz, M., Päsler, M., Karthikapallil, S., Arentz, T., Beyer, D., & Bansmann, M. (2011). Post-ablation asymptomatic cerebral lesions—long-term follow-up using magnetic resonance imaging. Heart Rhythm, 8, 1705–1711.
Di Biase, L., Gaita, F., Toso, E., Santangeli, P., Mohanty, P., Rutledge, N., Yan, X., Mohanty, S., Trivedi, C., Bai, R., Price, J., Horton, R., Gallinghouse, J., Beheiry, S., Zagrodsky, J., Canby, R., Leclerq, J. F., Halimi, F., Scaglione, M., Cesarini, F., Faletti, R., Sanchez, J., Burkhardt, D., & Natale, A. (2014). Does periprocedural anticoagulation management of atrial fibrillation affect the prevalence of silent thromboembolic lesion detected by diffusion cerebral magnetic resonance imaging in patients undergoing radiofrequency atrial fibrillation ablation with open irrigated catheters? Results from a prospective multicenter study. Heart Rhythm, 11, 791–798.
Gaita, F., Caponi, D., Pianelli, M., Scaglione, M., Toso, E., Cesarani, F., Boffano, C., Gandini, G., Valentini, M. C., De Ponti, R., Halimi, F., & Leclercq, J. F. (2010). Radiofrequency catheter ablation of atrial fibrillation: a cause of silent thromboembolism? Magnetic resonance imaging assessment of cerebral thromboembolism in patients undergoing ablation of atrial fibrillation. Circulation, 17, 1667–1673.
Müller, P., Maier, J., Dietrich, J. W., Barth, S., Griese, D. P., Schiedat, F., Szöllösi, A., Halbfass, P., Nentwich, K., Roos, M., Krug, J., Schade, A., Schmitt, R., Mügge, A., & Deneke, T. (2015). Association between left atrial low-voltage area, serum apoptosis and fibrosis biomarkers and incidence of silent cerebral events after catheter ablation of atrial fibrillation. Journal of Interventional Cardiac Electrophysiology, 1, 55–62.
Deneke, T., Jais, P., Scaglione, M., Schmitt, R., DI Biase, L., Christopoulos, G., Schade, A., Mügge, A., Bansmann, M., Nentwich, K., Müller, P., Krug, J., Roos, M., Halbfass, P., Natale, A., Gaita, F., & Haines, D. (2015). Silent cerebral events/lesions related to atrial fibrillation ablation: a clinical review. Journal of Cardiovascular Electrophysiology, 4, 455–463.
Scaglione, M., Blandino, A., Raimondo, C., Caponi, D., Di Donna, P., Toso, E., Ebrille, E., Cesarani, F., Ferrarese, E., & Gaita, F. (2012). Impact of ablation catheter irrigation design on silent cerebral embolism after radiofrequency catheter ablation of atrial fibrillation: results from a pilot study. Journal of Cardiovascular Electrophysiology, 23, 801–805.
Lakkireddy, D., Reddy, Y. M., Di Biase, L., Vallakati, A., Mansour, M. C., Santangeli, P., Gangireddy, S., Swarup, V., Chalhoub, F., Atkins, D., Bommana, S., Verma, A., Sanchez, J. E., Burkhardt, J. D., Barrett, C. D., Baheiry, S., Ruskin, J., Reddy, V., & Natale, A. (2014). Feasibility and safety of uninterrupted rivaroxaban for periprocedural anticoagulation in patients undergoing radiofrequency ablation for atrial fibrillation. Journal of the American College of Cardiology, 63, 982–988.
Dillier, R., Ammar, S., Hessling, G., Kaess, B., Pavaci, H., Buiatti, A., Semmler, V., Kathan, S., Hofmann, M., Lennerz, C., Kolb, C., Reents, T., & Deisenhofer, I. (2014). Safety of continuous periprocedural rivaroxaban for patients undergoing left atrial catheter ablation procedures. Circulation. Arrhythmia and Electrophysiology, 7, 576–582.
Di Biase, L., Burkhardt, J. D., Santangeli, P., Mohanty, P., Sanchez, J. E., Horton, R., Gallinghouse, G. J., Themistoclakis, S., Rossillo, A., Lakkireddy, D., Reddy, M., Hao, S., Hongo, R., Beheiry, S., Zagrodzky, J., Rong, B., Mohanty, S., Elayi, C. S., Forleo, G., Pelargonio, G., Narducci, M. L., Dello Russo, A., Casella, M., Fassini, G., Tondo, C., Schweikert, R. A., & Natale, A. (2014). Periprocedural stroke and bleeding complications in patients undergoing catheter ablation of atrial fibrillation with different anticoagulation management. Circulation, 129, 2638–2644.
Hussein, A. A., Martin, D. O., Saliba, W., Patel, D., Karim, S., Batal, O., Banna, M., Williams-Andrews, M., Sherman, M., Kanj, M., Bhargava, M., Dresing, T., Callahan, T., Tchou, P., Di Biase, L., Beheiry, S., Lindsay, B., & Natale, A. (2009). Radiofrequency ablation of atrial fibrillation under therapeutic international normalized ratio: a safe and efficacious periprocedural anticoagulation strategy. Heart Rhythm, 6, 1425–1429.
Patel, M. R., Mahaffey, K. W., Garg, J., Pan, G., Singer, D. E., Hacke, W., Breithardt, G., Halperin, J. L., Hankey, G. J., Piccini, J. P., Becker, R. C., Nessel, C. C., Paolini, J. F., Berkowitz, S. D., Fox, K. A. A., & Califf, R. M. (2011). Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. New England Journal of Medicine, 365, 883–891.
Connolly, S. J., Ezekowitz, M. D., Yusuf, S., Eikelboom, J., Oldgren, J., Parekh, A., Pogue, J., Reilly, P. A., Themeles, E., Varrone, J., Wang, S., Alings, M., Xavier, D., Zhu, J., Diaz, R., Lewis, B. S., Darius, H., Diener, H. C., Joyner, C. D., & Wallentin, L. (2009). Dabigatran versus warfarin in patients with atrial fibrillation. New England Journal of Medicine, 361, 1139–1151.
Granger, C. B., Alexander, J. H., McMurray, J. J., Lopes, R. D., Hylek, E. M., Hanna, M., Al-Khalidi, H. R., Ansell, J., Atar, D., Avezum, A., Bahit, M. C., Diaz, R., Easton, J. D., Ezekowitz, J. A., Flaker, G., Garcia, D., Geraldes, M., Gersh, B. J., Golitsyn, S., Goto, S., Hermosillo, A. G., Hohnloser, S. H., Horowitz, J., Mohan, P., Jansky, P., Lewis, B. S., Lopez-Sendon, J. L., Pais, P., Parkhomenko, A., Verheugt, F. W., Zhu, J., & Wallentin, L. (2011). Apixaban versus warfarin in patients with atrial fibrillation. New England Journal of Medicine, 365, 981–992.
Piccini, J. P., Stevens, S. R., Lokhnygina, Y., Patel, M. R., Halperin, J. L., Singer, D. E., Hankey, G. J., Hacke, W., Becker, R. C., Nessel, C. C., Mahaffey, K. W., Fox, K. A., Califf, R. M., & Breithardt, G. (2013). Outcomes after cardioversion and atrial fibrillation ablation in patients treated with rivaroxaban and warfarin in the ROCKET AF trial. Journal of the American College of Cardiology, 61, 1998–2006.
Eitel, C., Koch, J., Sommer, P., John, S., Kircher, S., Bollmann, A., Arya, A., Piorkowski, C., & Hindricks, G. (2013). Novel oral anticoagulants in a real-world cohort of patients undergoing catheter ablation of atrial fibrillation. Europace, 15, 1587–1593.
Naccarelli, G. V., Cappato, R., Hohnloser, S. H., Marchlinski, F. E., Wilber, D. J., Xiang, J., Ma, C., Hess, S., Davies, D. W., Fields, L. E., & Natale, A. (2014). Rationale and design of VENTURE-AF: a randomized, open-label, active-controlled multicenter study to evaluate the safety of rivaroxaban and vitamin K antagonists in subjects undergoing catheter ablation for atrial fibrillation. Journal of Interventional Cardiac Electrophysiology, 41, 107–116.
Di Biase, L., Lakkireddy, D., Trivedi, C., Deneke, T., Martinek, M., Mohanty, S., Mohanty, P., Prakash, S., Bai, R., Reddy, M., Gianni, C., Horton, R., Bailey, S., Sigmund, E., Derndorfer, M., Schade, A., Mueller, P., Szoelloesi, A., Sanchez, J., Al-Ahmad, A., Hranitzky, P., Gallinghouse, G. J., Hongo, R. H., Beheiry, S., Pürerfellner, H., Burkhardt, J. D., & Natale, A. (2015). Feasibility and safety of uninterrupted periprocedural apixaban administration in patients undergoing radiofrequency catheter ablation for atrial fibrillation: results from a multicenter study. Heart Rhythm, 12, 1162–1168.
Von Bary, C., Deneke, T., Arentz, T., Schade, A., Lehmann, H., Eissnert, C., Schwab-Malek, S., Fredersdorf, S., Ücer, E., Baldaranov, D., Wendl, C., & Schlachetzki, F. (2015). Silent cerebral events as a result of left atrial catheter ablation do not cause neuropsychological sequelae—a MRI-controlled multicenter study. Journal of Interventional Cardiac Electrophysiology, 43, 217–226.
Shea, S., & Di Tullio, M. D. M. (2014). Atrial fibrillation, silent cerebral ischemia, and cognitive function. Journal of the American College of Cardiology, 62, 1998–1999.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Human rights statements and informed consent: All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000(5). Informed consent was obtained from all patients for being included in this study.
Additional information
P. Müller and P. Halbfass contributed equally to this work and share first authorship.
Rights and permissions
About this article
Cite this article
Müller, P., Halbfass, P., Szöllösi, A. et al. Impact of periprocedural anticoagulation strategy on the incidence of new-onset silent cerebral events after radiofrequency catheter ablation of atrial fibrillation. J Interv Card Electrophysiol 46, 203–211 (2016). https://doi.org/10.1007/s10840-016-0117-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10840-016-0117-6